Research Article - (2023) Volume 11, Issue 9
A Demographic Profile of Patients Presenting with Post COVID Mucormycosis: Risk Factors and their Ophthalmic Involvement in a Major Tertiary Care Center in Central India
Richa Tripathi*, Bahubali Jain and Ritika Tripathi
*Correspondence: Dr. Richa Tripathi, Department of Ophthalmology, Netaji Subhash Chandra Bose Medical College, Madhya Pradesh, India, Email:
Abstract
Objectives: The study is performed to search for the probable cause of sudden rise in incidence of post COVID mucormycosis and demographic profile of such patients.
Materials and methods: This is a retrospective study conducted on 100 post COVID patients admitted in mucormycosis ward in NSCB medical college during month of May 2021. Risk factors, demographic profile and clinical presentation of the patients were reviewed with special reference to ophthalmic involvement.
Results: Upon analysis it was found that maximum 69% patients were of age group 41 yrs-60 yrs and 56% presented in 1-3 weeks, 66% patients had history of hospital admission and 34% were home isolated, 62% had history of oxygen requirement, 41% of which required it for 5-10 days, 88% had history of steroid and also 88% were found to be diabetic. 60% of the patients had ophthalmic symptoms out of which 38% were unilateral blind and 5% were bilateral blind.
Conclusion: Spores of mucormycosis have been ubiquitous in nature but there has to cause search of these docile spores overpowering human immunity and causing fatality. Given due to high mortality and rapid progression of mucormycosis it is of utmost importance to upraise awareness, identify the high risk groups, recognize the disease in earlier stages and treat aggressively with multidisplinary approach involving both surgery and specific medication.
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Keywords
Post COVID, Rhino orbito cerebral mucormycosis, Demographic profile, Patient presentation, Staging, Ophthalmic involvement
Introduction
Mucormycosis is an aggressive opportunistic fungal infection, also known as phycomycosis and zygomycosis. Mucormycosis infection of the sinuses is a form of lifethreatening invasive fungal sinusitis that typically affects immune compromised individuals with an impaired neutrophil response. It is an angioinvasive disease that is characterized by tissue infarction and necrosis [1].
The clinical presentations of mucormycosis are classified on the basis of anatomic localization, such as Rhino Orbital Cerebral Mucormycosis (ROCM), pulmonary, gastrointestinal, cutaneous, renal and disseminated mucormycosis. Clinically, ROCM can present with atypical signs and symptoms similar to complicated sinusitis, such as nasal blockade, crusting, facial pain and oedema, proptosis, ptosis, chemosis, ophthalmoplegia, loss of vision with headache and fever and various neurological signs and symptoms if intracranial extension is present. A black eschar is often seen in the nasal cavity or over the hard palate region, but is not characteristic.
Histological features include mycotic infiltration of blood vessels, vasculitis with thrombosis, tissue infarction, hemorrhage and acute neutrophilic infiltrate. Even with prompt diagnosis, treatment of underlying diseases and aggressive medical and surgical intervention, the management is often not effective, leading to an extension of the infection and ultimately death [2].
COVID-19 caused by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) has been associated with a wide range of opportunistic bacterial and fungal infections. Recently, a change in the incidence of mucormycosis infection of the sinuses has been observed, with more cases being diagnosed much more frequently. A firm association between COVID-19 and increased fungal infections can now be clearly seen. Mehta and Pandey reported a single case of a 60-year-old male with ROCM associated with COVID-19 in September 2020. Another such case report was published by Werthman-Ehrenreich in the same month. White et al. studied 135 adults with COVID-19 infection and reported an incidence of 26.7 percent for invasive fungal infections [3].
The primary reason facilitating mucorales spores to germinate in people with COVID-19 is an ideal environment of low oxygen, high glucose (diabetes, newonset hyperglycemia, steroid-induced hyperglycemia), acidic medium (metabolic acidosis, DKA) and decreased phagocytic activity of white blood cells due to immunosuppression coupled with several other shared risk factors including prolonged hospitalization with or without mechanical ventilators.
The overall numbers increase from 25 cases per year (1990 to 2007) to 89 cases per year (2013-2015). Contrary to the last wave, during the second wave of COVID 19 there has been a sudden spurt in cases of mucormycosis with around 10000 mucormycosis suspects being identified all over India. Over the past month in NSCB medical college Jabalpur, a tertiary care hospital, there has been a sudden rise in cases of invasive fungal sinusitis, specifically mucormycosis which is a medical emergency [4].
