Research Article - (2025) Volume 13, Issue 6
A Comparative Evaluation of Two Different Techniques for Esthetic Management of Gingival Melanin Hyperpigmentation: A Clinical Study
*Correspondence: Hatim Barrak A. AlOsaimi, Department of Restorative Dentistry, Prince Sattam Bin Abdulaziz University, Al-Kharj, Saudi Arabia, Email:
Abstract
Introduction: The colour of gingiva influences the smile of person, hence the objective of this study was to evaluate the effect of gingival depigmentation by scalpel and electro-surgery on patient’s response, healing and recurrence of pigmentation.
Materials and methods: A total number of 18 patients, 16 males and 2 females aged between 18 to 30 years, reported to the clinic, college of dentistry, Prince Sattam Bin Abdul Aziz University, Alkharj, with the common chief complain of “grayish blackish gums” which affected the aesthetics of their smile. The techniques followed in the present study were the scalpel surgical technique and electrocautary as these consumed less time and could be carried out easily. Patients were recalled post-operatively to evaluate healing and recurrence of pigmentation. Intraoral pictures were taken at every follow-up visit to compare the progress and also to access the occurrence of any repigmentation. One way ANOVA and unpaired t-test was used for statistical analysis.
Results: The results achieved for all the patients were satisfactory and pleasant. No post-operative complications like pain, infection, bleeding nor scarring was observed during the follow up visits. The patients were recalled for a follow-up up to a period of 6 months for scalpel depigmentation cases and 6 months for electrosurgical cases. There were no signs of repigmentation and the patients are being monitored longitudinally for any reoccurrences of pigmentation.
Conclusion: Both the surgical and electrocautary procedures for gingival depigmentation were successful and our patients were satisfied with the results achieved. Hence we conclude that surgical technique still serves as the simplest and effective depigmentation technique. During the follow-up period, no recurrence of gingival hyper-pigmentation was found with both the techniques employed in this study.
Keywords
Depigmentation, Electrocautary, Gingival melanin hyperpigmentation, Scalpel
Introduction
Smile is considered as one of the most powerful emotion to connect and socialize. Two main factors that can affect a confident smile is teeth and the gums. Hence other than the position of teeth, the color of the teeth, gingival color and health also plays an important role in making a smile attractive. The natural and acceptable color of the gingiva is usually coral pink. There are several factors which is responsible for the color they include the number and size of blood vessels, thickness of the epithelium, degree of keratinisation and the colored pigments within the epithelium [1].
Gingiva happens to be the most pigmented tissue in the mucosa and most predominant natural pigment responsible for this appearance of the gingiva is a brown pigment called melanin. Melanoblasts cells present in the gingival epithelium produces melanin granules which results in melanin pigmentation [2].
The variation in the degree of gingival hyperpigmentation among different populations is considered physiological or racial pigmentation and it is not related to the gender or age hence it can be seen as a racial trait [1,3]. Since the pigmentation is related to the melanoblastic activity, its degree differs from person to person [4].
Usually the occurrence of gingival pigmentation is persistent and symmetrical without causing any alteration of the gingival structure. Dark skinned ethnic populations are more prone for melanosis of gingiva, it is mostly observed in African and east Asian [5,6]. Gingival pigmentation also increases in certain medical conditions such as Addison’s syndrome or Addisons disease [7].
Literature search reports numerous techniques to treat depigmentation and to enhance esthetics. This study was conducted to evaluate the effect of gingival depigmentation by scalpel and electro-surgery on patient’s response, healing and recurrence of pigmentation.
Materials and Methods
The clinical trial was conducted among 18 patients (16 males and 2 females) aged 18 to 30 years who reported to the clinic, College of Dentistry, Prince Sattam Bin Abdul Aziz University, Al-kharj, with the chief complain of “grayish-blackish gums” which affected the aesthetics of their smile.
A detailed medical history about systemic diseases and medications related to the gingival melanin pigmentation were taken. Patients with acute pulpal or periodontal pain and abscesses were excluded from the study. Oral hygiene instructions were given to the patients and oral prophylaxis was carried out as a part of the first phase of the periodontal treatment. Once the gingival inflammation had subsided completely the patients were scheduled for the depigmentation procedure.
Written informed consent was obtained from all patients, and ethical clearance for the study was obtained from the Institutional Ethical Committee (IEC).
The selected subjects were divided into two groups randomly.
• Group I: Depigmentation using surgical blade technique.
• Group II: Depigmentation using electrocautery technique.
