Research - (2021) Volume 9, Issue 5
A Study of Colorectal Carcinoma, Pathological Variants, and its Staging for Their Significance
*Correspondence: Shoba T, Department of Pathlogy, Sree Bharath Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email:
Abstract
A study of colorectal carcinoma along with different histopathological variants. To study the staging of colorectal carcinoma and the significance of histopathological variants of colorectal carcinoma. The large bowel comprises the terminal 1 to 1.5m of the gastrointestinal tract and is divided into caecum, ascending colon, transverse colon, descending colon, sigmoid colon, and rectum. The hepatic flexure is at the junction of the ascending and transverse colon, and the splenic flexure is at the junction of the transverse and descending colon. The rectum forms the distal 8 to 15cm of extra peritoneal large bowel wall. There are two major functions of the colon and rectum. The colon absorbs water and minerals from blood and transports them into the bloodstream. The rectum stores faecal matter until it is eliminated from the body through the anus. Both organs are essential to the digestive process Caecum, ascending colon and right two thirds of transverse colon are derived from midgut and left one third of transverse colon, descending colon, pelvic colon and rectum are derived from hind gut.
Keywords
Midgut, Dysplasia, Colorectal carcinoma, Polyposis.
Introduction
Colorectal cancer is the third most common cancer in males (663,000 cases 10.0% of total cases) and second in females (570,000 cases 9.4% of total cases) worldwide [1]. Within Asia, the incidence rate of colorectal cancer varies widely and are uniformly low in all South Asian countries and high in all developed Asian countries. The incidence rate of colorectal cancer in India among males 4.3/100000 and in females 3.4/100000. The burden of colorectal cancer has risen rapidly in some economically developed Asian countries like Japan, South Korea, Singapore [2]. According to the American Cancer Society about 104,950 new cases of colon cancer and 40,340 new cases of rectal cancer were reported in 2005 in the United States combined, the two cancer types have caused about 56,290 deaths [3]. According to the World Health Organization April 2003 report on global cancer rates more than 940,000 new cases of colorectal cancer and nearly 500,000 deaths are reported worldwide each year. Incidence of colon carcinoma is highly variable worldwide, most common m northwest Europe, North America, and Australia and low in Africa, Asia and some parts of South America. It is by far the most common and most curable carcinoma of the gastrointestinal tract. However, the incidence is rising in countries that are adopting western lifestyle, for30-55 per I 00,000 by contrast in Africa it is only 5 per I 00,000. Epidemiologic studies indicate that the etiology of sporadic colorectal carcinoma is closely related to the environmental factors with genetic factors playing an important but less obvious role. The former is largely dietary particularly in terms of fats and animal proteins and lack of fiber and fresh vegetables [4,5]. One hypothesis indicates that excess dietary fat may result in increased production of bile acids which may themselves be carcinogenic or may be converted to carcinogen by the action of bacteria in the bowel lumen.
Male sex, increasing age, presence of long standing IBD and familial predisposition are strong risk factors. Mean age of incidence is 62 years. Cancer is mostly age related, the incidence rising progressively with increasing age. In highrisk areas 8% of patients present under the age of 50 years, prognosis of young patient differs from that of more elderly subjects. The incidence is a little higher in males than females. Cancer of left colon is more frequent in females under the age of 5 years and more frequent in males over the age of 70 years. Cancer of right colon is age dependent in both males and females. In females 40% occur in right colon, 30% in left colon and 30% in rectum 6 Globally more than I million people get colorectal cancer yearly (studied in U.K), resulting in about 0.5 million deaths 8 (studied in USA) [6]. As of 2008 it is the second most common cause of cancer in women and the third most common in men 9 (studied in USA). According to world health organization, it is the fourth most common cause of cancer death after lung cancer [7,8].
