Research - (2022) Volume 10, Issue 1
A Complete Check on the Soft Tissue and Hard Tissue of Patients Undergoing Socket Preservation-A Retrospective Hospital Based Analysis
Akhil Ashref1, Subhasree R2*, Thiyaneswaran N3, Dimple Rani1, Rajendra Prabhu Abhinav1 and Priyalochana G1
*Correspondence: Subhasree R, Deaprtment of Prosthodontics, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical science, Saveetha University, Chennai, India, Email:
Abstract
The aim of this retrospective study is to evaluate the preoperative and postoperative bone dimension and soft tissue change in patients undergoing socket preservation in a private dental hospital setup. A retrospective study was done in which 152 patients who underwent socket preservation from 1 September 2019 till 1 March 2020 were included. Data was reviewed from the patient’s records and analysed the data of 152 from June 2019 and March 2020 that were documented in a private institution. The data censored was collected by recalling the patient and reviewing. A retrospective study was done to identify the patients that underwent socket preservation procedure in a private hospital dental set up and the difference in bone gain attained was evaluated from pre and post cbcts and wound healing and primary stability, suturing technique used was also evaluated. Statistical analysis was performed using the Paired t test to assess the difference between the pre and post bone volume. Mean pre and post height and width was seen in post socket preservation was 0.47 ± 0.52, 0.35 ± 0.39 respectively. The association between the wound healing and suture technique; primary stability and the graft used was significant. Bio-os showed marked difference when compared to other graft material used. Within the limitations of the study, there was a statistical significant difference between the pre and post CBCT for the patient who underwent socket preservation. There was better healing with patients who had thick gingival biotype and when simple interrupted sutures were given. The primary stability of the site was more when grafted with Bio-oss.
Keywords
Socket Preservation, Dental implants, Soft tissue healing, Suturing technique, Grafting
Introduction
Radiographic imaging is a preliminary and essential step in the diagnosis, treatment planning, and follow-up cases in implant dentistry [1].CBCT aids in the 3-dimensional assessment of alveolar structures. So, this study was performed to evaluate the bone gain during socket preservation using CBCT and consider factors like wound healing, primary stability achieved, and the gingival biotype [2]. The alveolar process is a tooth-dependent tissue that occurs in tandem with tooth eruption. The volume and shape of the alveolar process are dictated by the shape of teeth, their eruption axis, and eventual inclination. The buccal bone plates in both the maxilla and the mandible were resorbed much more than the corresponding palatal/lingual bone walls, causing the ridge's core to change palatally/lingually [3].
Socket preservation procedure is performed to preserve soft and hard tissue at the extraction site. The alveolar bone is a special kind of bone being a tooth-dependent entity; therefore, post-extraction bone loss happens at a higher pace in the first six months, which in turn results in the diminishing of 40% of the bone height of the alveolus, and 60% of the width [4]. Multiple pieces of evidence have confirmed that bone loss occurs post-extraction, and its incidence is more on the labial side of the alveolar process than that of the lingual or the palatal side [5]. It can be assumed that, as compared to tooth extraction alone, ARP is an efficient method for reducing the dimensional reduction of the alveolar ridge that occurs after tooth extraction. As a result, alveolar ridge preservation should be considered in combination with a minimally painful tooth extraction in clinical scenarios where reducing alveolar ridge reduction is a priority. In the apical and lateral parts of the extraction socket, large quantities of freshly developed bone occurred [6] the central and peripheral compartments of the experimental site housed provisional matrix tissue. No periodontal ligament tissue could be found lateral to the socket walls at this time. The crestal area of the bone walls revealed no bundle bones. Furthermore, the woven bone had replaced a significant portion of the lamellar bone in the crestal region of the buccal wall [4]. The freshly developed tissue's surface showed signs of remodelling.