Gingival melanin pigmentation assessment preoperatively and postoperatively was made according to Dummett Gupta oral pigmentation index scoring criteria given by Dummett C.O. in 1964 [8]:
• 0-No clinical pigmentation (pink gingiva).
• 1-Mild clinical pigmentation (mild light brown color).
• 2-Moderate clinical pigmentation (medium brown or mixed pink and brown color).
• 3-Heavy clinical pigmentation (deep brown or bluish black color).
Observations were made in natural light. The observations were made by two investigators and a consensus score was assigned to the degree of hyperpigmentation.
Surgical blade technique (Group I)
Surgical gingival de-epithelization procedure was planned using the scalpel technique, following the administration of a local anesthetic solution, blade no.15 with bard parker handle was used to scrape the epithelium carefully with underlying pigmented layer from 1st premolar to 1st premolar for both the arches. The raw surface was irrigated with saline solution. A pressure pack was placed using sterile gauze to control the bleeding. Care was taken that excessive tissue was not removed thereby avoiding any bone exposure. Once the procedure was completed a periodontal pack was placed at the surgical site and proper post-operative instructions were given to the patients in the language they could comprehend. Pain management was done by prescribing analgesics and the patients were recalled after a week.
Group I: Gingival depigmentation by surgical blade (Figures 1-3).
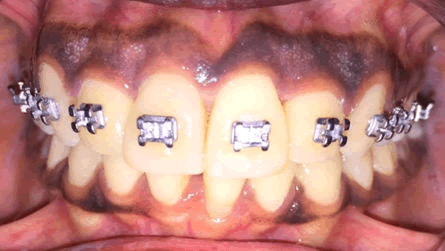
Figure 1: Pre-operative.
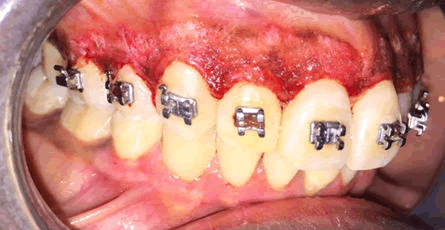
Figure 2: After de-epithialization.

Figure 3: 6 months post-operative.
Electrosurgical gingival depigmentation (Group II)
Gingival de-epithelization procedure was planned using electrocautary unit to de-epithelize the hyperpigmented areas. Ablation of the effected tissues was carried out by means of loop electrode of the electrocautery unit under standard protective measures. Great caution was exercised while using the tip and prolonged contact with one area can lead to tissue damage due to excessive heat, hence the tip should constantly be in motion and used only in light brushing strokes. Sterile gauze soaked in saline was used to remove the abscised tissue fragments. This was continued until the desired amount of pigmented tissue was ablated which can be easily achieved without any bleeding. On completion a periodontal pack was placed on the surgical site and proper post-operative instructions were given in the patient’s language.
Group II: Gingival depigmentation by electrocautery (Figures 4-8).
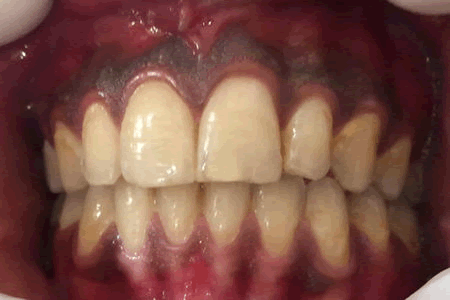
Figure 4: Pre-operative.
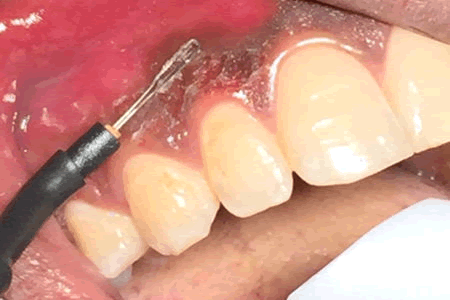
Figure 5: Loop electrode.
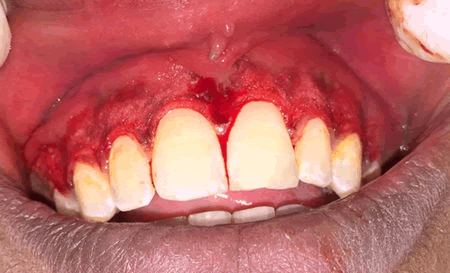
Figure 6: After de-epitheliazation.

Figure 7: Periodontal pack.

Figure 8: 6 months post-operative.
