Case Report - (2019) Volume 7, Issue 1
A Rare Manifestation of Subarachnoid Hemorrhage: Case Report
Vafadar Moradi Elnaz1, Bahar Vahdat Humain2, Rezvani Kakhki Behrang1*, Habibzadeh Seyed Reza1 and Sadrzadeh Sayyed Majid1
*Correspondence: Rezvani Kakhki Behrang, Department of Emergency Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran, Email:
Abstract
Bleeding is a critical sign in many patients and continues or recurrent hemorrhage leads to emergency department (ED) visits. Epistaxis alone is a common problem, but when it presented with simultaneous otorrhagia become a very unpleasant event. Spontaneous epistaxis and otorrhagia necessitate imaging assessment to identification of underlying cause. A ruptured aneurysm or a possible underlying SAH should be evaluated by brain Computed Tomography. Advance diagnostic modalities for detection of underlying cause of SAH include: Computed Tomography Angiography, Magnetic Resonance Angiography and Digital Subtraction Angiography. A 57-years-old woman was referred to our tertiary hospital emergency department (ED) with otorrhagia and epistaxis. She had no history of headache, head trauma, hypertension and drug usage. In physical examination her vital signs were normal and Glasgow Coma Scale score on admission was 15. She had bilateral epistaxis and neurologic examination revealed no pathologic findings. ENT consultation was done, otoscopy reveal a normal tympanic membrane with bloody otorrhagia in the left external auditory canal. The epistaxis stop spontaneously and there was no findings, on nose examination. She underwent further investigation for intracranial aneurysm or hemorrhage. Brain CT scan was performed and showed Sub Arachnoids Hemorrhage (SAH). She was candidate for brain CT angiography, which was normal. The patient, discharged from hospital after 1 week with stable vital sign and normal Brain CT scanning.
Keywords
Hemorrhage, CT scanning, Epistaxis
Introduction
Bleeding is a critical sign in many patients and continuous or recurrent hemorrhage leads to emergency department (ED) visits [1]. Epistaxis alone is a common problem, but when it presents with simultaneous otorrhagia become a very unpleasant event [2,3]. In the absence of trauma history, bloody otorrhagia is an uncommon event [3]. Spontaneous epistaxis and otorrhagia necessitate imaging assessment to identification of underlying cause [3]. Ruptured aneurysm of extra cranial internal carotid may be presented by severe otorrhagia [4]. A ruptured aneurysm or a possible underlying SAH should be evaluated by brain Computed Tomography [4]. Spontaneous subarachnoid haemorrhage (SAH) is defined by hemorrhage in the subarachnoid space, and this event is usually due to the presence of concealed vascular disease [5]. The initial symptom of these patients is a sudden onset severe headache; nevertheless dizziness, vertigo, neck pain, nausea and vomiting are frequent clinical presentation, associated with sudden onset headache [6]. The brain Computed Tomography is the first modality of choice to evaluate these patients [6]. Advance diagnostic modalities for detection of underlying cause of SAH include; Computed Tomography Angiography, Magnetic Resonance Angiography and Digital Subtraction Angiography [7]. Despite some limitation of CTA, it can provide multi directional view from aneurismal morphology and its surrounding [7]. In 8%-10% of patients with SAH, there is no underlying cause such as aneurysm or vascular malformation [6].
Case Presentation
A 57-years-old woman was presents to our Emergency Department with chief complain of spontaneous otorrhagia and epistaxis. She said that she was asleep and suddenly had spontaneous epistaxis and otorrhagia. She had no history of headache, head trauma, hypertension and medication usage. On initial admission and physical examination her vital signs were: Blood Pressure: 110/78 mmhg, Pulse Rate: 80/min, Respiratory Rate: 16/ minute, O2 Saturation in air room: 96% and Glasgow Coma Scale score on admission was 15. She had bilateral epistaxis and otorrhagia from right ear. Laboratory tests were performed. Her hemoglobin was 14 and PT: 11 second, INR: 1, PTT: 25 second and PTT ratio: 36 second. Bleeding time (BT) was 5 minutes. ENT consultation was done, otoscopy reveal a normal tympanic membrane with bloody otorrhagia in the left external auditory canal. The epistaxis stop spontaneously and there was no finding on nose examination. The decision was made to take brain computed tomography with and without intravenous contrast agent. The brain spirals axial brain CT scanning without contrast had shown spontaneous subarachnoid hemorrhage (SAH) in the upper right hemisphere (Figure 1) and brain CT angiography was normal (Figure 2). Clinically Hunt Hess Grade 1 and other neurologic examination revealed no pathologic findings.
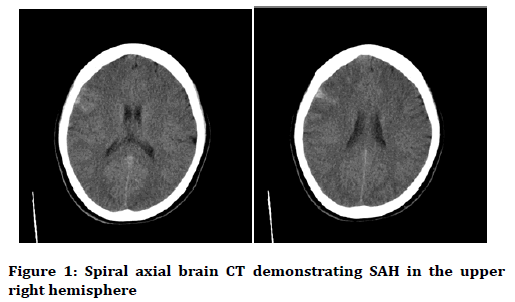
Figure 1. Spiral axial brain CT demonstrating SAH in the upper right hemisphere
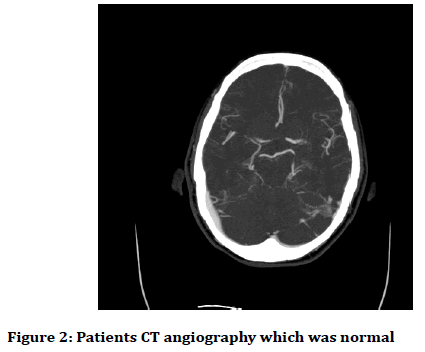
Figure 2. Patients CT angiography which was normal
She was admitted in neurosurgical intensive care unit and discharged home after 7 days with GCS score 15 and no focal neurologic deficient. Epistaxis and otorrhagia were controlled.