Different grafting materials may affect the pattern of bone healing and the consistency of the bone in healed sockets [5]. Cortical and cancellous biomaterials also demonstrated Osteoconductive properties, though with different healing patterns. It has been discovered that cancellous bone recovers with initial bone formation accompanied by osteoclastic bone resorption, while cortical bone resorption occurs first. Some factors can influence dimensional changes after tooth extraction, such as flap rising during extraction, buccal plate thickness, or the presence of a single or multiple-rooted tooth. Socket preservation can avoid the necessity for bone augmentation at a later stage. By decreasing bone resorption and facilitating bone formation, it increases the implant success rate and survival chances. In preclinical models, the potential benefit of a flapless surgery during tooth extraction for limiting the resorptive phase of the alveolar crest was explored by contrasting the outcomes with a flapped traditional surgery. At the same time, some studies have shown that after flapless tooth extraction, bone remodelling of the alveolar ridge is slightly less pronounced; biomaterials for socket grafting including autograft, allograft, xenograft and alloplastic. A bone substitute that has a lesser substitution rate is recommended.
Materials and Methods
A retrospective study was done in a private institution, conducted over a six month period, i.e. from 1 September 2019 to 1 March 2020 and included 152 patients who had undergone socket preservation.
Inclusion criteria
Patients who underwent socket preservation and implant placement, Age within 25 to 50 years, males and females, Non-smokers and non-alcoholic.
Exclusion criteria
Any systemic disease, Multiple implant placement, Pterygoid or Zygomatic implant placement.
The data collected was entered, tabulated and analysed for the comparison of the level of implant placement with the associated marginal bone loss.
Statistical analysis was done using SPSS Statistics Software for windows, version 20.0. Chi-square test and Pearson’s correlation was done to determine that there is any statistically significant difference between the Pre and Postoperative height and after socket preservation, the association between gingival biotype and healing, suturing technique and healing, primary stability and the graft used.
Results
Out of 152 patients who underwent socket preservation, 75(49.3%) were males, and 77(50.7%) were females. The mean pre height and post height was 16.59 ∓ 3.89 and 16.12 ∓ 3.93, respectively (Table 1).
| Mean and SD (mm) | P value | |
|---|---|---|
| Pre Height | 16.59 ± 3.89 | 0 |
| Post Height | 16.12 ± 3.93 | |
| Pre Width | 6.96 ± 1.12 | 0 |
| Post Width | 6.61 ± 1.14 |
Table 1: Showing the pre and post height and width of the socket.
The association between the Suturing technique and wound healing, primary stability, and the graft used were statistically significant and was done using the Chi- Square test and Pearson correlation; the p-value was 0.000, proving that simple interrupted technique was better than horizontal mattress.
The association between the gingival biotype and wound healing was not statistically significant (p - 0.392); hence there is no difference in the wound healing between the thick and thin gingival biotype.
The association between the primary stability and bone graft used was also statistically significant using the Chi-Square test and Pearson correlation; the p-value was 0.000, proving that Bio-oss had better primary stability (>25Ncm) than Osseo graft used during the socket preservation (Table 2), (Figures 1-3).
| Wound Healing | df | Sig | |||
|---|---|---|---|---|---|
| Satisfactory | Not Satisfactory | ||||
| Gingival Biotype | Thick | 71 (55.5%) | 12 (50%) | 1 | 0 |
| Thin | 57 (44.5%) | 12 (50%) | |||
| Simple Interrupted | 111 (86.7%) | 12 (50%) | 1 | 0 | |
| Suturing Technique | Horizontal Mattress | 17 (13.3%) | 12 (50%) | ||
| Primary Stability | |||||
| <25 Ncm | > 25N | ||||
| Bone Graft | Bio-oss | 35 (33%) | 71(61%) | 1 | 0 |
| Osseo graft | 39(84%) | 7 (15.2%) | |||
Table 2: Shows the association of wound healing and gingival biotype; suture technique; primary stability and the bone graft used.
