Case Report - (2022) Volume 10, Issue 5
A Rare Case with Bilateral Fracture of Condylar and Coronoid Processes of the Mandible including Symphysis
Ganiga Channaiah Shivakumar*, Preeti P Nair, Annette M Bhambal, Rashmi Sathe, Palak Choudhary, Vikalp Raghuvanshi, Akhil Trivedi and Priyanka Deshmukh
*Correspondence: Ganiga Channaiah Shivakumar, Department of Oral Medicine and Radiology, People’s College of Dental Sciences and Research Centre, People’s University, Bhopal, India, Email:
Abstract
Fractures are common in the maxillofacial region of the human body because of the maximum exposure to trauma. The trauma received can be due to road accidents, sports injuries, physical assault, etc. the nasal bone being the commonest site prone to fractures followed by mandible. In mandible condyles are the commonly involved sites with fractures; others being dent alveolar region, parasymphyseal area, angle, ramus, and the body of the mandible. Owing to its strategic location depth and muscle coverage coronoid processes are spared. To ascertain the fracture site, dental radiology plays a great role. Currently, besides the conventional extraoral radiography, advanced modalities like Cone Beam Computed Tomography (CBCT), Computed Tomography (CT) are preferred for an improved fracture diagnosis and management. We report a case of a young female who received multiple maxillofacial fractures, after meeting with a tragic road accident.
Keywords
Cone-beam computed tomography, Condyle, Coronoid, Fracture
Introduction
The maxillofacial region is the most common part of the body to be affected by trauma, causing fractures. Mandible, owing to its position and prominence, is the second most common site of the maxillofacial skeleton, prone to fractures [1-2]. Thirty-five per cent of mandibular fractures occur between the ages of 20 to 30 years. Mandibular fractures may destabilize the airway and lead to malocclusion, joint dysfunction, pain, infection, and paresthesia. Condyle fractures are considered the most common fracture of the mandible and are divided into the head, neck, and sub-condylar regions. The slender neck of the mandibular condyle renders it particularly liable to fracture making its incidence very high. Most are not caused by direct trauma but follow indirect forces transmitted to the condyle from an impact. According to available literature and studies reported, condylar fracture constitutes about 25%-50% [3-4]. Although the coronoid process is a relatively weak part of the mandible, its fracture is difficult due to its strategic location and muscle coverage. Therefore, fractures of the mandibular coronoid process are rare constituting about 0.6 to 4.7% of all facial fractures making the coronoid process the least frequently fractured region of the mandible [5-6]. Most coronoid fractures are a result of indirect blunt or penetrating trauma. Various other possible iatrogenic factors causing fractures of the coronoid process can be a resultant of extractions of third molars, sagittal split osteotomy, and cystectomies [7]. Symphyseal and parasymphyseal fractures are usually caused by direct traumatic impact to the chin. Mandibular symphyseal fracture accounts for 15.6 to 29.3% of mandibular fractures [8-9]. Before the introduction of Conventional Tomography (CT) in the 1980 s, two-dimensional (2D) radiographic images were utilised for assessing the maxillofacial injuries. With the advent of three-dimensional (3D) technologies, the concept to visualize the maxillofacial region in dental radiology practice has changed and improved. However, CBCT may be considered the technology that has had the greatest impact on maxillofacial imaging over the past decade.
Available literature suggests no reports of bilateral fractures of both condylar and coronoid process of the mandible. We report an extremely rare case of the same along with other maxillofacial fractures suffered by the patient, using advanced imaging technologies like CBCT and CT for a confirmed radio diagnosis.
Case Presentation
A 27 yrs. the old female patient reported to the Department of Oral Medicine and Radiology, Peoples College of Dental Sciences and Research Center, Bhopal, India with the chief complaint of pain and difficulty in opening the jaw. She has sustained a trauma to the chin in a road accident one day before. Past medical history was non-contributory. Clinical examination of the head and neck revealed positive physical findings of multiple lacerations and edema to the lower lip abrasions on the chin and cheek region. No facial palsy was observed. TMJ examination revealed restricted mouth opening, lateral excursive movements, and tenderness over the temporomandibular joint and temporal region bilaterally, on palpation. Intraoral examination showed occlusal disharmony, mobility of 11, 31, 32, 41, 42, and avulsion of 12 and 22. Investigatory findings like complete blood count, hemoglobin levels, serology, and urine analysis were within normal limits.
On radiological investigations, as evident in Figure 1, the Orthopantomogram (OPG) revealed a sharply defined radiolucent line extending from right sigmoid notch to the posterior ramus region. Step deformity notch with the left condylar head was observed. Horizontal radiolucent lines are seen in relation with right and left coronoid processes. The symphyseal region reveals two radiolucent lines, one running vertically between the apices of 31 and 41, whereas other horizontally below the apices of 41,42 (Table 1).
