Case Report - (2022) Volume 10, Issue 1
A Case of Mismanaged Supracondylar Fracture of Humerus in a 48 Year Old Man: Case Report
Kailasnath MS*, Vijay Narasimman Reddy and Lionel John
*Correspondence: Kailasnath MS, Department of Orthopaedics, Sree Balaji Medical College and Hospital, Chromepet, Chennai, Tamilnadu, India, Email:
Abstract
Background: The most common type of fracture around the elbow in children and adolescents is a supracondylar humeral fracture. It is rarely seen in adults and is difficult to manage. Here is a case report a case of a 48 year old male patient who presented to our outpatient department with a 4 months old supracondylar humerus fracture of the right side managed successfully with dual plating without any complications and need for further interventions. Case presentation: A 48 year old male patient presented to our department with complaints of swelling, deformity and difficulty to move his right elbow for a period of 4 months after a history of a road traffic accident. He has been taking native treatment for 4 months before presenting to our institute. A supracondylar fracture of the right humerus was diagnosed based on the plain radiograph and CT scan. An open reduction and internal fixation of the right humerus was performed successfully with dual plating and the deformity was corrected. His other complaints were also addressed with the procedure. There was a satisfactory improvement in function and range of motion after a follow up period of 6 months. Conclusion: The surgical management by internal fixation with dual plating can show promising results in the management of supracondylar humerus fracture in adults. This management modality can be considered for a satisfactory function, range of joint motion and correction of deformity without any post-operative complications.
Keywords
Supracondylar fracture humerus, Dual plating
Introduction
Mismanagement of fractures is a commonly seen among rural population. In most cases such fractures are either neglected or the patients sort to native treatment was condition is poorly managed leading to poor or loss of function of the affected upper extremity. Native treatment is accepted among general public of rural population as it is less expensive which often does not involve radiological investigations and is completely oriented to non-operative treatment which involves splints and herbal medications. Fractures that are improperly treated for more than a few weeks allow nerves, muscles and arteries to contract, which can lead to disuse osteopenia. Supracondylar fracture of humerus in adults is very rarely encountered which can result is residual deformity, joint stiffness and poor function which affects daily activities. We came across a case of old supracondylar fracture of humerus which was managed surgically with dual plating.
Case Report
A 48 year old male patient came to our OPD with a history of road traffic accident 4 months back where he sustained injury to his rightt elbow. He had pain, swelling and inability to move his right elbow after the trauma.
He was taken to a native practitioner by his relatives were he was managed by splinting with herbal medications of the affected limb for a period of 2 months. After the splints were removed he noticed deformity over his right elbow with restricted movement and functional loss. 2 months after the removal of native splints he came to us for further management. He was examined clinically. He had no pain or any local skin changes. Deformity over his right elbow with an abnormal mobility was noted. It was non tender with restricted movement of the right elbow joint. Neurovascular status of his right upper limb appeared to be normal with no sensory loss or signs of ischemia. A plain radiograph and CT Scan of the right elbow was taken which showed a supracondylar humerus fracture which appeared to be of Type 3 according to Gartland Classification. X ray of the forearm of the same side showed a distal ulnar fracture. He was managed by an open reduction with dual plating of distal part of the humerus. Fracture was successfully reduced using posteromedial and lateral plating under a Posterior Approach. Post-operative period was uneventful. There were no signs of any neurovascular compromise. He was discharged on 14th day after surgery. Active range of movement exercises were initiated at 6 weeks. He was followed up after 4 weeks, 3 months and 6 months following discharge. There was a significant improvement in his symptoms and function with satisfactory range of movements on every follow up (Figure 1).
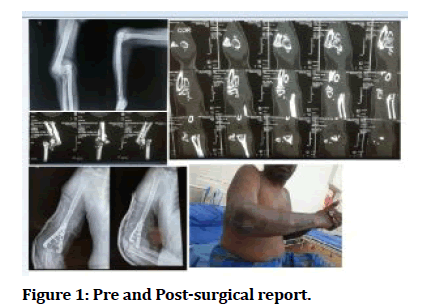
Figure 1: Pre and Post-surgical report.