The colon is a tubular structure of 30-40 ems in length at birth that reaches l .5mts in length in adults. Proximally it continues at ileocecal valve with small intestine and ends distally at anal verge. The external appearance of colon - the outer longitudinal muscle fiber coalesces into 3 discrete bands (teniae) located at 120 degrees interval about the colonic circumference [9]. The tenia starts at the base of appendix and run continuously to the proximal rectum. The outpouchings of the colon (haustra) separate the tenia. On the outside of the colon are fatty filled sacs of peritoneum called appendices epiploic or omental appendices. Ascending colon extends cranially from caecum for 12-20cms along the right side of the peritoneal cavity to the under surface of liver. At the hepatic flexure, the colon turns medially and anteriorly to emerge into the peritoneal cavity as the transverse colon 45cms in length and supports the greater momentum. Descending colon travels posteriorly and inferiorly in retroperitoneal compartment to the pelvic brim. There it emerges into the peritoneal cavity as a sigmoid colon. This is 'S' shaped redundant segment. Sigmoid colon, the narrowest portion of the colon (2-5cm diameter), explains why the tumors in this region may be symptomatic early [10-13].
Materials and Methods
Our present study was conducted at Sree Bharath Medical College and Hospital, Chennai for a period starting from July 2011 to June 2013. A two year study was done taking into account all the clinical details of the patients retrieved from the medical records section in the hospital. The clinical features, laboratory data, and detailed pathological examination of each case was analyzed.
The lesions were fixed in 10% formalin; and after careful observation with the naked eye, the lesion was cut into sections and stained with hematoxylin and eosin (H&E). All the· ides were reviewed, and the sections were examined histologically. The following staining procedures were also adopted. Special stains done for few cases where required.
Haematoxylin and eosin staining
Bring sections to water.
✓ Stain in Harris haematoxylin for 15 - 20 minutes.
✓ Remove excess of haematoxylin by keeping section in running water for 10 minutes followed by differentiation in 1% acid alcohol.
✓ Decolorizing acid is then removed by keeping in running tap water followed by bluing in lithium carbonate.
✓ Stain in eosin for 2 minutes.
✓ Dehydrate, clear and mount.
PAS staining for mucins
✓ Dewax and hydrate paraffin section.
✓ Oxidize for 5 minutes in 0.5% aqueous periodic acid.
✓ Rinse in tap and then in distilled water.
✓ Place in Schiff's reagent for 15minutes.
✓ Rinse for 2 minutes in each of three changes of freshly made sulfite rinse.
✓ Wash 5 to 10 minutes in running ta water.
✓ Counter stain with hematoxylin for 1-3minutes.
✓ Differientiate by means of three to five quick dips in 1% acid alcohol wash in tap water and blue in Scott's tap water substitute.
Alcian blue-pas staining for acid and neutral mucins Reagents
✓ Alcian blue-1 gm.
✓ Schiff 's reagent.
Method
✓ Dewax sections and bring water.
✓ Alcian blue solution 5min.
✓ Wash in water then in distilled water.
✓ 1 percent aqueous periodic acid 5min.
✓ Rinse well in distilled water.
✓ Schiff 'reagent 15 min.
✓ Wash in running tap water 5-l0min.
✓ Stain nuclei lightly with one of the usual hematoxylin solutions (not Ehrlich"s) differentiated as appropriate and blue.
✓ Wash in water.
✓ Rinse in absolute alcohol.
✓ Clear in xylene and mount with DPX.
Results
The present study of colorectal carcinoma was undertaken at Department of pathology, Sree Bharath Medical College and Hospital, Chennai for a period of two years (July 2010- June 2012). Total 57 cases were collected, and the observations are recorded, out of which 49 cases were adenocarcinoma, 7 cases of adenomatous polyps, and 1 case of adenosquamous carcinoma.
Table 1 shows various types of adenocarcinoma. 44 were conventional adenocarcinomas, 5 cases of adenomatous polyps associated with dysplasia, 2 cases of Familial adenomatosis polyposis, 4 cases of mucinous adenocarcinoma, 1 case adenosquamous carcinoma were seen. There was a slight male preponderance in adenocarcinoma and the peak incidence was in the 5th and 6th decade.