Post-operative care
Analgesics were prescribed for pain management and the periodontal dressings were removed after 1 week postoperatively. Patients were recalled at 7, 15 and 21 days postoperatively to observe healing and to assess the level of patient comfort following the procedure.
Re-evaluation of the clinical parameters
The degree of gingival depigmentation and recurrence of gingival melanin pigmentation and its intensity were recorded on completion of the first month, and 6 months postoperatively.
Statistical analysis
Descriptive data are presented as mean and standard deviations. Unpaired t-test was used to assess the difference between the groups in relation to the degree of depigmentation and the extent of re-pigmentation. One-way ANOVA was used for the intra-group comparison followed by Tukey’s post hoc test for pairwise comparisons.
Results
The results achieved for all the patients were satisfactory and pleasant. No post-operative complications like pain, infection, bleeding nor scarring was observed during the follow up visits. The patients were recalled for a follow up up to a period of 6 months for scalpel depigmentation cases and 6 months for electrosurgical cases. There were no signs of repigmentation and the patients are being monitored longitudinally for any reoccurrences of pigmentation.
Table 1 shows the intragroup comparison of the mean Dummett-Gupta oral pigmentation index score at baseline, 1 month and 6 months. It can be observed that there was statistically significant reduction seen for both the study techniques 6 months postoperatively as compared to baseline.
| Study group | Electrosurgical | Surgical blade | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Baseline | 3 | 0 | 3 | 0 |
| 1 month | 1 | 0 | 1 | 0 |
| 6 months | 1.45 | 0.522 | 1.3 | 0.483 |
| ANOVA | 133 | 149.571 | ||
| P value | 0 | 0 | ||
Table 1: Intragroup comparison of the mean Dummett-Gupta oral pigmentation index score at baseline, 1 month and 6 months.
Table 2 shows the comparison of the mean Dummett Gupta Oral Pigmentation Index score at baseline, 1 month and 6 months. It can be observed that there was no statistically significant difference seen between the two study techniques 6 months postoperatively.
|
Study group |
Mean score |
STD. dev. |
T test |
P value |
Baseline |
Electrosurgical |
3 |
0 |
- |
- |
Surgical blade |
3 |
0 |
|||
1 month |
Electrosurgical |
1 |
0 |
- |
- |
Surgical blade |
1 |
0 |
|||
6 months |
Electrosurgical |
1.45 |
0.522 |
0.702 |
0.491 |
Surgical blade |
1.3 |
0.483 |
Table 2: Comparison of the mean Dummett-Gupta oral pigmentation index score.
Discussion
Gingival hyperpigmentation is the cause for esthetic concern for many patients. Literature search reports numerous techniques to treat depigmentation and to enhance esthetics.
Surgical blade de-epithelization is an effective technique which is simpler and more economical than most of the available techniques [9]. Electrosurgery is another commonly used technique for effective depigmentation but it requires more expertise and prolonged application of electrical current can cause tissue destruction. This study was thus undertaken to compare these two techniques for esthetic management of gingival melanin hyperpigmentation.
The anterior sextant being the most esthetically noticeable region in the oral cavity was chosen for the study and gingival depigmentation is essentially undertaken to satisfy the esthetic needs of the patients. It has been shown that anterior attached gingivais more pigmented than the posterior as it is more exposed to light [10]. It has been observed that after the initial reduction in pigmentation mean score after the procedure, the rate and intensity of re-pigmentation was more in the anterior sextant than the posterior sextant [11]. This difference has been attributed to the effect of sunlight on the anterior segment.
A comparison between group I and group II showed no statistically significant difference in the degree of depigmentation. The efficacy of surgical blade technique and electrocautery has been demonstrated in several previous studies. In a case series, split mouth de epithelization procedure using scalpel, bur abrasion and electrosurgery were successfully used to treat gingival hyperpigmentation. It was reported that electrosurgery required a lot of precision but increased the efficacy of work, giving a cleaner and neater work field. Scalpel de epithelization was reported to be easier and gave excellent results and patient satisfaction [9].
In another case series it was found that scraping, electrosurgery, and diode laser were simple, effective, and yielded good results, along with good patient satisfaction [12].
