Research - (2021) Volume 9, Issue 5
A Study of Fasting Serum Magnesium Level in Type 2 Diabetes Mellitus and Its Correlation with its Complications
R Umashankar, C Ramakrishnan and Radhakrishanan A*
*Correspondence: Radhakrishanan A, Department of General Medicine, Sree Balaji Medical College and Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email:
Abstract
In our study done in hundred patients admitted in general medical ward in Sree Balaji Medical College Hospital following conclusions were obtained. Summarizing our study: 42 patients had hypomagnesemia ( 42 % ) Youngest patient in our study was 45 years of age; mean age of patients in our study was 57.73 years Hypomagnesemic patients had a higher incidence of complications like neuropathy, retinopathy, and nephropathy. Hypomagnesemia correlated with higher incidence of ischemic heart disease and hypertensive heart disease.
Keywords
Hypertension, Type -2 Diabetes mellitus, Echocardiography, Fasting serum magnesium
Introduction
Diabetes mellitus, the metabolic disease characterized by hyperglycemia due to insulin deficiency or dysfunction or both. The chronic hyperglycemia of diabetes is associated with long term compliations – micro and macro vascular – retinopathy, nephropathy, neuropathy, cerebrovascular disease and peripheral vascular disease. Majority of cases of diabetes fall into two broad categories, Type 1 and Type 2 Diabetes mellitus. Type 2 Diabetes accounts for approximately 90 to 95 percentage of all diagnosed cases of diabetes. Long term complications of diabetes are include retinopathy, nephropathy and peripheral neuropathy and foot ulcers. Patients with diabetes have an increased risk of atherosclerotic, cardiovascular diseases. Hypertension and abnormalities of lipid metabolism are often found in diabetes [1- 3].
There are several pathogenic processes involved in the development of either form of diabetes or long term complications. The basis of the abnormalities in carbohydrate, fat, protein metabolism in diabetes is deficient action of insulin on target tissues. Defective insulin action results from inadequate insulin secretion and or reduced tissue response to insulin action. Defect in insulin secretion or action on target organ frequently coexist in the same patient. Several vitamins and minerals act as cofactors in the enzyme reaction regulated by insulin. Deficiency of several vitamins and minerals such as vitamin E, potassium, magnesium, zinc and chromium may worse the carbohydrate intolerance. Of these the need for potassium or magnesium replacement is relatively easy to detect based on low serum levels [4,5].
Magnesium is the fourth most abundant cation in the human body and the second most abundant intracellular cation. Magnesium plays an essential role in carbohydrate metabolism and in insulin action. Magnesium acts as a cofactor in glucose transport mechanism of the cell membranes and various intra cellular enzymes involved in carbohydrate metabolism. The concentrations of serum magnesium in healthy people are remarkably constant whereas 30 to 35% of diabetes have low serum magnesium concentration. Magnesium deficiency has a negative impact on glucose homeostasis and insulin sensitivity in patients with type 2 diabetes as well as the evaluation of the complications like retinopathy, cardiovascular diseases, nephropathy and neuropathy. Moreover, low serum magnesium is a strong, independent predictor of development of type 2 diabetes. The present study was undertaken with an aim to estimate prevalence of hypomagnesemia in patients with type 2 diabetes and correlate serum magnesiumconcentrations with micro and macro vascular complications of diabetes [6-9].
Methodology
Study population
Patients with type 2 diabetes mellitus admitted in general medical ward in Sree Balaji medical college hospital.
Methods
100 patients with type 2 DM who were admitted in general medical ward in Sree Balaji Medical College Hospital were randomly selected for this study. From all patients detailed history, thorough clinical examination and relevant biochemical investigations were obtained.
Inclusion criteria
All case of type 2 DM admitted in Sree Balaji medical hospital in general medical wards.
Exclusion criteria
Chronic Diarrhea, Malabsorption, Patients with Renal Failure, Patients on Diuretics, Acute Myocardial Infarction in Last 6 Months, Patient Having Alcohol Abuse, Patients Receiving Mg Supplements or Mg containing Antacid.
Patients were divided into three groups as follows normal 1.7-2.4mg/dl, low <1.7mg/dl, high >2.4mg/dl. Patients were categorized on the basis of diabetic duration, presence of IHD, HTN, mode of treatment, presence/absence of retinopathy, neuropathy, nephropathy and glycemic control. Diabetic retinopathy was classified as non-proliferative diabetic retinopathy and proliferative retinopathy. Diabetic nephropathy was graded by using 24 hr urine albumin as follows no nephropathy if <30mg/24hr, microalbuminuria 30 -299mg/24hr and macroalbuminuria >=300mg/24hr.