Table 1: The various types of colorectal cancers.
| Tumor type | Number | Percentage |
|---|---|---|
| Conventional adenocarcinoma | 44 | 77.69% |
| Polyps associated Dysplasia | 5 | 8.21% |
| Familial adenomatous polyposis | 2 | 3.40% |
| Mucinous adenocarcinma | 4 | 7.20% |
| Signet ring carcinoma | 1 | 1.75% |
| Adenosquamous carcinoma | 1 | 1.75% |
| Total | 57 | 100% |
Table 2 shows patients having adenocarcinoma presenting clinically with symptoms of pain abdomen 29.7%, bleeding per rectum 15.6%, anemia 26%, loss of appetite and loss of weight 10.2%, altered bowel habits 11.2%.
Table 2: The comparison of complaints with other study.
| Complaints | Hamiliton (2001-2006) | Percentage | Present study | Percentage |
|---|---|---|---|---|
| Bleeding per rectum | 853 | 15.60% | 51 | 89.47% |
| Pain in the abdomen | 1629 | 29.70% | 44 | 77.19% |
| Altered bowel habits | 615 | 11.20% | 41 | 71.92% |
| Anorexia, loss of weight | 561 | 10.20% | 32 | 56.14% |
| Anemia | 1424 | 26% | 29 | 50.87% |
| Blood & mucus in stools | - | 3 | 5.26% |
Present study shows symptoms of bleeding per rectum 89.47%, pain abdomen 77.19%, altered bowel habits 71.92%, anemia 50.87%, blood & mucus m stools 5.26%, anorexia & loss of weight 56.14.
Table 3 shows in the large intestines rectum 35 tumors were involved, rectosigmoicl 6 cases, sigmoid colon 3 cases, transverse colon 5 cases, anal canal 1 case, caecum 2 cases, same for ascending colon and descending colon, splenic flexure 1 case.
Table 3: Site wise incidence of colorectal cancers in present study.
| Site | Total | Percentage |
|---|---|---|
| Rectum | 35 | 61.4 |
| Rectosigmoid | 6 | 10.52 |
| Transverse Colon | 5 | 8.77 |
| Sigmoid Colon | 3 | 5.56 |
| Ascending Colon | 2 | 3.5 |
| Decending Colon | 2 | 3.5 |
| Caecum | 2 | 3.5 |
| Splenic Flexure | 1 | 1.75 |
| 5 Hepatic Flexure | 0 | 0 |
| Anal Canal | 1 | 1.75 |
| Appendix | 0 | 0 |
| Total | 57 |
Ponz De Leon in 2004 studied 626 colorectal cancers out of which 51 cases were in caecum and appendix, 85 cases in ascending colon, 84 cases in transverse: colon and flexures, 51 cases seen in descending colon, while 192 cases seen in sigmoid colon, 151 cases were recorded in rectum and junction (Table 4).
Table 4: Comparison of site wise incidence of other study with present study.
| Site | Study Ponz de Leon 1993 -1998 | Present Study July 2010 - July 2012 |
|---|---|---|
| Caecum | 7.02% | 3.50% |
| Appendix | 1.10% | - |
| Ascending colon | 13.14% | 3.50% |
| Hepatic flexure | 1.30% | - |
| Transverse colon | 11.14% | 8.77% |
| Splenic flexure | 1.10% | 1.75% |
| Descending colon | 8.14% | 1.75% |
| Sigmoid colon | 30.67% | 5.26% |
| Rectum | 24.13% | 61.40% |
| Anal canal | 1.19% | 3.50% |
| Total cases Observed | 626 | 57 |
In our study total numbers of biopsies were 57 out of which 35 cases were in rectum, 6 cases in rectosigmoid, 3 cases were in sigmoid colon, 5 cases in transverse colon, 2 cases in ascending colon, same for caecum and descending colon, 1 case in splenic flexures, and 1 case recorded in anal canal region. High rates of colorectal cancers in young Indians could suggest a different etiopathogenesis, which was neither inherited nor traditional diet related, Epidemiology of digestive tract cancer in India.
