Research - (2020) Volume 8, Issue 6
A Deceiver Feature of SCC: A Rare Case of Oral Lichen Planus Malignant Transformation
Maryam Moshaverinia1, Afshin Bagheri2, Razieh Zare3 and Hajar Shakibasefat4*
*Correspondence: Hajar Shakibasefat, Department of Oral and Maxillofacial Medicine, Faculty of Dentistry, Arak University of Medical Sciences, Iran, Email:
Abstract
Oral Lichen Planus (OLP) is a chronic inflammatory disease of the oral mucosa. Patients with OLP have an increased risk of developing Oral Squamous Cell Carcinomas (OSCCS), with a reported malignant transformation rate between 0% and 5.3%. Current case report is a patient with a primary feature of erythematouse lichen planus but the last feature of OSCC. The nature of OLP favors an active-quiescent-active course. The active course may happen after direct irritation, pchycological stress, medication use, and systemic disease. In our case, presumably, emotional stress was a trigger for exacerbating the disease. Worsening ulceration and induration are clues of malignant transformation and carefull follow up sessions are mandatory for these patients.
Keywords
OLP, OSCC, Malignant transformation
Introduction
Oral lichen planus (OLP) is a chronic disorder that autoreactive T cell lymphocytes have an important role in its pathogenesis. The prevalence rate is between 0.5% to 2.2% [1]. The incidence is more in woman [1-3] and the mean age of onset is in 4th and 5th decade [3]. Various clinical types are: Reticular, Papular, Plaque –like, Bullous, Erythematous, and Ulcerative Lichen Planus. OLP as a premalignant lesion has an increased risk for neoplastic changes in oral cavity. Oral Squamous Cell Carcinoma (OSCC) will occure in OLP patients with malignant transformation rate between 0% and 5.3% [4]. In this study, we present a 41-year-old woman with a primary feature of erythematous oral lichen planus but the last feature of OSCC. The patient was treated with a composite resection and reconstructed with a deep circumflex iliac artery (DCIA) flap.
Case History and Detail
The patient was a 41-year-old woman with chief complaint of erythematouse and erosive lesions of gingiva, who was referred to Oral and Maxillofacial Department of Shiraz Dental School in July 2011 for the first time. Due to clinical impression of oral lichen planus, a biopsy was taken. the histopathological report showed nonspecific inflammation probably due to insufficient sampling. She had megaloblastic anemia and received iron and calcium supplement. Medical history, careful clinical and histopathological examination, and laboratory investigations ruled out the possibility of drugor restoration-related lichenoid reactions, and/ or oral lichenoid manifestation of systemic disease.
Treatment began according to clinical diagnosis of LP included topical steroid (Volon ointment) and combination of Diphenhydramine syrup and Aluminium-Mg suspension and dexamethasone as a palliative mouthwash. Because of the temporary subsidence of the disease she disconnected the therapy and did not attend the follow up sessions.
In the latest follow up session (in March 2018), After a sudden psychological stress the lesions of gingiva and sever gingival recession of posterior right side of mandible occurred, seven years after her first oral visit in Shiraz Dental School. In clinical examination there was no plaque and calculus associated with severe gingival lesions (Figure 1).
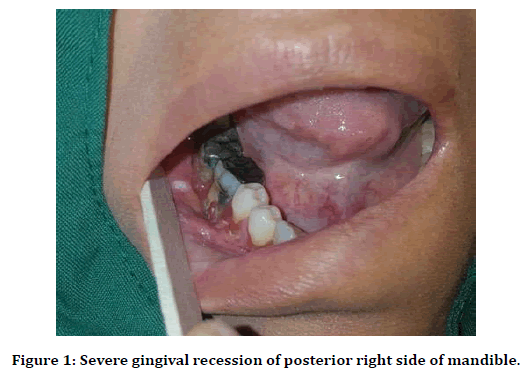
Figure 1. Severe gingival recession of posterior right side of mandible.
Periapical radiography showed severe bone loss with ill-defined border in first molar area of right mandibular side. Two specimens were taken from the most indurated part of facial gingiva of second premolar and a popular white lesion in right buccal mucosa. The histopathological report showed moderate dysplasia of the papule on buccal mucosa and Squamous Cell Carcinoma with moderate differentiation of facial gingival tissue (Figure 2). The patient was referred to an oral and maxillofacial surgeon and oncologist. Multidetector 3D CT scan of the mandibe showed a 35×13×15 mm osteolytic lesion in the right side of the body of the mandible involving the root of the molar teeth with destruction of the cortex in the medial and lateral aspect. In Figure 3 computed tomography shows right mandibular bony destruction.
