Case Report - (2022) Volume 10, Issue 9
A Rare case of drug induced usual interstitial pneumonia
Boddepalli Madhuri*, Umashankar, A Sankar, Kanmani and Raviteja Reddy
*Correspondence: Boddepalli Madhuri, Department of General Medicine, Sree Balaji Medical College and Hospital, Chrompet, India, Email:
Abstract
Amiodarone is an anti-arrhythmic drug that is generally used for arrhythmias like supraventricular tachycardia and ventricular tachycardia, atrial fibrillation. It will cause different adverse effects, among them amiodarone induced pulmonary toxicity is most serious complication. This is normally described in patients who are using amiodarone from long time of duration and in high accumulative doses .But here we are reporting amiodarone therapy in short term duration, induced pulmonary toxicity. In this case, 72 yrs. old female who presented with symptoms of interstitial pneumonia, after a few months of therapy with amiodarone for post MI atrial fibrillation. So it is important to be aware of this rare type of early onset pulmonary toxicity in patients with amiodarone therapy.
Keywords
Amiodarone, Interstitial pneumonia, Ground glass opacities, Traction bronchiectasis
Introduction
Amiodarone is a Benzofuran derivative antiarrhythmic drug, that is frequently used in atrial fibrillation, supra ventricular tachycardia and ventricular tachycardia. Pulmonary toxicity due to amiodarone is one of the serious side effects of therapy. Usual interstitial pneumonia (UIP) is a concept that is deeply entrenched in clinical practice and the prognostic significance of UIP is well established, but the field continues to suffer from the lack of a true gold standard for diagnosing fibrotic interstitial lung disease (ILD). The meaning and usage of UIP have shifted over time and this term is prone to misinterpretation and poor diagnostic agreement [1-5].
Case Report
A 72 yrs. old female patient was admitted to the hospital with palpitations, chest discomfort, absent P waves in ECG, normal chest X-ray. Patient was diagnosed as AF. She had medical history of CAD (anteroseptal MI) 2 years back, post per cutaneous coronary stenting, hypertension, type 2 diabetes mellitus on irregular treatment since 6 months. Amiadarone was started at initial loading dose of 150 mg, followed by dose of 360 mg infusion over 6 hrs, 540 mg infusion over next 18 hrs. Later patient was discharged on maintenance dose of 400 mg/day.
After 2 months she came with complaints of dry cough, breathlessness which are sudden in onset progressive in nature since 2 weeks. Saturation on room air was 88%. when compared with initial chest X-ray findings; follow up X-ray, demonstrated reticular opacities.
Total count showed 11800/mm3.sputum culture and blood culture reports are negative. Gram stain, smear for TB organisms, ANA, RF-factor are also negative, meanwhile antibiotics also started but no change was noted in chest X-ray. HRCT chest showed extensive areas of interstitial reticular opacities, honey combing, ground glass opacities, patchy areas of collapse consolidations, sub pleural fibrosis and minimal traction bronchiectasis in bilateral lung fields, owing to suspicion of amiodarone induced usual interstitial pneumonia (Figures 1 and 2).
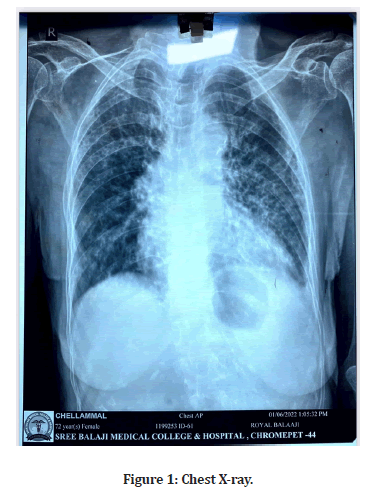
Figure 1: Chest X-ray.