Table 1: Radiographic report of the case.
| Structure | Findings |
|---|---|
| Maxillary findings include: | Dentoalveolar fracture is seen in left anterior maxilla extending from the alveolar crest to involve floor of the left maxillary sinus. |
| Hyperdensity noted in left maxillary sinus suggestive of hemosinus. | |
| Zygomatic arches appear normal. | |
| Mandibular findings include: | Dentoalveolar fracture is seen in mandible anterior region extending from crest to inferior border of the mandible (correlated from OPG, not in FOV of CBCT). |
| Bilateral coronoid and condylar fracture. |
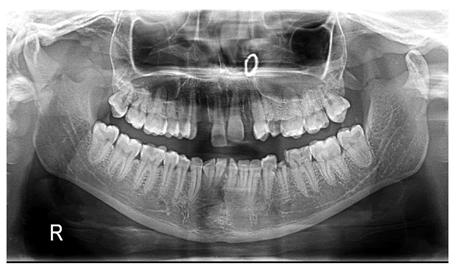
Figure 1: Orthopantomogram image showing bilateral fracture of condyle and coronoid processes and symphysis region.
To evaluate the status of the maxillary complex and involvement of the orbital area, and a better appreciation of the mandibular fractures, CBCT was advised. As depicted in Figure 2 the CBCT images revealed a bilateral fracture of both coronoid and condylar processes by mandibular findings include (Figure 2):
- Dentoalveolar fracture is seen in mandible anterior region extending from crest to inferior border of the mandible (correlated from OPG, not in FOV of CBCT).
- Bilateral coronoid and condylar fracture.
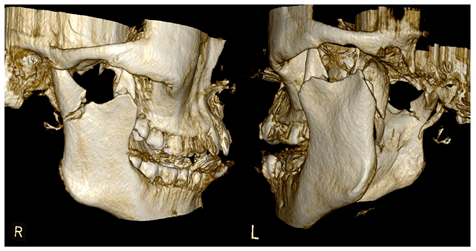
Figure 2: 3D CBCT image showing bilateral fracture of condyle and coronoid processes.
Maxillary findings include (Figures 3 and 4):
Dentoalveolar fracture is seen in left anterior maxilla extending from the alveolar crest to involve floor of the left maxillary sinus.
Hyperdensity noted in left maxillary sinus suggestive of hemosinus.
Zygomatic arches appear normal.
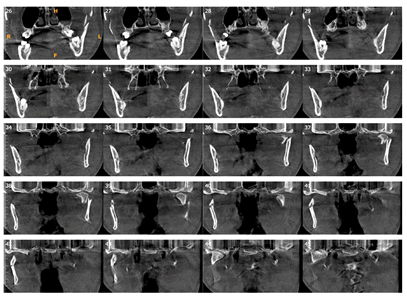
Figure 3: Coronal sections of CT image.
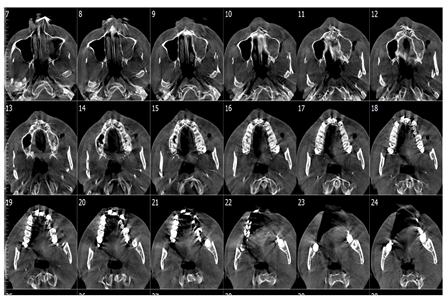
Figure 4: Axial sections of CT image.
Radiographic impression was of multiple maxillofacial fractures. For a more enhanced view of the condylar and coronoid neck fractures, CT scans were done of the concerned region only to confirm the radiodiagnosis. The scans also revealed a clear image of bilateral fractures in the condylar and coronoid processes of the mandible. After a complete evaluation, the patient was planned for conservative management. In oral surgery department, under nasal intubation, maxillary and mandibular dental arches were stabilized using arch bars and the Inter-Maxillary Fixation (IMF) was carried out using elastic bands and ligatures. The fractures were rectified and bones were repositioned accordingly while considering the correct establishment of the patient's occlusion status. Muscle relaxants were prescribed to the patient, and thermotherapy (dry heat application for 10 min) with manual massage was advised to the patient. A soft diet was to avoid excessive masticatory load was advised. The patient was followed-up postoperatively to observe for any esthetic or functional problems.