Materials and Methods
This is a retrospective study of post covid patients admitted in mucormycosis ward in Netaji Subhash Chandra Bose medical college during month of May 2021. 100 post COVID patients diagnosed with ROCM on the basis of clinical manifestation, radiological investigation and endoscopic biopsy of sinus are included in study.
A retrospective study was performed to identify the risk factors for development of post COVID mucormycosis and the demographic profile of patients. Informed consent was taken to patients in study [5].
Results
Out of 100 patients in study 79 were male and 21 females. 15 patients were below age of 40 years, 69 from age group of 41 to 60 years and 16 patients more than 60 yrs (Table 1).
Taking interval between COVID-19 positive diagnosis and development of mucormycosis symptoms patients were divided into 3 groups (Table 2). 21% presented within 1 week of covid. Maximum presented in interval of 1-3 weeks which was 56% and 23% after 3 weeks. History highlighted following results: 66% patients had hospital admission whereas 34% were home isolated (Table 3) [6].
62% patient oxygen requirement during treatment out of which 18% used NRM, 30% Hudson mask and 12% nasal prongs and 2% BIPAP while 38% cases didn’t require oxygen. It was found that out of 62% patient who required oxygen, 32% needed it for less than 5 days, 21% for 5-10 days and 9% for >10 days. Of 62%, 12% were admitted in hospitals with central supply oxygen while others used either oxygen cylinders or industrial oxygen.
During the treatment 53% patients took steroids by i/v route, while 28% had oral intake and 7% had no history while 12% did not know about it. During treatment 68% took zinc during treatment. 89% patients were on antibiotic coverage.
The most significant and common factor in history was found to be diabetes which was found in 88% of the patient among which 24% were newly diagnosed (Table 4). In our study 1 patient had history of HIV. 3 patients had malignancy and 18 patients were undergoing treatment of previous respiratory illness 12 patients had chronic kidney disease.
Out of 100 patients 2 patients presented in stage 1 with complains of nasal stuffiness and epistaxis. 32 patients presented in stage 2 with U/L or B/L sinus involvement (Table 5). 60 patients presented with ophthalmological signs and symptoms in stage 3. Out of these 6% patients presented in stage 3 which involved only congestion chemosis and periorbital pain (Table 5) [7].
15% patients presented in stage 3 which involved restricted eye movements with or without ptosis. 37% patients presented in stage 3 all of which were U/L blind and presented mostly with total ophthalmoplegia. 2 patients were in stage 3d with B/L vision loss but no intracranial extension. 6 patients presented in stage 4 with intra cranial extension out of which 1 was U/L blind 3 were B/L blind and 2 had intact vision (Table 6).
| Age at prsentation | <40 yrs | 41-60 yrs | >60 yrs |
|---|---|---|---|
| Total patients 100 | 15 | 69 | 16 |
Table 1: Age presentation.
| Presentation of symptoms after COVID positive result | <1 week | 1-3 week | >3 week |
|---|---|---|---|
| Total PT 100 | 21 | 56 | 23 |
Table 2: Symptoms of mucormycosis patients.
| Post COVID patients with mucormycosis | Total patients | 100 | ||
|---|---|---|---|---|
| History of hospital admission | Hospital admission | 66 | ||
| Home isolation | 34 | |||
| Duration of oxygen exposure | <5 days | 11 | ||
| 5-10 days | 41 | |||
| >10 days | 10 | |||
| History of oxygen exposure | Absent | 38 | ||
| Present | 62 | BiP | 2 | |
| NP | 12 | |||
| HM | 31 | |||
| NRM | 17 | |||
| History of steroid | IV | 53 | ||
| No | 7 | |||
| Oral | 28 | |||
| Not known | 12 | |||
| History of zinc intake | No zinc | 37 | ||
| Zinc | 63 | |||
| History of antibiotic intake | Yes | 89 | ||
| No | 5 | |||
| Not known | 6 | |||
Table 3: History of mucormycosi ptients.
| Total patients | DM | Newly diagnosed dm | No history of dm | |
|---|---|---|---|---|
| 100 | 64 |
24 | 12 | |
| Uncontrolled | Controlled | |||
| 46 | 18 | |||
Table 4: Newly diagnosed patients.
| Stage at presentation | Stage 1 | Stage 2 | Stage 3 | Stage 4 | |||
|---|---|---|---|---|---|---|---|
| 100 | 2 |
32 |
60 |
6 | |||
| Stage 3a | Stage 3b | Stage 3c | Stage 3d | ||||
| 6 | 15 | 37 | 2 | ||||
Table 5: Stage presentation.
| Patients with ophthalmic involvement | 60 | ||
|---|---|---|---|
| Congestion | 17 | ||
| Chemosis | 28 | ||
| Proptosis | 10 | ||
| Ptosis | 55 | Mild | 9 |
| Mod | 3 | ||
| Severe | 43 | ||
| Ophthalmoplegia | Restricted | 8 | |
| Total | 41 | ||
| Pupil reaction |
Mid dil not reacting | 39 | |
| RAPD | 4 | ||
| NSRL | 16 | ||
| Vision loss | UL | 38 | |
| BL | 5 | ||
| Peri orbital crusting | 2 | ||
Table 6: Patients with ophthalmic involvement.
