Case Report - (2023) Volume 11, Issue 1
A Rare Case of Mitochondrial Neurogastrointestinal Encephalopathy
Hamsa VS*, Harivasudevan, Jagadeeshwari and Sundari
*Correspondence: Hamsa VS, Department of Paediatrics, Sree Balaji Medical College and Hospital Chrompet, Chennai, Tamil Nadu, India, Email:
Abstract
Mitochondrial Neuro Gastrointestinal Encephalopathy (MNGIE) is rare genetic disorder. It is characteristic by progressive gastrointestinal dysmotility, cachexia, opthalmoplegia and leucoencephalopathy. We hereby report a case of MNGIE in a female.
Keywords
Mitochondrial, Neurogastrointestinal, Encephalopathy, Leucoencephalopathy, Dysmotility
Introduction
It mainly affects the gastrointestinal tract and central nervous system. Clinical features starts at the age of 20 years and progressive in nature [1]. Dysmotility of gastrointestinal tract seen in majority of cases in MNGIE, is a condition in which there is a difficulty in passage of food due to inactivation of muscles and nerves leads to early fullness, difficulty in swallowing, heartburns, nausea, vomiting after eating, pain in the abdomen, bloating and loose stools.
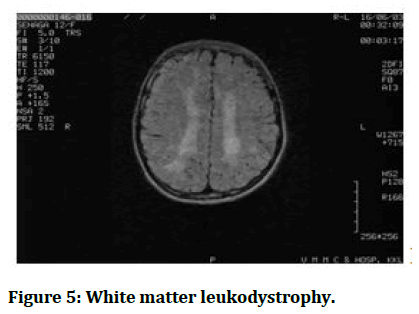
Generally patient diagnosed with MNGIE can have loss of appetite, lose weight, ptosis, ophthalmoplegia, auditory impairment, Tingling, paraesthesia, numbness, weakness of lower limbs. In MNGIE there is depletion of white matter of brain tissue which is the classical features of this syndrome, mostly less common (leukoencephalopathy), due to the autosomal recessive inheritance of TYMP gene in MNGIE which is an essential gene for maintaining proper level of mitochondrial thymidine [1,2].
Blood levels of thymidine and deoxyuridine is raised in this syndrome and it’s diagnosed by identification of variations in TYMP gene. Symptomatic management is the choice of treatment which includes maintaining the airway, teaching new swallowing techniques, focal management for nausea vomiting and neuropathic features. Further management incorporate diet support, antibiotics for bacterial infection in intestine, aided education and physical therapy like exertion, exercise [2] following medication chloramphenicol, tetracycline linezolid, valproate, phenytoin and aminoglycosides should be avoided due to hindrance of mitochondrial function [3].
Case Presentation
12 years female child of 3rd degree consanguineous parents came with complaints of abdominal discomfort, slurred speech, hearing disturbance, loss of weight for 7 years.
On examination: Child had opthalmoplegia, ptosis, B/L mixed hearing loss, slurred speech and cachexia (Figures 1 and 2).
Figure 1: A 12-years-old female patient opthalmoplegia, ptosis.
Figure 2: Cachexia.
Per abdomen examination: Visible gastric peristalsis seen (Figure 3).
Figure 3: Visible gastric peristalsis.
Investigation
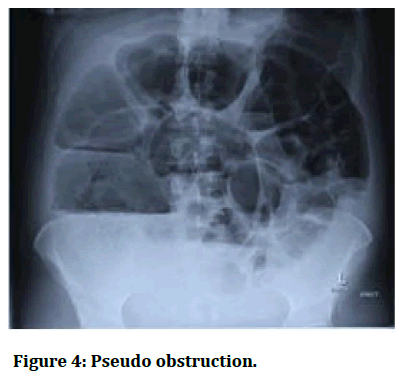
USG abdomen shows hypoplastic uterus. X-ray abdomen shows pseudo-obstruction (Figure 4). MRI shows white matter leukodystrophy (Figure 5).
Hormonal assay shows elevated LH and FSH, serum lactate and CSF lactate pyruvate is increased.
Figure 4: Pseudo obstruction.
Figure 5: White matter leukodystrophy.
Muscle biopsies: Ragged red fibre in gomoritrichrome stain.
Discussion
Diagnosis of MNGIE is made in the child by the presence of h/o consanguinity, clinical findings and neuroimaging [4].
CSF protein and lactate are raised and muscle biopsies: Ragged red fibre in gomoritrichrome stains [5].
Muscle biopsies: Ragged red fibre in gomoritrichrome stain. Molecular genetic testing for routine TYMP gene mutation has been sent, reports awaited [6].
Conclusion
Mitochondrial Neuro Gastrointestinal Encephalopathy (MNGIE) is rare genetic disorder. It is characteristic by progressive gastrointestinal dysmotility, cachexia, opthalmoplegia and leucoencephalopathy. We hereby report a case of MNGIE in a female.
References
- Hirano M, Marti R, Spinazzola A, et al. Thymidine phosphorylase deficiency causes MNGIE: An autosomal recessive mitochondrial disorder. Nucleosides Nucleotides Nucleic Acids 2004; 23:1217-1225. [Crossref][Googlescholar][Indexed]
- Hirano M, Silvestri G, Blake DM et al. Mitochondrial Neuro Gastro Intestinale Encephalomyopathy (MNGIE): Clinical, biochemical and genetic features of an autosomal recessive mitochondrial disorder. Neurology 1994; 44:721-727.
- Hirano M. Mitochondrial neurogastrointestinal encephalopathy disease. 2005. [Googlescholar][Indexed]
- Giordano C, Sebastiani M, Plazzi G, et al. Mitochondrial neurogastrointestinal encephalomyopathy: Evidence of mitochondrial DNA depletioin the small intestine. Gastroenterology 2006; 130:893–901. [Crossref][Googlescholar][Indexed]
- Martí R, Spinazzola A, Tadesse S, et al. Definitive diagnosis of mitochondrial neurogastro intestinal encephalomyopathy by biochemical assays. Clin Chem 2004; 50:120–124. [Crossref][Googlescholar][Indexed]
- Nishino I, Spinazzola A, Hirano M. Thymidine phosphorylase gene mutations in MNGIE, a human mitochondrial disorder. Science 1999; 283:689-692. [Crossref][Googlescholar][Indexed]
Author Info
Hamsa VS*, Harivasudevan, Jagadeeshwari and Sundari
Department of Paediatrics, Sree Balaji Medical College and Hospital Chrompet, Chennai, Tamil Nadu, IndiaCitation: Hamsa VS, Harivasudevan, Jagadeeshwari, Sundari, A Rare Case of Mitochondrial Neurogastrointestinal Encephalopathy, J Res Med Dent Sci, 2023, 11 (1):296-298
Received: 29-Jul-2022, Manuscript No. JRMDS-22-57353; , Pre QC No. JRMDS-22-57353 (PQ); Editor assigned: 01-Aug-2022, Pre QC No. JRMDS-22-57353 (PQ); Reviewed: 16-Aug-2022, QC No. JRMDS-22-57353; Revised: 03-Jan-2023, Manuscript No. JRMDS-22-57353 (R); Published: 13-Jan-2023