Case Report - (2019) Volume 7, Issue 1
A 60-year-old Female with Acute Bilateral Lower Limbs Plegia, Low Back Pain and Discoordinated Neurological Examinations
Seyed Reza Habibzadeh1, Ehsan Bolvardi1, Elnaz Vafadar Moradi1, Esmaeil Raeyat Doost2 and Mahdi Foroughian1*
*Correspondence: Mahdi Foroughian, Department of Emergency Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran, Email:
Abstract
Classification of the spinal cord tumors varies depending on their placement in the spinal cord and their relationship with meninges. This case presenting to the Emergency Department with severe low back pain and acute progressive bilateral lower limbs plegia, in her clinical and neurological examinations both upper and lower motor neuron lesions founded. Spinal MRI of patient showed an extramedullary intradural mass posterior to T9-T12 vertebral bodies, which was highly suggestive for meningioma and a central bulging of lower discs that could cause mild pressure on the thec al sac. These combinations of pathology causes upper and lower motor symptoms for our patient.
<Keywords
Meningioma, Upper motor neuron, Lower motor neuron
Introduction
Spinal cord lesions and their neurologic examinations are important in determining the origin of them. Meningioma in spinal cord can make upper and lower motor neuron symptoms. In this case we discuss a patient with upper and lower motor neuron symptoms with extramedullary intradural mass that highly suggestive for meningioma.
Case Study
A 60-year-old female presented to our center with severe weakness, low back pain, and acute progressive bilateral plegia in her lower limbs. She was admitted to a hospital with these complaints in a small province three days ago, where the primitive treatment and diagnostic management obtained no acceptable results. Therefore, the patient was referred to our emergency center. During admission, she was awake and alert and there was no sign of illness or toxicity. However, she complained of lumbosacral pain and had no ability to move her lower limbs. In a review of her medical files, diabetes mellitus, hypertension and a non-documented history of lumbar disk protrusion were detected. She used no drugs and denied addiction, smoking, and alcohol consumption. The vital signs were measured as: BP: 170/95 mmHg, PR: 82/ min, RR: 18/min, T: 36.8 C (axillary), SO2: 98% (in room air), and BS: 209 mg/dl.
The head and neck survey were normal since the neck was supple. In addition, there was no jugular vein distension, and the movements of eyes were within normal limits (normal visual fields & acuity). Both pupils were normal in size and reaction, and she had a responsive gag reflex. In the cardiovascular system, there was a regular rate and rhythm without murmurs, gallops, or rubs. In the respiratory system, the patient had normal bilateral lung auscultation, and her abdomen was soft with no tenderness or distention. However, the bowel sounds were diminished. We detected signs of urinary retention (as a vesical globe) in the palpation of hypogastrium, and the tone of sphincter was normal in the rectal examination. Meanwhile, the anal skin touch sensorium was deranged. In addition, there was no occult blood, and the bulbocavernosus reflex was patent. In the extremities, the upper and lower limbs were warm and perfect, and peripheral perfusion was detected with no clinical findings of cyanosis, clubbing or edema. Moreover, all pulses and capillaries fillings were normal in both upper and lower extremities. In neurological examinations, the patient was alert and oriented to time, place and other people. The neurological exams of the upper limbs were normal in movements, sensation, muscle strength and reflexes. In lower limbs, muscle strength was diminished bilaterally (1/5), both lower limbs were flaccid, and a defined sensory loss was detected lower the hypogastrium. Therefore, the patient had no pain, and vibration and temperature sensorium are lost in these limbs bilaterally. The most interesting findings were detected in asymmetrical neurologic reflexes of the lower limbs of the case, where an increase was observed in the patellar reflexes in the right lower limb. Nonetheless, these exams were flat and undetectable on the other side (left lower limbs). Other cranial nerves examinations and equilibrium tests (e.g., nose to finger test), were within the normal limits. The 12 leads-ECG was obtained, and the rate, rhythm and other parameters were within the normal limits.
Laboratory results were remarkable for leukocytosis (17.7 × 103), other results are as follows:
BS: 144 mg/dl; UREA: 138 mg/dl; Cr: 5.6 mg/dl; Hb: 15.3 g/dl; Hct: 44.6%; Plt: 219 × 103
In bedside sonography, obvious evidence of urinary retention was detected. Furthermore, the lumbosacral Xray was taken and there were no acute pathologic findings, except for osteoarthritis in the lumbosacral spine (Figure 1). In addition, the axial head CT showed no acute cerebral pathology, mass or midline shifting (Figure 2).