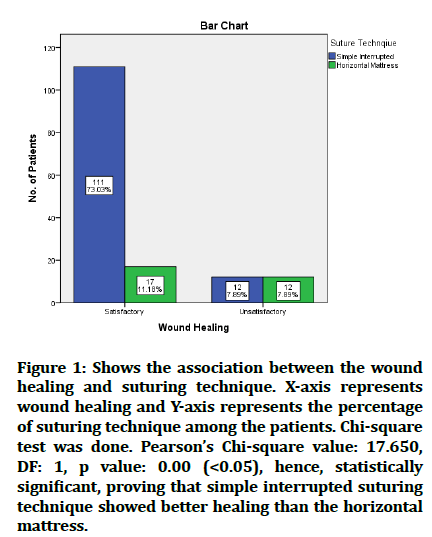
Figure 1: Shows the association between the wound healing and suturing technique. X-axis represents wound healing and Y-axis represents the percentage of suturing technique among the patients. Chi-square test was done. Pearson’s Chi-square value: 17.650, DF: 1, p value: 0.00 (<0.05), hence, statistically significant, proving that simple interrupted suturing technique showed better healing than the horizontal mattress.
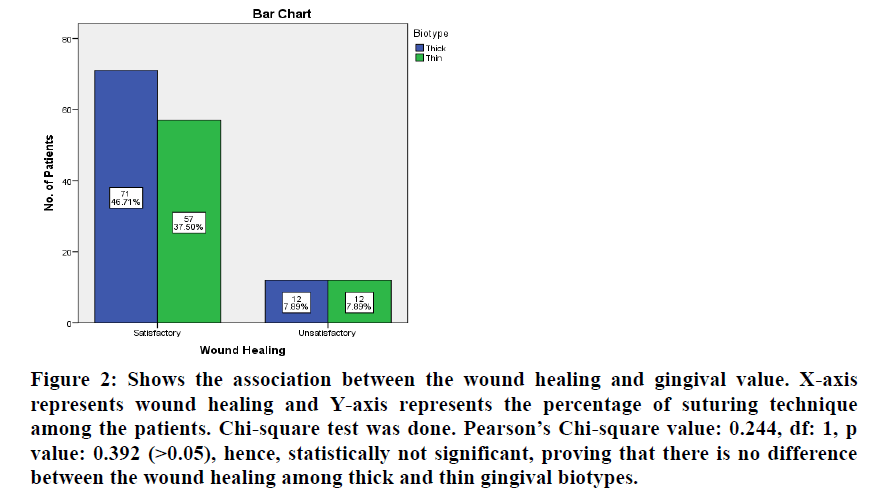
Figure 2: Shows the association between the wound healing and gingival value. X-axis represents wound healing and Y-axis represents the percentage of suturing technique among the patients. Chi-square test was done. Pearson’s Chi-square value: 0.244, df: 1, p value: 0.392 (>0.05), hence, statistically not significant, proving that there is no difference between the wound healing among thick and thin gingival biotypes.
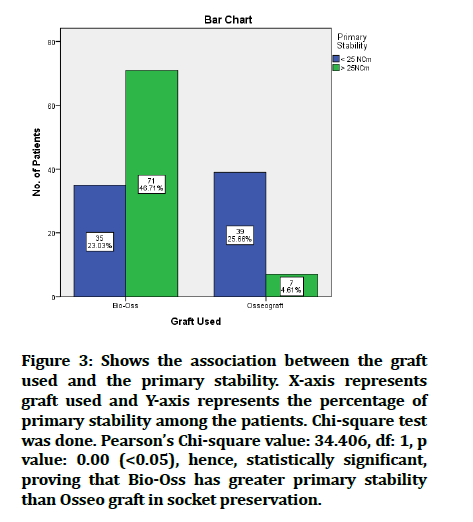
Figure 3:Shows the association between the graft used and the primary stability. X-axis represents graft used and Y-axis represents the percentage of primary stability among the patients. Chi-square test was done. Pearson’s Chi-square value: 34.406, df: 1, p value: 0.00 (<0.05), hence, statistically significant, proving that Bio-Oss has greater primary stability than Osseo graft in socket preservation.