Discussion
A myriad of manifestations and complications have been documented with COVID 19 infection, new ones are emerging and being reported, newest being, mucormycosis, not a new disease just previously a rare disease found in immunocompromised individuals, but in present scenario with COVID pandemic sudden exponential increase in cases is creating havoc in world and especially India where there are thousands of cases with increasing mortality and situation getting out of hand. Mucormycosis in last wave of COVID had few cases, but for this wave, there is no clear data to find the causes responsible for such mammoth spread [8,9].
Mucor is a saprophytic fungus; its spores spread in soil, air, food and decaying organic material. ROCM refers to the entire spectrum ranging from limited sino-nasal disease, limited rhino orbital disease (progression to orbits) to rhino-orbital-cerebral disease (CNS involvement). The area of involvement may differ due to underlying condition. The signs, symptoms and radiographic findings of mucormycosis are nonspecific; direct histologic examination of scrapings or biopsies of involved tissue or paranasal sinus secretions are diagnostic. The fungal invasion may be patchy, so multiple biopsies may be required for definitive diagnosis [10].
It may be present in the nasal mucosa of healthy people as a commensal but when patient becomes immunosuppressed, this fungus may germinate within the paranasal sinuses and it may spread directly to the orbital apex and gain intracerebral access. The optic nerve may be affected resulting in vision loss. Involvement of the superior orbital fissure and its contents, such as cranial nerves III, IV and VI and branches of V1 and V2, may cause diplopia, ophthalmoplegia and sensory loss to areas of the cornea and face [11].
Mucormycosis is difficult to diagnose early, as patients often present with non-specific symptoms. When orbital apex involvement develops, it is often too late to save the patient’s vision, eye or life.
The proposed staging system follows the general progression and severity.
Stage 1: Involvement of the nasal mucosa
• Limited to the middle turbinate (Figure 1).
• Involvement of the inferior turbinate or ostium of the
nasolacrimal duct.
• Involvement of the nasal septum.
• Bilateral nasal mucosal involvement.
• Symptoms of stage 1-nasal stuffiness, nasal discharge,
foul smell, epistaxis.
Stage 2: Involvement of paranasal sinuses
• One sinus.
• Two ipsilateral sinuses.
• >Two ipsilateral sinuses and/or palate/oral cavity
(Figure 2).
• Bilateral paranasal sinus involvement or involvement
of the zygoma or mandible.
Stage 3: Involvement of the orbit
• Nasolacrimal duct, medial orbit, vision unaffected.
• Diffuse orbital involvement (>1 quadrant or >2
structures), vision unaffected.
• Central retinal artery or ophthalmic artery occlusion
or superior ophthalmic vein thrombosis; involvement
of the superior orbital fissure, inferior orbital fissure,
orbital apex, loss of vision (Figure 3).
• Bilateral orbital involvement.
Stage 4: Involvement of the CNS
• Focal or partial cavernous sinus involvement and/or
involvement of the cribriform plate.
• Diffuse cavernous sinus involvement and/or
cavernous sinus thrombosis.
• Involvement beyond the cavernous sinus, i.e., skull
base, internal carotid artery occlusion, brain
infarction.
• Multifocal or diffuse CNS disease (Figure 4).
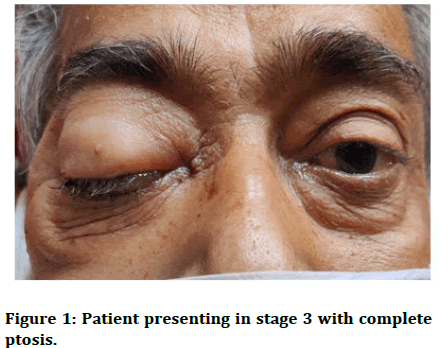
Figure 1: Patient presenting in stage 3 with complete ptosis.