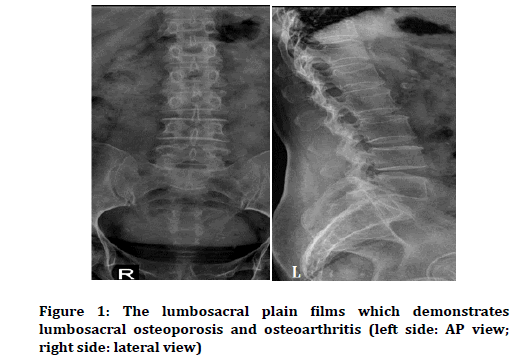
Figure 1. The lumbosacral plain films which demonstrates lumbosacral osteoporosis and osteoarthritis (left side: AP view; right side: lateral view)
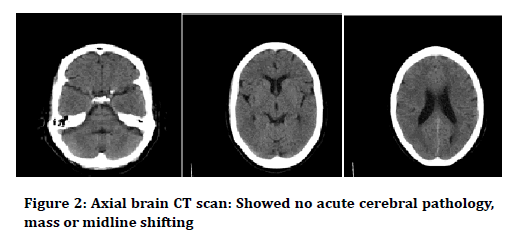
Figure 2. Axial brain CT scan showed no acute cerebral pathology, mass or midline shifting.
According to the history and clinical exams, lumbosacral MRI with contrast was performed due to a lack of confirmed intra or extrathecal lesions (Figure 3). In MRI, we found dehydration of all lumbar discs, and central bulging of the lumbar disk with mild pressure on thecal sac was noted. An extramedullary intradural mass was observed posterior to T9-T12 vertebral bodies, which was highly suggestive for meningioma. After GD injection, mild heterogeneous enhancement of the mass was observed. The patient was referred to a neurosurgeon and underwent a mass dissection surgery. She was discharged after recovery. The pathological report confirmed that the mass was a meningioma.
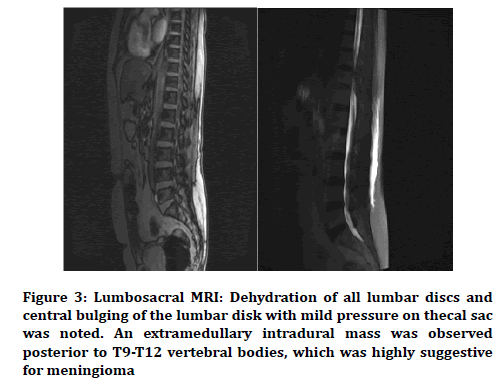
Figure 3. Lumbosacral MRI: Dehydration of all lumbar discs and central bulging of the lumbar disk with mild pressure on thecal sac was noted. An extramedullary intradural mass was observed posterior to T9-T12 vertebral bodies, which was highly suggestive for meningioma
Discussion
Classification of the spinal cord tumors varies depending on their placement in the spinal cord and their relationship with meninges. Therefore, the spinal cord tumors can be placed outside the meninges and the spinal cord, inside the meninges and outside the spinal cord or inside the meninges and inside the spinal cord.