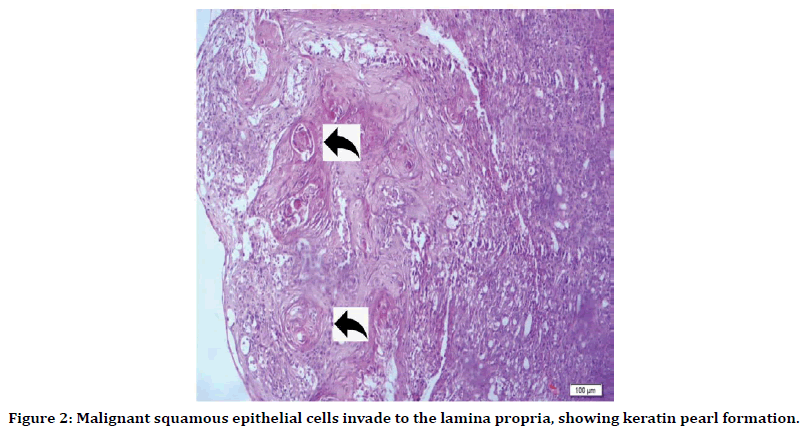
Figure 2. Malignant squamous epithelial cells invade to the lamina propria, showing keratin pearl formation.
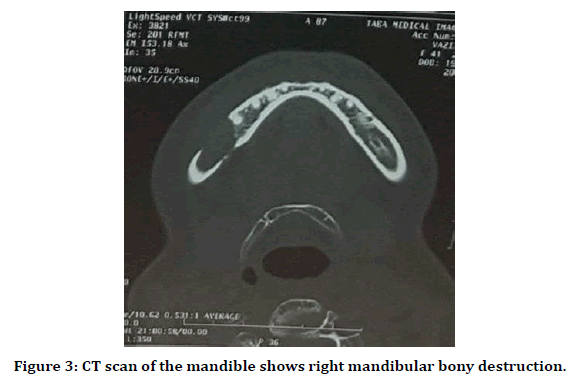
Figure 3. CT scan of the mandible shows right mandibular bony destruction.
Due to stage IV OSCC (T4aN1M0) the patient underwent composite resection with right extensive segmental mandibulectomy, resection of buccal mucosa and right supraomohyoid neck dissection. A right-side deep circomflex iliac artery and vein (DCIA) graft was used for reconstruction with anastomosis to facial artery and external jugular vein. The graft was secured in position with plates and screws.
The hole in pelvic bone was left to heal on its own and after one week the patient was able to walk without help. During the first week after the operation she was fed through a gastrostomy tube.
Discussion
The patients with OLP have an increased risk for malignant transformation with the incidence rate of 0.2% per year. The increased risk is obscure to be related to a specific type of OLP, but plaque type and ulcerative lesions are overrepresented [1]. One other research showed that, malignancy occures more in erosive and erythematous types [5]. OLP has an active-quiescent-active mode, and active phase may occure after some conditions, such as stressful psychological states, systemic disease and use of some special drugs [6]. Buccal mucosa is the most affected site of oral lichen planus followed by tongue and gingiva [7]. Histopathological findings especially dysplasia in OLP patients can affect on pathogenesis and progression of the disease to malignancy. Dysplasia in older patients with lichen planus is significantly higher than younger patients [8].
Indurated ulceration is a sign of malignancy in OLP. Malignant transformation is related to various factors, like genetic, alcohol abuse, smoking, candidiasis, HPV infection, immunosuppressed conditions, and nutritional states [9-11]. Also, some changes in gene expression of p53, COX-2, Smad3, Bmil, CD133, and Myc-1 are predictors of malignancy [12]. Cancerogenesis is highly suspected to be a result of constant stimulation by inflammatory T cell mediators and oxidative changes [13]. Regarding patient gender and age, the risk is greater in women, and between the sixth and seventh decades of life [9,14]. Neoplastic changes need at least 6 months duration to occure after the first manifestation of OLP [9].
In a case report of a 62-year-old woman with sever cutaneous and erosive oral lichen planus, malignant transformation to invasive Squamous Cell Carcinoma occurred in right maxillary area. The patient also had neuralgia along maxillary nerve, due to perineural involvement of SCC [15].
In another case study of a 37-year-old woman with no history of alcohol and tobacco use, malignant transformation of erosive OLP in buccal mucosa occurred with involvement of her gingiva and tongue, this patient underwent chemoradiation therapy and surgery [16].
Also, Carcinoma in situ arising in the oral druginduced lichenoid lesion of buccal mucosa was reported in a 66-year-old female using Simvastatin after 7-year follow-up [17].
In our study a 41-year-old woman with no history of alcohol and tobacco use and no medication that induced oral lesion, experienced oral SCC in the base of chronic inflammation of mandibular gingiva after seven years. She underwent extensive segmental mandibulectomy, resection of buccal mucosa and right supraomohyoid neck dissection.
In all these cases chronic inflammation was existed and the association between chronic inflammation and malignant transformation has been proven [4].