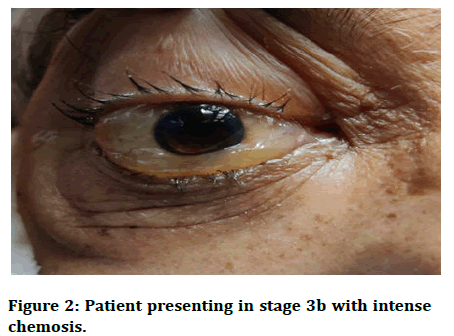
Figure 2: Patient presenting in stage 3b with intense chemosis.
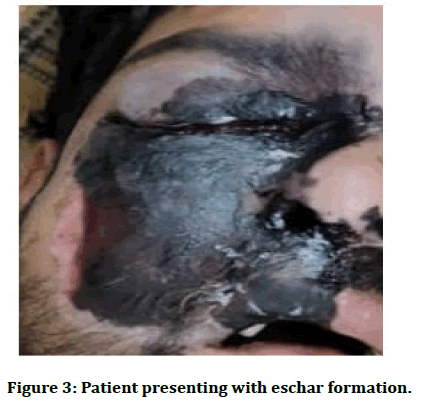
Figure 3: Patient presenting with eschar formation.
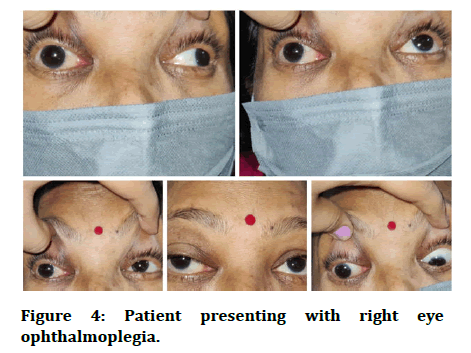
Figure 4: Patient presenting with right eye ophthalmoplegia.
In our study there was male preponderance, the reason might be because of male more mobile in the environment where spores are found. The most probable age group is late middle age group from 40-60 bearing the maximum caseload while the extreme age groups are less prevalent [12].
The patients included in the study are post COVID mucormycosis cases who had RT-PCR/RAT Positive and or took treatment based on HRCT CTSS score. Majority of the patient complained of the initial symptom within 1-3 weeks after diagnosed positive mostly after getting discharged from hospital, while very few got it while admission or after being discharged >3 weeks. Though maximum patients had history of admission many were home isolated which proves that only hospital environment isn’t a major factor. Though there was an increased oxygen exposure in cases but also a significant numbers state no oxygen use forcing us to look for other factors. The duration of oxygen was found to be maximum 10 days or less in patients very few requiring above it [13,14]. An important factor to be taken into consideration here is that among those 62%, 12% were admitted in hospitals with central supply oxygen while others used either oxygen cylinders or industrial oxygen which should be studied more keenly to find out any association between the same.
Coming to the biggest and common factor causing immunodeficiency in patients of mucor is Diabetes Mellitus (DM) in any form. Around 80% patients having the disease or uncontrolled steroid induced hyperglycemia during covid accounting for newly diagnosed DM during or after covid and its inefficient control with concurrent steroid use. Moreover, steroid use reduces the phagocytic activity of WBC, causes impairment of bronchoalveolar macrophages migration, ingestion and phagolysosome fusion, making a diabetic exceptionally vulnerable to mucormycosis as stated in various articles. As found in the study maximum patient had taken steroids in any form mainly iv and oral and equal with slight preponderance to the i/v group, a humongous factor to be considered for this epidemic which immunocompromises the host and its concurrent excessive and at times nonjudicial use of steroids [15].
During the treatment almost all had antibiotics with a very few exceptions. Another factor was zinc intake as proposed by some, zinc provides a suitable environment in body for fungus growth and thus can have its role.
ROCM and eye: the orbital and eye involvement is extensive, with ophthalmic findings in more than half of the patients in ROCM requiring stat and aggressive treatment because prognosis becomes poor if eye is involved causing threat of cerebral involvement, next natural course of disease and thus, fatal.
Conclusion
Many patients had initial ophthalmic complaints (stage 3) as they fail to recognize signs in initial nasal and paranasal stages of disease. Eye symptoms start appearing after involvement of lamina papyracea through ethmoid sinuses or through lacrimal apparatus. The patients present with a wide but repetitive ophthalmic signs and symptoms consisting of headache to permanent blindness -U/L or B/L. The cause of vision loss is either contributed to CRAO (maximally), optic nerve or corneal involvement which is usually irreversible. There is rapid involvement of brain after there are eye signs especially if there is vision loss, thus mandating appropriate management to avoid case fatality.