Table 5 shows the Age wise incidence in the study period. Table 6 shows in all the anatomical sites, tumors more often occurred in the males was 33 than in females was 24 and ratio M: F, 1.5:1.
Table 5: Age wise incidence in the study period.
| Age | 1-10 | 11-20 | 21-30 | 31-40 | 41-50 | 51-60 | 61-70 | 71-80 | 81-90 |
|---|---|---|---|---|---|---|---|---|---|
| Total | - | - | 3 | 2 | 12 | 28 | 9 | 2 | 1 |
Table 6: Sex wise incidence in the various sites each year.
| Sex | Rectum | Recto Sigmoid Junction | Sigmoid colon | Transverse Colon | Ascending Colon | Descending Colon | Caecum | Anal canal |
|---|---|---|---|---|---|---|---|---|
| Male | 23 | 1 | 2 | 3 | 1 | 1 | 1 | 1 |
| Female | 13 | 5 | 1 | 2 | 1 | - | 1 | 1 |
In mild dysplasia there is little glandular irregularity apart from an increase in branching of glands, nuclei are enlarged, the nuclear cytoplasmic ratio is slightly increased, there may be some early stratification, but the gland arrangement remains regular, in severe dysplasia there is marked glandular irregularity with compression of gland elements which obliterates gland lumina and gives a back-to-back appearance. The nuclear cytoplasmic ratio is greatly increased, there is much cellular pleomorphism with loss of normal nuclear polarity and an increased number or mitosis, mucin secretion is greatly decreased. Moderate dysplasia falls between these two categories. The criteria used for the histologic diagnosis of adenoma, dysplasia, carcinoma in situ (CIS) and invasive carcinoma are those of Enterlie.
Adenomas are defined by the presence of hyperchromatic, crowded, cigar shaped nuclei, are more pleomorphic and less polarized than usual, but the crypt architecture is not markedly distorted. Carcinoma in situ shows the features described in dysplasia plus obvious distortion of growth pattern (irregular budding of glands and cribriform areas). Invasive carcinoma is defined as an adenoma with an area showing not only the cytologic features of carcinoma in situ, but also clear evidence of invasion as denoted by a desmoplastic reaction and or by the presence of single cells or clusters of cells not obviously confined within a tubule or villous structure (Figure 1 to Figure 3).
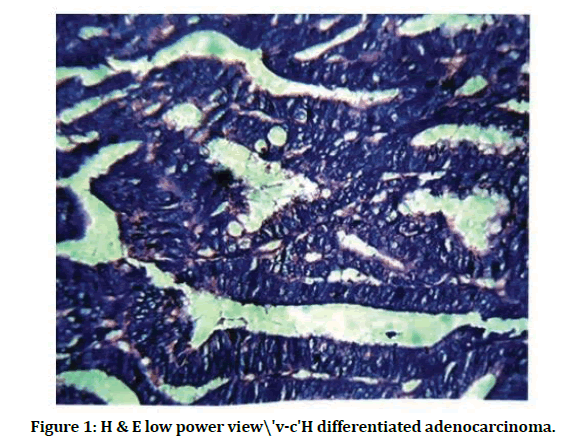
Figure 1: H & E low power view\'v-c'H differentiated adenocarcinoma.
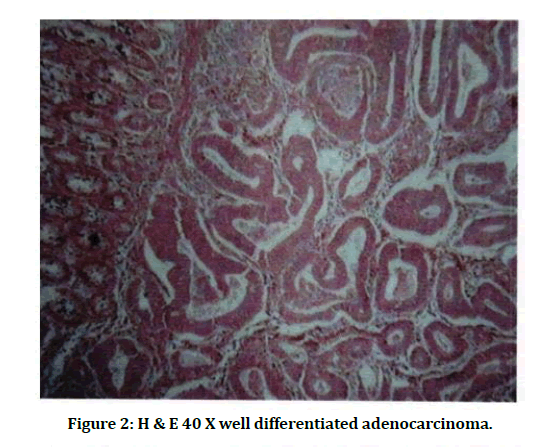
Figure 2: H & E 40 X well differentiated adenocarcinoma.