Discussion
Socket preservation procedures aim to minimize ridge resorption and maximize bone regeneration within the alveolus and thus facilitate implant placement in a prosthetically driven position or maintain an acceptable ridge contour in areas of aesthetic concern [7].
The purpose of this study was to evaluate if there is any association seen between the level of implant placement and crestal bone loss associated with it. Many retrospective studies and animal studies where implants have been placed sub crestally and bone loss have been evaluated. A retrospective study by Gopal et al. [8] was done on 118 patients who underwent placement of end osseous dental implants. The study stated that when comparing males and females and different age groups, there was no significant variation in gingival biotype. There was no statistically significant difference between males and females; however, there was a statistically significant difference across age groups. The gingival biotype and soft tissue healing had a statistically significant relationship (p 0.05). Some studies suggest no significance between gingival biotype and soft tissue alterations and long term aesthetic results [6], whereas some recommend management of the implant site based on gingival biotype as thinner biotypes tend higher ridge resorption [9]. In the present study, the thick gingival biotype did not demonstrate significant outcomes compared to the thin gingival biotype.
Simple interrupted suture showed better healing compared to the matressing suture technique in the current study and is similar to a clinical report that employed simple sutures in socket preservation to assess soft tissue healing [10]. In a study conducted by Acar et al., In terms of postoperative discomfort, trismus, and oedema, there were no statistical differences between the two suturing procedures (P > 0.05). The horizontal mattress suturing group had much less wound dehiscence than the simple interrupted suturing group (P: 0017). According to the findings, the horizontal mattress suturing approach is more effective than the standard interrupted suturing technique in wound healing after impacted mandibular third molar surgery, but it does not reduce discomfort, trismus, or swelling study [11].
The limitation of our study is that it is done in an institutional setting; hence there are limited samples. As an institutional study, there can be operator bias and protocol bias seen, affecting bone loss. The present study results have demonstrated that the use of bio-oss resulted in significantly better clinical and radiographic outcomes compared with those obtained using the only Osseo graft. A similar study by Hu et al. Except for one, all of the grafted sockets healed usually. The average period of follow-up was 27.9 months (24 to 31 months). The sockets in the control group healed usually, but complex and soft tissue collapsed three months following extraction. There was no significant difference in the width of the alveolar ridge and associated gingiva in the bone graft group before and after extraction (P > 0.05). The breadth of the alveolar ridge before extraction (7.69 + or 0.48) mm and after extraction (7.68 + or 0.48) mm, as well as the width of associated gingiva before extraction (4.36 + or 1.02) mm and after extraction (4.36 + or 1.02) mm [12] results, were seen in a study where it was shown that the use of a bone xenograft alone or the use of L-PRF combined with a bone xenograft for performing alveolar ridge preservation procedures significantly limited bone resorption [13].
Conclusion
Within the limitations of our study, we conclude that the wound healing is satisfied in patients having thick gingival biotype when a simple interrupted suturing technique was done. The primary stability was better when the socket preservation was done using Bio-oss and achieved to be greater than 25 Ncm. Therefore, the choice of graft and the suturing technique must be considered for socket preservation cases.
Author Contribution
First author (Akhil Ashref) performed the analysis and interpretation and wrote the manuscript. Second author (Subhashree R) contributed to conception, data design, analysis, interpretation and critically revised the manuscript. Third, (Thiyaneswaran N) critically reviewed the manuscript. All the authors have discussed results and revised the manuscript.
Conflict of Interest
The authors declare no conflict of interest, financial or otherwise.
References
- https://www.jaypeedigital.com/book/9789351526391/chapter/ch5
- Venkatesh E, Elluru SV. Cone beam computed tomography: Basics and applications in dentistry. Istanbul Univ Dishekim Fak Derg 2017; 51:S102–21.