The occurrence of spinal cord tumors, regardless of their initial or metastatic nature, results in different neurological symptoms due to compressive effects on the spinal cord and reaching the spinal cord paths. These symptoms vary depending on the size and location of the tumor in the spinal cord. While only 1% of all malignancy returns to the spinal cord tumors, approximately 4%-10% of the central nervous system malignancies are spinal cord tumors [1]. It should be noted that many of the spinal masses are metastatic and about 10% of patients with known malignancies experience a tumor reaching their spinal cord during the disease course [2]. More than half of the cases of metastasis to the spinal cord occur due to the lung, breast, and lymphatic malignancies, whether direct or through the blood system. Most metastases occur at the level of the thoracic spine [3]. In terms of clinical symptoms, many spinal cord tumors exhibit vague pain [4], and severe pain in the waist area, which intensifies at night, can be a sign of a possible spinal cord tumor [5]. It is notable that in this case, an attempt to increase the pressure inside the spinal cord for any reason, such as sneezing or coughing, exacerbated pain. The nerve exam in these patients varies depending on the level and extent of the spinal cord injury and might be different from full spinal cord syndrome to the anterior spinal cord syndrome or the central spinal cord syndrome [1]. In many of these patients, a simple spinal cord graph is the primary diagnostic key. Undoubtedly, in cases where suspicious issues appear in the simple graph or the patient has a suspicious neurological examination, more diagnostic measures, such as MRI, are required for the patient despite the seemingly natural initial gradient [6,7]. In the diagnosis of important differential divisions of the spinal cord, full attention must be paid to the hematomas, spinal cord infections, as well as infarction and transverse myelitis [1]. Myelopathy caused by acute pressure on the spinal cord as a result of a mass is a real medical emergency [1]. The speed of operation to manage these patients is necessary because if paraplegia and urinary incontinence occur, less than 5% of patients will return to their normal state [8-10]. Consultation with a neurologist, oncologist and radiologist is required to start coronary therapy, radiotherapy or emergency surgery for optimal management of these patients [1].
Conclusion
Our case was a 60-year-old female presenting to the center due to severe low back pain and acute progressive bilateral lower limbs plegia. The patient was an interesting case because her clinical and neurological examinations demonstrated both upper and lower motor neuron lesions, increased reflexes and Babinski’s response presentation in the right side due to meningioma, which was lower in the opposite side. In addition, there was an absence of reflexes due to primitive herniation of the lumbar disk. The patient had an obvious sensory level that corresponded to a compression on the anterior spinal cord. However, her anal sphincter tone was normal, and urinary retention was detected in this patient. The composition of these clinical findings provided vague data, which led us to perform an imaging to determine the lesions in multiple levels. We found an extramedullary intradural mass posterior to T9-T12 vertebral bodies, which was highly suggestive for meningioma and a central bulging of lower discs that could cause mild pressure on the thecal sac. Finally, we concluded that clinical and neurologic examinations are important in determining the origin of spinal cord lesions. In this regard, paying attention to diseases can produce multi-level symptoms in conditions that we have, and some upper motor neuron symptoms beside lower motor neuron findings.
References
- Marx J, Hockberger R. Rosens emergency medicine, concepts and clinical practice. 2014; 106:1426.
- Traul DE, Shaffrey ME, Schiff D.: Spinal cord intradural neoplasms. Lancet Oncol 2007; 8:35.
- Ruckdeschel JC. Early detection and treatment of spinal cord compression. Oncology 2005; 19:81.
- Schiff D, O’Neill BP, Suman VJ. Spinal epidural metastasis as the initial manifestation of malignancy: Clinical features and diagnostic approach. Neurology 1997; 49:452-80.
- Jansson KA, Bauer HC. Survival, complications, and outcome in 282 patients operated for neurological deficit due to thoracic or lumbar spinal metastases. Eur Spine J 2006; 15:196.
- Abdu WA, Provencher M. Primary bone and metastatic tumors of the cervical spine. Spine 1998; 23:2767-82.
- Husband DJ, Grant KA, Romaniuk CS. MRI in the diagnosis and treatment of suspected malignant spinal cord compression. Br J Radiol 2001; 74:15-83.
- Sciubba DM, Gokaslan ZL. Diagnosis and management of metastatic spine disease. Surg Oncol 2006; 15:141.
- Schiff D. Spinal cord compression. Neurol Clin 2003; 21:67.
- Wagner R, Jagoda A. Spinal cord syndromes. Emerg Med Clin North Am 1997; 15:699.
Author Info
Seyed Reza Habibzadeh1, Ehsan Bolvardi1, Elnaz Vafadar Moradi1, Esmaeil Raeyat Doost2 and Mahdi Foroughian1*
1Department of Emergency Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran2Department of Emergency Medicine, Faculty of Medicine, Jahrom University of Medical Sciences, Jahrom, Iran
Citation: Seyed Reza Habibzadeh, Ehsan Bolvardi, Elnaz Vafadar Moradi, Esmaeil Raeyat Doost, Mahdi Foroughian, A 60-year-old female with acute bilateral lower limbs plegia, low back pain and discoordinated neurological examinations, J Res Med Dent Sci, 2019, 7(1): 77-79.
Received: 27-Dec-2018 Accepted: 05-Jan-2019