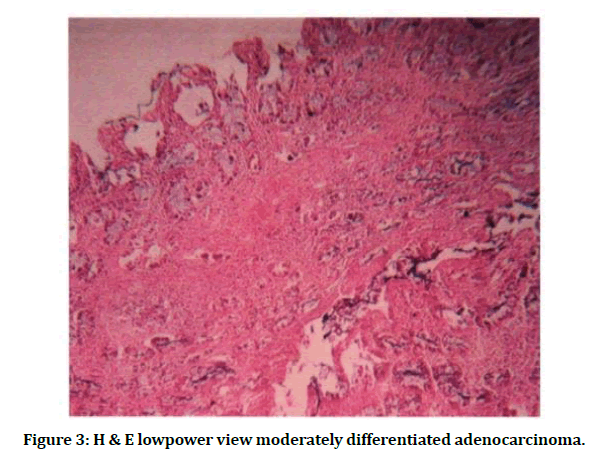
Figure 3: H & E lowpower view moderately differentiated adenocarcinoma.
Discussion
Colorectal cancer is a disease originating from the epithelial cells lining the gastrointestinal tract. The present study was conducted at Sree Bharath Medical College & Hospital, Chrompet, Chennai for a period of 2 years from July 2010 to June 2012. We have studied a total of 57 cases of colorectal carcinoma. Out of 57 malignant lesions, 49 were adenocarcinomas, 1 case of Adenosquamous carcinoma, 7 cases were polyps. Tfilfe was a marked preponderance in adenocarcinoma and the peak incidence was seen in the 5th and 6th decade. Male preponderance was seen with male to female ratio 1.5:1. Out of the 49 cases of adenocarcinomas 19 cases were of well differentiated type (38.72%), 25 cases of moderately differentiated type (51.02%) and 1 cases of poorly differentiated type (1.75%) [14,15].
Mucinous adenocarcinoma is defined by more than or equal to 50% mucin in the section studied. Incidence of mucin secreting adenocarcinoma in our study is (8.33%), it is near to the other studies which has studied 248 cases of adenocarcinomas of which 29 cases were of mucmous carcinomas (11.69%). In our study, the number of cases were recorded in the rectum were 61.40% (35cases). The Rectum is the common site of involvement of malignancies forming 61.40% (35 cases) of the large gut malignancies. This incidence is in accordance with the view that in India carcinoma of rectum and anal canal is seen more frequently than the carcinoma of the colon as in the west. The factors responsible for the high incidence of rectal malignancies are difficult to explain. It may be due to the low fiber. In the present study single tumor was seen in splenic flexure area. Similarly, the series recorded by Ponzdeleon recorded 1.3% incidence from this region [2,16].
In the present study youngest patient seen was female 26 years with adenocarcinoma of the ileocecal region and the oldest patient was 89-year-old male with the adenocarcinoma of the sigmoid colon. Nearly 32.8% (44 cases) of the large gut malignancies occurred between the age of 40-60 years, this study had the same incidence as was done in study series in Shiraz Iran which showed a marked increase in the incidence of colorectal cancer in the 40–60-year-old age group [17]. There was male preponderance in the malignant tumors in our study. In the series presented by PonzdeLeon also showed male preponderance. In the present series the cancer of the colon showed male preponderance. Others have done a retrospective study of 162 cases of colorectal adenocarcinoma histologic variants. It was found that cribriform pattern associated with infiltrative margin, mucinous subtype correlated with depth of invasion, signet ring cell pattern related to its vascular invasion along with nodal and distant metastasis. These factors namely - infiltrative margin, depth of invasion, vascular invasion is associated with poor outcome. In the, resent study one case of signet ring cell variant was associated with recurrence (which itself is an independent factor for aggressive behavior). This patient also had multiple peritoneal metastasis indicating that this morphological subtype is associated with increased incidence of angiolymphatic invasion [18].