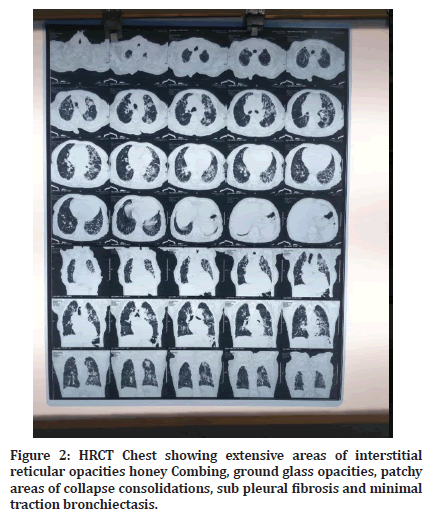
Figure 2:HRCT Chest showing extensive areas of interstitial reticular opacities honey Combing, ground glass opacities, patchy areas of collapse consolidations, sub pleural fibrosis and minimal traction bronchiectasis.
Discussion
Amiodarone is a highly effective anti-arrhythmic drug that is frequently used in atrial fibrillation because of its rapid onset of action, high conversion rate, and minimal cardiac depression. But treatment with amiodarone has been associated with various types of side effects, including pulmonary toxicity. This pulmonary toxicity can present as different types in different patients such as chronic interstitial pneumonitis, RDS, organizing pneumonia and solitary pulmonary mass. The mechanisms involved in causing this are incompletely understood, but two hypotheses include direct cytotoxicity and a hypersensitivity reaction. The risk factors to cause this pulmonary toxicity in general include high doses daily (more than 400 mg/day) or longer duration of use, Preexisting lung disorders and old age.
Amiodarone induced pulmonary toxicity is diagnosis of exclusion. Because it’s nonspecific nature of disease progression, and its ability to mimic other disease processes. So the diagnosis of this pulmonary toxicity may be missed or delayed. A reduction in DLCO of 15% is a strong indicator for the diagnosis of pulmonary toxicity due to amiodarone, having sensitivity of 68-97%. lung biopsy may help in pathological type of toxicity (Eg. chronic interstitial pneumonia), but nonspecific for amiodarone induced disease. In this patient initially treated with antibiotics and diuretics as we suspected pneumonia and pulmonary edema due heart failure, but no improvement was found, after HRCT we discontinued amiodarone as this is the primary treatment for amiodarone toxicity [1-5].
Conclusion
Early onset of pulmonary toxicity with the amiodarone therapy can occur anytime during therapy may be due to presence of other risk factors.so it can occur even if it is not higher dose and long duration of use. As the usage of amiodarone increased in regular practice it is important to be aware of a possible early onset amiodarone induced pulmonary toxicity.
References
- Dusman RE, Stanton MS, Miles WM, et al. Clinical features of amiodarone-induced pulmonary toxicity. Circulation 1990; 82:51â??59.
- Martin WJ, Rosenow EC. Amiodarone pulmonary toxicity. Recognition and pathogenesis (Part I). Chest 1988; 93:1067â??1075.
- Martin WJ, Rosenow EC. Amiodarone pulmonary toxicity. Recognition and pathogenesis (Part 2). Chest 1988; 93:1242â??1248.
- Ernawati DK, Stafford L, Hughes JD. Amiodarone-induced pulmonary toxicity. Br J Clin Pharmacol 2008; 66:82â??87.
- Jang WJ, Chon HR, Jung JS, et al. Amiodarone-induced pulmonary toxicity within a short period of the initiation of amiodarone therapy: A case report. Korean J Crit Care Med 2011; 26:117â??121.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Boddepalli Madhuri*, Umashankar, A Sankar, Kanmani and Raviteja Reddy
Department of General Medicine, Sree Balaji Medical College and Hospital, Chrompet, IndiaReceived: 20-Aug-2022, Manuscript No. jrmds-22-75329; , Pre QC No. jrmds-22-75329(PQ); Editor assigned: 22-Aug-2022, Pre QC No. jrmds-22-75329(PQ); Reviewed: 06-Sep-2022, QC No. jrmds-22-75329(Q); Revised: 09-Sep-2022, Manuscript No. jrmds-22-75329(R); Published: 16-Sep-2022