References
- Scheckenbach K, Cornely O, Hoffmann TK, et al. Emerging therapeutic options in fulminant invasive rhinocerebral mucormycosis. Auris Nasus Larynx 2010; 37:322-328.
[Crossref] [Google scholar] [PubMed]
- Vairaktaris E, Moschos MM, Vassiliou S, et al. Orbital cellulitis, orbital subperiosteal and intraorbital abscess: Report of three cases and review of the literature. J Craniomaxillofac Surg 2009; 37:132-136.
[Crossref] [Google scholar] [PubMed]
- de Shazo RD, Chapin K, Swain RE. Fungal sinusitis. N Engl J Med 1997; 337:254-259.
[Crossref] [Google scholar] [PubMed]
- Musa QH, Mohammed HI, Al-Assadi HZ. Evaluation of prognostic factors in management of associated COVID-19 oro-facial mucormycosis. J Popul Ther Clin Pharmacol 2023; 30.
- Peterson KL, Wang M, Canalis RF, et al. Rhinocerebral mucormycosis: Evolution of the disease and treatment options. Laryngoscope 1997; 10:855-862.
[Crossref] [Google scholar] [PubMed]
- Singh AK, Singh R, Joshi SR, et al. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab Syndr 2021; 15:102146.
[Crossref] [Google scholar] [PubMed]
- Sharma S, Grover M, Bhargava S, et al. Post coronavirus disease mucormycosis: A deadly addition to the pandemic spectrum. J Laryngol Otol 2021; 135:442-427.
[Crossref] [Google scholar] [PubMed]
- Choksi T, Agrawal A, Date P, et al. Cumulative mortality and factors associated with outcomes of mucormycosis after COVID-19 at a multispecialty tertiary care center in India. JAMA Ophthalmol 2022; 140:66-72.
[Crossref] [Google scholar] [PubMed]
- Raj A, Nishant P, Sadhukhan K, et al. A cross-Sectional study to describe the spectrum of ocular manifestations and risk factors of mucormycosis presenting to a tertiary hospital of east India. Indian J Ophthalmol 2023; 71:249-256.
[Crossref] [Google scholar] [PubMed]
- Patel R, Jethva J, Bhagat PR, et al. Rhino-orbital-cerebral mucormycosis: An epidemiological study from a tertiary care referral center in western India. Indian J Ophthalmol. 2022; 70:1371-1375.
[Crossref] [Google scholar] [PubMed]
- Baghel SS, Keshri AK, Mishra P, et al. The spectrum of invasive fungal sinusitis in COVID-19 patients: Experience from a tertiary care referral center in northern India. J Fungi 2022; 8:223.
[Crossref] [Google scholar] [PubMed]
- Jain K, Surana A, Choudhary TS, et al. Clinical and histology features as predictor of severity of mucormycosis in post-COVID-19 patients: An experience from a rural tertiary setting in central India. SAGE Open Med 2022; 10:20503121221074785.
[Crossref] [Google scholar] [PubMed]
- Singh S, Basera P, Anand A, et al. COVID-19-associated mucormycosis in a tertiary care hospital in India: A case series. Cureus 2022; 14:e27906.
[Crossref] [Google scholar] [PubMed]
- Ravani SA, Agrawal GA, Leuva PA, et al. Rise of the phoenix: Mucormycosis in COVID-19 times. Indian J Ophthalmol. 2021; 69:1563-1568.
[Crossref] [Google scholar] [PubMed]
- Singh Y, Ganesh V, Kumar S, et al. Coronavirus disease-associated mucormycosis from a tertiary care hospital in India: A case series. Cureus 2021; 13:e16152.
[Crossref] [Google scholar] [PubMed]
Author Info
Richa Tripathi*, Bahubali Jain and Ritika Tripathi
Department of Ophthalmology, Netaji Subhash Chandra Bose Medical College, Madhya Pradesh, IndiaCitation: Richa Tripathi, Bahubali Jain, Ritika Tripathi, A Demographic Profile of Patients Presenting with Post COVID Mucormycosis: Risk Factors and their Ophthalmic Involvement in a Major Tertiary Care Center in Central India, J Res Med Dent Sci, 2023, 11 (09): 001-006.
Received: 14-Jun-2021, Manuscript No. jrmds-23-33678; , Pre QC No. jrmds-23-33678 (PQ); Editor assigned: 18-Jun-2021, Pre QC No. jrmds-23-33678 (PQ); Reviewed: 02-Jul-2021, QC No. jrmds-23-33678; Revised: 18-Aug-2023, Manuscript No. jrmds-23-33678 (R); Published: 15-Sep-2023