Discussion
Supracondylar fracture of humerus in adults is a condition which we rarely come across in daily orthopaedic trauma. It is seen most frequently in children between 3 to 10 years of age [1]. A potential for developing neurovascular complications and higher incidence of residual deformity make supracondylar fracture of humerus a serious injury. The medial column along with the lateral column attaches the articulating surfaces present in the distal humerus to the humerus shaft2. A thin area of the bone present in the distal humerus separates medial column from the lateral column. The coronoid fossa is located anteriorly and olecranon fossa is located posteriorly in this area [2]. This part of the bone acts as a weak link in the distal humeral architecture. This part of the bone is responsible for the origin of the supracondylar fractures [2].The pattern of the supracondylar fractures is transverse in majority of the cases and it occurs in the region of olecranon fossa and it does alter with the mechanism of flexion force or extension force. The pattern of fracture seen in older patients is usually oblique rather than transverse pattern which is seen in children2. The exact reason is unknown. The rotation force results in an angulation additionally leading to instability in oblique type compared to the latter type. Extension type accounts for majority of the supracondylar fractures. About 94% to 97% of all supracondylar fractures are of extension type. The rarest type is a flexion type which comprises of only 3% to 6% of fractures reported.
Initially supracondylar humeral fractures are classified into flexion or extension type of injuries and then it is classified based on the degree of displacement radiographically. In 1959 Gartland introduced a classification system for supracondylar fracture of humerus [3]. It is a 3part classification system. Type 1 fractures are non-displaced or fractures with minimal displacement. Fractures with distal fragment having an angulation with one intact cortex formed type 2. Type 3 fractures formed with fractures of both cortices with complete displacement. Our present case can be classified into Type 3 according to Gartland classification. Reporting of diagnosis of a case of supracondylar fractures it land one in a diagnostic dilemma. It is either very evidently presents or it is very difficult to diagnose. In some cases it is very difficult to differentiate between a supracondylar fracture and an intercondylar fracture. In cases of fractures with severe displacement, to diagnose clinically is not much of a task but one may find difficulty in ruling out injuries associated with supracondylar fracture especially injuries to the neurovascular structures. The examiner should be cautious while examining for possible associated injuries and it should be done without fail. Various literatures have reported the incidence of various associated injuries especially the presence of other fractures in the ipsilateral limb especially fracture of distal radius (5%). 10% to 15% of cases have associated neurological injury [4,5]. The main aim of the management of supracondylar humeral fractures is to avoid short term complications like compartment syndrome, associated vascular injuries and minimize embarrassments like iatrogenic nerve palsies and cubitus varus deformity [5,6].
Conclusion
Management of an old supracondylar fracture is a challenge considering the intraoperative neurovascular injuries, post-operative rehabilitation and chance of residual deformities. The surgical management in this case by internal fixation with dual plating has shown satisfactory improvement in limb function, range of joint motion on every follow ups with no residual deformity without any commonly encountered post-operative complications. Dual plating provides various choices for screw positioning and it supports bilaterally leading to excellent compression of the fixation thereby imparting successful anatomical reduction.
Conflict of Interests
None.
References
- Robinson CM, Hill RM, Jacobs N, et al. Adult distal humeral metaphyseal fractures: Epidemiology and results of treatment. J Orthop Trauma 2003; 17:38-47.
- Korner J, Lill H, Müller LP, et al. Distal humerus fractures in elderly patients: Results after open reduction and internal fixation. Osteoporos Int 2005; 16:S73-9.
- Nauth A, McKee MD, Ristevski B, et al. Distal humeral fractures in adults. J Bone Joiunt Surg 2011; 93:686-700.
- Gofton WT, MacDermid JC, Patterson SD, et al. Functional outcome of AO type C distal humeral fractures. J Hand Surg 2003; 28:294-308.
- Prasarn ML, Ahn J, Paul O, et al. Dual plating for fractures of the distal third of the humeral shaft. J Orthop Trauma 2011; 25:57-63.
- Ali N, Mir NA, Dar TA, et al. Outcome of extra-articular distal humerus fractures fixed by single column extra-articular distal humerus locking compression plate using triceps sparing postero-lateral approach. Bulletin Emergency Trauma 2018; 6:306. Indexed at, Google Scholar
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Kailasnath MS*, Vijay Narasimman Reddy and Lionel John
Department of Orthopaedics, Sree Balaji Medical College and Hospital, Chromepet, Chennai, Tamilnadu, IndiaReceived: 14-Dec-2021, Manuscript No. Jrmds-22-49830; , Pre QC No. Jrmds-22-49830 (PQ); Editor assigned: 16-Dec-2021, Pre QC No. Jrmds-22-49830 (PQ); Reviewed: 30-Dec-2021, QC No. Jrmds-22-49830; Revised: 04-Jan-2022, Manuscript No. Jrmds-22-49830 (R); Published: 11-Jan-2022