The repigmentation was assessed at the end of 1 month and at the end of 6 months. Repigmentation refers to the clinical reappearance of melanin pigment following a period of clinical depigmentation. The mechanism suggested for the spontaneous repigmentation is that the melanocytes from the normal skin proliferate and migrate into the depigmented areas [13]. A study by Perlmutter et al., showed that gingival surgical procedures performed solely for cosmetic reasons offer no permanent results [4]. Ginwalla, et al. reported repigmentation in 50% of their cases between 24 and 55 days [14]. A case series by Prasad D, et al. had shown thatbur abrasion, scraping, partial thickness flap cryotherapy and electrosurgery for depigmentation were simple, effective and yielded good results, along with good patient satisfaction [15]. This study is limited by the number of subjects. Also, consideration was not given to the patient’s complexion with regard to the degree of pigmentation and the rate of repigmentation. In spite of the limitations, it can be inferred from the study that both scalpel technique as well as electrocautery can be successfully used in the treatment of unaesthetic gingival pigmentation.
Conclusion
Both the surgical and electrocautary procedures for gingival depigmentation were successful and our patients were satisfied with the results achieved. Hence we conclude that surgical technique still serves as the simplest and effective depigmentation technique. During the follow-up period, no recurrence of gingival hyperpigmentation was found with both the techniques employed in this study.
References
- Dummett CO. First symposium of oral pigmentation. J Periodontol 1960; 31:356–360.
- Cicek Y, Ertas U. The normal and pathological pigmentation of oral mucous membrane: A review. J Contemp Dent Pract 2003; 4:76–86.
[Google Scholar] [PubMed]
- Dummet CO, Barens G. Oromucosal pigmentation: An updated literary review. J Periodontol 1971; 42:726–736.
[Crossref] [Google Scholar] [PubMed]
- Perlmutter S, Tal H. Repigmentation of gingival following injury. J Periodontal 1986; 57:48–50.
[Crossref] [Google Scholar] [PubMed]
- Fry L, Almeyda JR. The incidence of buccal pigmentation in cauacasoids and negroids in Britain. Br J Dermatol 1968; 80:244-247.
[Crossref] [Google Scholar] [PubMed]
- Tamizi M, Taheri M. Treatment of severe physiologic gingival pigmentation with free gingival autograft. Quintessence Int 1996; 27:555-558.
[Google Scholar] [PubMed]
- Almas K, Sadiq W. Surgical Treatment of Melanin-Pigmented Gingiva: An Esthetic Approach. Indian J Dent Res 2002; 13:70–73.
[Google Scholar] [PubMed]
- Dummett CO,Gupta OP. Estimating the epidemiology of the oral pigmentation. J Natl Med Assoc 1964; 56:419-420.
[Google Scholar] [PubMed]
- Kathariya R, Pradeep A R. Split mouth de-epithelization techniques for gingival depigmentation: A case series and review of literature. J Indian Soc Periodontol 2011; 15:161-168.
[Crossref] [Google Scholar] [PubMed]
- Raut RB, Baretto MA, Mehta FS, et al. Gingival pigmentation: Its incidence amongst the Indian adults. JAIDA 1954; 26:9-10.
- Kaur H, Jain S, Sharma R L. Duration of reappearance of gingival melanin pigmentation after surgical removal-A clinical study. J Indian Soc Periodontol 2010; 14:101-105.
[Crossref] [Google Scholar] [PubMed]
- Thangavelu A, Elavarasu S, Jayapalan P. Pink esthetics in periodontics – Gingival depigmentation: A case series. J Pharm Bioallied Sci 2012; 4:S186–S190.
[Crossref] [Google Scholar] [PubMed]
- Sucheta A, Prasad R, Laksmi P, et al. Depigmentation: To beautify a smile. Ann Dent Res 2014; 3:52-94.
- Ginwalla TM, Gomes BC, Varma BR. Surgical removal of gingival pigmentation. J Indian Dent Assoc 1966; 38:147-150.
[Google Scholar] [PubMed]
- Prasad D, Sunil S, Mishra R, et al. Treatment of gingival pigmentation: A case series. Indian J Dent Res 2005; 16:171-176.
[Crossref] [Google Scholar] [PubMed]
Author Info
Department of Restorative Dentistry, Prince Sattam Bin Abdulaziz University, Al-Kharj, Saudi ArabiaCitation: Hatim Barrak A. AlOsaimi, A Comparative Evaluation of Two Different Techniques for Esthetic Management of Gingival Melanin Hyperpigmentation: A Clinical Study, J Res Med Dent Sci, 2025, 13 (01): 037-042.
Received: 01-Dec-2023, Manuscript No. JRMDS-23-129606; , Pre QC No. JRMDS-23-129606; Editor assigned: 04-Dec-2023, Pre QC No. JRMDS-23-129606; Reviewed: 18-Dec-2023, QC No. JRMDS-23-129606; Revised: 22-Jan-2025, Manuscript No. JRMDS-23-129606; Published: 29-Jan-2025