Our study shows male were 33 cases, female were 24 cases of colorectal cancer. 37 cases were in 6th decade 32 cases showed lymph node metastasis, 7 cases were in stage I, 9 cases were in stage II, 32 cases were in stage III and 2 cases were in stage IV. The factors responsible for the high incidence of rectal malignancies are difficult to explain. It might be due to the result of repeated mucosal trauma caused by straining during defecation or may be due to increased intake of spicy food.
Conclusion
The present study was conducted at Sree Bharath Medical College & Hospital, Chennai for a period of 2 years starting from July 2010 to June 2012. Age and Sex incidence of all the colorectal carcinoma were analyzed. There was a male predominance in our study and the peak age was in the 5th decade. The age of the youngest patient was 26 years. Bleeding per rectum was the commonest complaint of patients. 44 cases of colorectal carcinoma were seen between age of 40-60 years. Maximum number of cases seen was conventional type of adenocarcinoma. Maximum number of cases was seen in the rectum where it is symptomatic at early stage. Present study shows rectal cancers are more common, which is like the Indian studies whereas colon cancers are more common in World literature. Most of the tumors were ulcer proliferative growth size ranging from 5-20 ems. Mucinous tumors were 4 in number 8.33%, one case was presented with recurrence were associated with poor prognosis. Only 7 cases of polyps associated with adenocarcinoma were seen in our study as compared to the incidence in the West where polyps are most associated with adenocarcinoma. Present study showed one case 1.75% of signet ring cell carcinoma with recurrence, showed poor prognosis.
References
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010; 127:2893-2917.
- Corado MP, Edwards B. Shin HR et al. Cancer incidence in five continents. IARC Scientific publication Volume 9, IARC, Lyon 2007.
- American Cancer Society: Cancer facts and figures. 2006.
- Tamura K, Ishiguro S, Munakata S et al. Annual changes in colorectal carcinoma incidence in Japan. Cancer 1996; 78:1187-1194.
- Kim YI. Vegetables, fruits and CuA>rectal cancer risk: What should we believe? Nutr Rev 2001; 59:394-398.
- Parkin DM. Global cancer statics in the year 2000: Lancet Oncol 2001; 2:533-543.
- Boyle P, Langman JS. ABC of colorectal cancer epidemiology. Br Med J 2000; 321:805-808.
- Hipp JD, Hipp JA, Lyday BW, et al. Cancer vaccines: An update. In vivo. 2000; 14:571-586.
- https://www.who.int/health-topics/cancer
- Moorehead J, Mackelvery STD. Cholecystectomy and colorectal cancer review. Br J Surg 1989; 76:250-253.
- Bremner CG, Ackerman LV. Polyps and carcinoma of the large bowel in the South African Bantu. Cancer 1970; 26:991-999.
- Hills. MJ, Drasar BS, Aries V, et al. Bacteria and etiology of cancer in the large bowel. Lancet 1971; 1:95.
- Muto T, Bussey HJ, Morson BC. The evolution of cancer of the colon and rectum. Cancer 1975; 36:2251-2270.
- Lynch HT, Krush AJ. Differential diagnosis of the cancer family syndrome. Surgery 1973; 6:221-224.
- Thornton JR. High colonic pH promotes colorectal cancer: Hypothesis. Lancet 1981; I:1081-1082.
- Cruse P, Clark C, Lewin M. Dietary cholesterol is co-carcinogenic for human colon cancer. Lancet. 1979; 313:752-755.
- Yeole BB. Trends in cancer incidence in esophagus, stomach, colon, rectum & liver in males in India. Asian Pac J Cancer Prev 2008; 9:97-100.
- Cunningham D, Atkin W, Lenz HJ, et al. Colorectal cancer. Lancet 2010; 375:1030-1047.