- Thakkar DJ, Deshpande NC, Dave DH, et al. A comparative evaluation of extraction socket preservation with demineralized freeze-dried bone allograft alone and along with platelet-rich fibrin: A clinical and radiographic study. Contemp Clin Dent. 2016; 7:371–6.
- Heggeler JMAGT, Ten Heggeler JMAG, Slot DE, et al. Effect of socket preservation therapies following tooth extraction in non-molar regions in humans: A systematic review. Clin Oral Implants Res 2011; 22:779–88.
- Fee L. Socket preservation. Br Dent J 2017; 222:579–82.
- Cabello G, Rioboo M, Fábrega JG. Immediate placement and restoration of implants in the aesthetic zone with a trimodal approach: Soft tissue alterations and its relation to gingival biotype. Clin Oral Implants Res 2013; 24:1094–100.
- Kresnoadi U, Ariani M, Djulaeha E, et al. The potential of mangosteen (Garcinia mangostana) peel extract, combined with demineralized freeze-dried bovine bone xenograft, to reduce ridge resorption and alveolar bone regeneration in preserving the tooth extraction socket. J Indian Prosthod Society 2017; 17:282.
- Gopal TM, Rohinikumar S, Nesappan T. Association of gingival biotype and soft tissue healing one week after implant placement. J Long-Term Effects Med Implant 2020; 30:213–8.
- Nagaraj KR, Savadi RC, Savadi AR, et al. Gingival biotype: Prosthodontic perspective. J Indian Prosthodont Soc 2010; 10:27–30.
- Landsberg CJ. Implementing socket seal surgery as a socket preservation technique for pontic site development: Surgical steps revisited--a report of two cases. J Periodontol 2008; 79:945–54.
- Acar AH, Kazancioğlu HO, Erdem NF, et al. Is horizontal mattress suturing more effective than simple interrupted suturing on postoperative complications and primary wound healing after impacted mandibular third molar surgery? J Craniofac Surg 2017; 28:e657–61.
- Hu XL, Lin Y, Wang J, et al. Clinical study of tissue preservation of extraction socket with Bio-Oss collagen and acellular dermal matrix. Zhonghua Kou Qiang Yi Xue Za Zhi 2009; 44:513–6.
- De Angelis P, De Angelis S, Passarelli PC, et al. Hard and soft tissue evaluation of different socket preservation procedures using leukocyte and platelet-rich fibrin: A retrospective clinical and volumetric analysis. J Oral Maxillofac Surg 2019; 77:1807–15.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Akhil Ashref1, Subhasree R2*, Thiyaneswaran N3, Dimple Rani1, Rajendra Prabhu Abhinav1 and Priyalochana G1
1Deaprtment of Implantology, , Saveetha dental College and Hospital, Saveetha Institute of Medical and Technical Science, Saveetha University, Chennai, India2Deaprtment of Prosthodontics, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical science, Saveetha University, Chennai, India
3Deaprtment of Prosthodontics and Implantology, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical science, Saveetha University, Chennai, India
Citation: Akhil Ashref, Subhasree R, Thiyaneswaran N, Dimple Rani, Rajendra Prabhu Abhinav, Priyalochana G, A Complete Check on the Soft Tissue and Hard Tissue of Patients Undergoing Socket Preservation-A Retrospective Hospital Based Analysis, J Res Med Dent Sci, 2022, 10(1):15-19
Received: 27-Dec-2021, Manuscript No. JRMDS-21-43335; , Pre QC No. JRMDS-21-43335 (PQ); Editor assigned: 29-Dec-2021, Pre QC No. JRMDS-21-43335 (PQ); Reviewed: 12-Jan-2022, QC No. JRMDS-21-43335; Revised: 17-Jan-2022, Manuscript No. JRMDS-21-43335 (R); Published: 24-Jan-2022