Discussion
We report a rare manifestation of SAH in middle-aged woman. Otorrhagia in seldom found with limited literature available [8]. History of a trauma in these patients is very important, and some time otorrhagia is secondary to skull fracture [8]. Simultaneous presentation of epistaxis and otorrhagia is a rare clinical finding. More than one site of bleeding can be an important sign for many critical situations. Relationship between the clinical presentation and the SAH is key in this case report and should be developed as for the etiology of the SAH. It is likely at the moment of the bleeding, the patient developed a sudden increase in blood pressure which might have induced the epistaxis. Regarding the cause of otorrhagia, emphasis should be made that it was from the external duct, thus unrelated to the SAH itself but to its related condition (vascular malformation of the external canal that bleed after a sudden increase in blood pressure?).
As for the etiology of this cortical SAH, Reversible Cerebral segmental Vasoconstriction could be hypothesized despite normal CT angiogram and cerebral angiography.
Trans cranial Doppler could be of interest in the diagnosis of Reversible Cerebral segmental Vasoconstriction. Epistaxis and otorrhagia can be first manifestation of hereditary hemorrhagic telangiectasia (HHT) and should be fully evaluated [9].
Giacobbe et al. also have reported a rare case report of an otorrhagia and epistaxis during hysteroscopy due to intravascular absorption syndrome (IVA) which developed during hysteroscopy with glycine [1]. An internal carotid aneurysm also may cause otorrhagia, these patients also have tinnitus or conductive hearing loss and CTA is a technique of choice to evaluate these patients [1]. Our patient does not have a history of a head trauma, surgery, hearing loss or HHT. Because there is no source of bleeding on the primary evaluations, the decision was made to take brain computed tomography with and without intravenous contrast agent and brain CT revealed SAH in right hemisphere of the brain. Naganuma et al. have reported that 8%-10% of their cases with SAH had no headache at the time of admission in the ED [10]. Actually, typical symptoms other than headache, like our patient, abundantly reported recently. Our patient had a rare manifestation of SAH; she had spontaneous epistaxis and otorrhagia.
History taking is a crucial part of evaluating patients with bleeding, previous history of coagulopathy or craniofacial trauma. Coagulopathy is another probable pathology in these cases and should be rolled out with laboratory investigation and previous history. In our case normal platelet count, normal BT and normal range PT and INR were reported.
Cerebral CT angiography in our patients showed no aneurysm, arteriovenous malformation.
Our patient has a rare manifestation of SAH, and she has no pathological findings on brain CT and CTA. In these situations, cerebral angiography may be helpful to determine small aneurysm but our patient did not give consent for cerebral angiography.
Conclusion
Epistaxis and otorrhagia should never be neglected in any patients and further investigations including imaging and laboratory tests should have performed.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this manuscript.
References
- Giacobbe V, Rossetti D, Vitale SG, et al. Otorrhagia and nosebleed as first signs of intravascular absorption syndrome during hysteroscopy: From bench to bedside. Kathmandu Univ Med J 2016; 14:87-9.
- Davies K, Batra K, Mehanna R, et al. Pediatric epistaxis: Epidemiology, management & impact on quality of life. Int J Pediatr Otorhinolaryngol 2014; 78:1294-7.
- Boyar C, Chao W. Spontaneous bilateral epistaxis and bilateral otorrhagia in a five-year-old with tympanostomy tubes. Pediatr Emerg Care 1995; 11:179-80.
- Kopanky D, Spetzler RF, Bonstelle C. Severe otorrhagia resulting from a ruptured aneurysm of extra cranial internal carotid artery. Surg Neural 1981; 15:141-3.
- Long B, Koyfman A, Runyon MS. Subarachnoid hemorrhage update in diagnosis and management. Emerg Med Clin 2017; 803-24.
- Ogasawara Y, Ito K, Ohkuma H. Atypical presentation of aneurysmal subarachnoid hemorrhage: Incidence and clinical importance. J Stroke Cerebrovasc Dis 2016; 25:1208-14.
- Kumar A, Kato Y, Hayakawa M, et al. Recent advances in diagnostic approach for sub-arachnoid hemorrhage. Asian J Neurosurg 2011; 6:94-8.
- Spano SJ, Burg M. An unusual case of otorrhagia. J Emerg Med 2012; 42:e149-50.
- Wirsching KEC, Haubner F, Kühnel TS. Influence of temporary nasal occlusion (TNO) on epistaxis frequency in patients with hereditary hemorrhagic telangiectasia (HHT). Eur Arch Otorhinolaryngol 2017; 274:1891-6.
- Naganuma M, Fujioka S, Inatomi Y, et al. Clinical characteristic of subarachnoid hemorrhage with or without headache. J Stroke Cerebrovasc Dis 2008; 17:334-9.
Author Info
Vafadar Moradi Elnaz1, Bahar Vahdat Humain2, Rezvani Kakhki Behrang1*, Habibzadeh Seyed Reza1 and Sadrzadeh Sayyed Majid1
1Department of Emergency Medicine, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran2Department of Neurosurgery, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
Citation: Vafadar Moradi Elnaz, Bahar Vahdat Humain, Rezvani Kakhki Behrang, Habibzadeh Seyed Reza, Sadrzadeh Sayyed Majid, A rare manifestation of subarachnoid hemorrhage: Case report, J Res Med Dent Sci, 2019, 7(1): 178-180.
Received: 24-Jan-2019 Accepted: 08-Feb-2019