Result And Discussion
The potent causes of maxillofacial trauma include traffic accidents, home accidents, falls, sports injuries, domestic violence, work-related injuries, and sexual abuse. Young men aged 16 to 30 years are more prone to physiological traumatic events, double the rate of young women of the same age [10]. Facial injuries may not only affect the dentition but also the adjacent tissues, thus causing a range of fractures from isolated to complex ones [11]. Mandibular fractures can occur horizontally in the dentoalveolar area and vertically at the angle, ramus, condyle or coronoid processes. The most common fracture sites being the condyle, body, and angle, followed by less frequent sites being parasymphysis, ramus, coronoid process, and the alveolar crest [12]. Mandibular fractures form approximately 2/3rds of all the maxillofacial fractures. The site and pattern of a fracture are determined by the mechanism of injury and the direction of force applied. Additionally, the patient’s age, the status of the dentition, and the traumatic impact influence the characteristics of the resultant injury [13]. Coronoid fractures due to direct trauma are very uncommon because of their protected position under the zygomaticomalar complex [14]. The fracture of the coronoid process mostly results from direct, penetrating trauma or if there occurs concomitant sudden and violent contraction of the temporalis muscle at the time of impact [15]. A direct blow to the chin region can lead towards a fracture of one or both condyles. A blow from the side can cause fracture of the opposite condylar neck along with parasymphysis fracture at the ipsilateral side of the blow [16]. Showed that no isolated coronoid fracture was observed and the most frequently observed associated maxillofacial fracture was zygomatic (46.4%). However, mandibular complex fractures can also occur in absence of any trauma, possibly abnormal muscle contractions reported a similar case of unilateral right subcondylar and coronoid fractures without any presence of direct or indirect trauma [17].
The diagnosis and handling of maxillofacial fractures are based on the clinical and radiographic evaluation. Currently, there is no "gold standard" for mandibular fracture imaging. The radiological diagnosis of a fracture of the coronoid process is not always easy to make, and the fracture may go undetected because of inappropriate radiographs. Conventional radiographic methods like OPGs are not sufficient to detect coronoid fractures and even the status evaluation of the orbital complex and maxilla is hampered. Artefact issues and superimposition of images makes it necessary to go in for other extraoral radiographs like Temporomandibular Joint (TMJ) views, Sub Mento Vertex (SMV) skull views and advanced techniques to detect maxillo-mandibular facial fractures. Intraoral and extraoral radiographs are often unable to reveal cortical plate fractures, and it may be difficult to differentiate a tooth fracture from an overlapping alveolar fracture, similar to our case. Additionally, nondisplaced fractures of the mandibular condyle can be very difficult to diagnose with conventional imaging techniques; therefore, it is important to supplement them with advanced imaging techniques such as CBCT. Multiplanar imaging procedures like Cone Beam Computed Tomography (CBCT) is an imaging option that improves fracture diagnosis [18-19]. CBCT has proven to be superior to conventional dental radiography, especially in the detection of the fractures of the condyle, coronoid processes and in the anterior section of the mandible. Considering the above, we also went for a CT and CBCT examination of the patient failing to identify other fractures suffered by the patient. Apart from the mandibular fractures, CBCT scans also revealed a dentoalveolar fracture of the anterior maxilla and hemosinus of the left maxillary sinus that could not be detected in OPG accurately. Similar to our case Yilmaz SY diagnosed a case of the maxillofacial trauma patient with maxillary sinus fracture using CBCT [20]. Heiland stated that the use of CBCT for preoperative, intra-operative, and postoperative imaging can decrease radiation doses in cases of zygomatico-maxillary complex fractures, while CT crucial in cases of severe traumatic injuries [21]. Since the advent of CT scans, it is no longer difficult to correctly diagnose a coronoid fracture and CBCT seems to be a good complementary for panoramic radiography in trauma cases, making it a great radiological tool to detect dentoalveolar fractures.
Conclusion
Dental radiographic evaluation is a key step in the diagnosis and management of dento-maxillofacial trauma. The increasing beneficial use of CBCT in the evaluation of facial structures following maxillofacial trauma helped detect multiple dentoalveolar, bilateral condylar and coronoid fractures in our patient. The presence of bilateral coronoid fractures makes it a rare case to be reported in the literature.
References
- Ogundare BO, Bonnick A, Bayley N. Pattern of mandibular fractures in an urban major trauma center. J Oral Maxillofac Surg 2003; 61:713-718. [Crossref][Google Scholar][Pubmed]
- Thaller SR. Management of mandibular fractures. Arc Otolaryngol Head Neck Surg 1994; 120:44-48. [Google Scholar]
- Olson RA, Fonseca RJ, Zeitler DL, et al. Fractures of the mandible: a review of 580 cases. J of Oral Maxillofac Surg 1982; 40:23-28. [Crossref][Google Scholar][Pubmed]
- Shakya S, Zhang X, Liu L. Key points in surgical management of mandibular condylar fractures. Chin J Traumat 2020; 23:63-70. [Crossref] [Google Scholar][Pubmed]
- Oliveira DM, Vasconcellos RJ, Laureano Filho JR, et al. Fracture of the coronoid and pterygoid processes by firearms: case report. Braz Dent J 2007; 18 :168-170.