The management of OLP with malignant transformation and invasive OSCC depends on patient's condition and stage of tumor. Because of high rate of nodal involvement and metastase, awfully close follow up sessions every 2 months for the first 6-9 month after diagnosis is necessary [18]. Thereafter, an examination every 4 months is suggested as sufficient for detecting future complications [15]. A new research showed NBI (Narrow-Band Imaging as a good method for determination of OLP malignant transformation. It may be helpful for early detection of OLP neoplastic changes in follow up sessions [19].
Acknowledgments
The authors would like to thank Dr. Daneshbod Pathobiology Laboratory, TABA and Faraparto Medical Imaging and Interventional Radiology Centers and Shahriar Hospital (Shiraz, Fars, Iran) for their excellent cooperation.
References
- Glick M. Burket's oral medicine: PMPH USA; 2015.
- Mozaffari HR, Sharifi R, Sadeghi M. Prevalence of oral lichen planus in diabetes mellitus: A meta-analysis study. Acta Inform Med 2016; 24:390.
- Mozaffari H, Ziaei N, Nazari H, et al. Oral lichen planus treatment by CO2 laser: A systematic review. Asian J Sci Res 2017; 10:1-9.
- Bombeccari GP, Guzzi G, Tettamanti M, et al. Oral lichen planus and malignant transformation: A longitudinal cohort study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011; 112:328-334.
- Bermejo-Fenoll A, Sanchez-Siles M, López-Jornet P, et al. Premalignant nature of oral lichen planus. A retrospective study of 550 oral lichen planus patients from south-eastern Spain. Oral Oncol. 2009; 45:e54-e56.
- Eisen D. The clinical features, malignant potential, and systemic associations of oral lichen planus: a study of 723 patients. J Am Acad Dermatol 2002; 46:207-214.
- Mozaffari HR, Rahmani M, Rezaei F, et al. Evaluation of oral lichen planus frequency in patients referred to pathology centers of Kermanshah city, during 2008 to 2011. Sch J App Med Sci. 2016; 4:2200-2222.
- Mozaffari HR, Mirbahari S, Sadeghi M. Histopathological findings in oral lichen planus: A three-year report from western Iran. J Res Med Dent Sci 2018; 6:274-278.
- Gandolfo S, Richiardi L, Carrozzo M, et al. Risk of oral squamous cell carcinoma in 402 patients with oral lichen planus: A follow-up study in an Italian population. Oral Oncol 2004; 40:77-83.
- Lodi G, Scully C, Carrozzo M, et al. Current controversies in oral lichen planus: report of an international consensus meeting. Part 1. Viral infections and etiopathogenesis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005; 100:40-51.
- Lozada-Nur F. Oral lichen planus and oral cancer: Is there enough epidemiologic evidence? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 89:265.
- Olson MA, Rogers RS, Bruce AJ. Oral lichen planus. Clin Dermatol 2016; 34:495-504.
- Georgakopoulou EA, Achtari MD, Achtaris M, et al. Oral lichen planus as a preneoplastic inflammatory model. J Biomed Biotechnol 2012; 2012.
- Lanfranchi-Tizeira HE, Aguas SC, Sano SM. Malignant transformation of atypical oral lichen planus: A review of 32 cases. Med Oral 2003; 8:2-9.
- Braun KA, Massa L. Oral lichen planus with malignant transformation to invasive squamous cell carcinoma. Cutis. 2015; 96:e12.
- Soo J, Kokosis G, Ogilvie M. A rare case of malignant transformation of oral lichen planus of the mandible. Plast Reconstr Surg 2016; 4.
- Phattarataratip E, Dhanuthai K, Thongprasom K. Carcinoma in situ arising in the oral lichenoid lesion-An unusual case report. J Med Surg Pathol 2016; 1:2.
- Mignogna M, Russo LL, Fedele S, et al. Clinical behavior of malignant transforming oral lichen planus. Eur J Surg Oncol. 2002; 28:838-843.
- Cozzani E, Russo R, Mazzola F, et al. Narrow-band imaging: A useful tool for early recognition of oral lichen planus malignant transformation? Eur J Dermatol 2019; 29:500-506.
Author Info
Maryam Moshaverinia1, Afshin Bagheri2, Razieh Zare3 and Hajar Shakibasefat4*
1Department of Oral and Maxillofacial Medicine, Shiraz University of Medical Sciences, Shiraz, Iran2Department of Maxillofacial Oncology, Shiraz University, Iran
3Department of Oral and Maxillofacial Pathology, Shiraz University of Medical Sciences, Shiraz, Iran
4Department of Oral and Maxillofacial Medicine, Faculty of Dentistry, Arak University of Medical Sciences, Arak, Iran
Citation: Maryam Moshaverinia, Afshin Bagheri, Razieh Zare, Hajar Shakibasefat, A Deceiver Feature of SCC: A Rare Case of Oral Lichen Planus Malignant Transformation, J Res Med Dent Sci, 2020, 8 (6): 142-145.
Received: 15-Aug-2020 Accepted: 21-Sep-2020