- Shen L, Li J, Li P, et al. Mandibular coronoid fractures: Treatment options. Int J Oral Maxillof Surg 2013; 42:721-726. [Crossref] [Google Scholar][Pubmed]
- Farish SE. Iatrogenic fracture of the coronoid process: report of case. J Oral Surg 1972; 30:848-850. [Google Scholar][Pubmed]
- Dongas P, Hall GM. Mandibular fracture patterns in Tasmania, Australia. Aust Dent J 2002; 47:131-137.
- Motamedi MH. An assessment of maxillofacial fractures: a 5-year study of 237 patients. J Oral Maxillofac Surg 2003; 61:61-64.
- Yun PY, Kim YK. The role of facial trauma as a possible etiologic factor in temporomandibular joint disorder. J Oral Maxillofac Surg 2005; 63:1576-83.
- Aydin U, Gormez O, Yildirim D. Cone-beam computed tomography imaging of dentoalveolar and mandibular fractures. Oral Radiol 2020; 36:217-224.
- Lam EWN. Trauma. In: White SC, Pharoah MJ, editors. Oral radiology principles and interpretation. 7th ed. St. Louis: Mosby; 2014: 562–581.
- Fasola AO, Obiechina AE, Arotiba JT. Incidence and pattern of maxillofacial fractures in the elderly. Int J Oral Max Surg 2003; 32:206-208.
- Zachariades N, Mezitis M, Mourouzis C, et al. Fractures of the mandibular condyle: a review of 466 cases. Literature review, reflections on treatment and proposals. J Cran Max Surg 2006; 34:421-432. [Crossref] [Google Scholar][Pubmed]
- Philip M, Sivarajasingam V, Shepherd J. Bilateral reflex fracture of the coronoid process of the mandible. A case report. Int J Oral Maxillofac Surg 1999; 28:195-196. [Crossref] [Google Scholar][Pubmed]
- Boffano P, Kommers SC, Roccia F, et al. Fractures of the mandibular coronoid process: a two centres study. J Cran Max Surg 2014;42:1352-1355. [Crossref] [Google Scholar][Pubmed]
- Shintaku W H, Venturin J S, Azevedo B, et al. Applications of cone-beam computed tomography in fractures of the maxillofacial complex. Dent Traumatol. 2009; 25 :358–366. [Crossref] [Google Scholar] [Pubmed]
- Yilmaz SY, Misirlioglu M, Adisen MZ. A Diagnosis of Maxillary Sinus Fracture with Cone-Beam CT: Case Report and Literature Review. Craniomaxillofac Trauma Reconstr 2014; 7:85-91. [Crossref] [Google Scholar][Pubmed]
- Heiland M, Schulze D, Blake F, et al. Intraoperative imaging of zygomaticomaxillary complex fractures using a 3D C-arm system. Int J Oral Maxillofac Surg 2005; 34:369–375. [Crossref][Google Scholar] [Pubmed]
- Pohlenz P, Blake F, Blessmann M, et al. Intraoperative cone-beam computed tomography in oral and maxillofacial surgery using a C-arm prototype: first clinical experiences after treatment of zygomaticomaxillary complex fractures. J Oral Max surg 2009; 67:515-21. [Crossref][Google Scholar][Pubmed]
- Pohlenz P, Blessmann M, Blake F, et al. Clinical indications and perspectives for intraoperative cone-beam computed tomography in oral and maxillofacial surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103:412-417. [Crossref]
Author Info
Ganiga Channaiah Shivakumar*, Preeti P Nair, Annette M Bhambal, Rashmi Sathe, Palak Choudhary, Vikalp Raghuvanshi, Akhil Trivedi and Priyanka Deshmukh
1Department of Oral Medicine and Radiology, People’s College of Dental Sciences and Research Centre, People’s University, Bhopal, IndiaCitation: Ganiga Channaiah Shivakumar, Preeti P Nair, Annette Bhambal, Rashmi Sathe, Palak Chaudhary, Vikalp Raghuvanshi, Akhil Trivedi, Priyanka Deshmukh, A Rare Case with Bilateral Fracture of Condylar and Coronoid Processes of the Mandible including Symphysis , J Res Med Dent Sci, 2022, 10(5): 109-112.
Received: 23-Feb-2022, Manuscript No. 47730; , Pre QC No. 47730; Editor assigned: 25-Feb-2022, Pre QC No. 47730; Reviewed: 11-Mar-2022, QC No. 47730; Revised: 25-Apr-2022, Manuscript No. 47730; Published: 05-May-2022