Statistical method
Statistical method analysis was done using chi square test and sample variable t test to compare proportions. Results were considered significant at p value <0.05.
Results
This study was composed of 100 patients of type 2 DM of which 54 were men and 46 were women. These patients were further grouped according to their age, duration of diabetes, mode of treatment, glycemic control, presence, or absence of co morbidities (ischemic heart disease and hypertension) and presence / absence of diabetic complications (retinopathy, neuropathy and nephropathy).
In our study maximum number of diabetics occurred in the age group 51 – 70 years. Youngest patient in our study was of the age 45 years. The mean age of diabetic patient in our study was 57.73 years. In our study maximum number of hypomagnesemia patients occurred in the age group 61 – 70 years (45.24 %). All patients who were more than 70 years old had hypomagnesemia (100 %) (Table 1 and Table 2 and Figure 1).
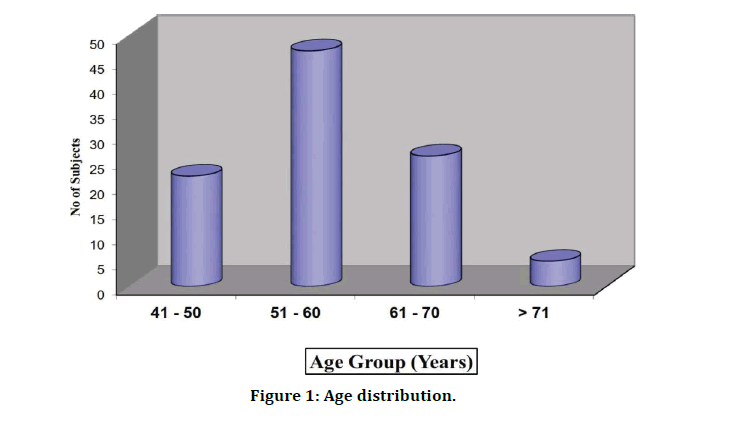
Figure 1: Age distribution.
Table 1: Age distribution & magnesium levels.
| Age Group | No of Patients | % |
|---|---|---|
| 41-50 | 22 | 22 |
| 51-60 | 47 | 47 |
| 61-70 | 26 | 26 |
| >70 | 5 | 5 |
| Total | 100 | 100 |
| Mean | 57.73 | |
| Sd | 7.9 | |
Table 2: Magnesium levels.
| Age Group (Yrs.) | Hypomagnesemia | Normomagnesemia | Total | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| 41–50 | 2 | 4.76 | 20 | 34.48 | 22 | 22 |
| 51–60 | 16 | 38.1 | 31 | 53.45 | 47 | 47 |
| 61-70 | 19 | 45.24 | 7 | 12.07 | 26 | 26 |
| ≥ 71 | 5 | 11.9 | 0 | 0 | 5 | 5 |
| Total | 42 | 100 | 58 | 100 | 100 | 100 |
The average duration of diabetes in our study population was 9.39 years and range from 2 yrs. to 25 yrs.; among the 100 patients 44 persons were receiving insulin and 56 persons were receiving OHAs; Among these individuals 10 patients had hypertension (10%) and 34 patients had ischemic heart diseases (34%) total 28 patients had retinopathy (28%) and out of them 22 had nonproliferative retinopathy and 6 had proliferative retinopathy. Total 14 patients had diabetic nephropathy (14%) among them 5 patients were microalbuminuria, and 9 patients were macroalbuminuria and 4 persons had neuropathy (4%) (Table 3).
Table 3: Characteristics of study population.
| Sl. No. | Characteristics | Value |
|---|---|---|
| 1 | No of Subject | 100 |
| Men | 54 | |
| Women | 46 | |
| 2 | Age in Years | 57.73 ± 7.90 (45 – 82 ) |
| Men | 55.69 ± 6.82 | |
| Women | 60.13 ± 8.46 | |
| Medication | ||
| 3 | Insulin | 44 |
| OHA | 56 | |
| Co morbidities | ||
| 4 | Hypertension | 10 |
| Ischemic Heart Disease | 34 | |
| 5 | Diabetic Retinopathy | 28 |
| NPDR PDR | 6 | |
| 6 | Diabetic Neuropathy | 4 |
| 7 | Diabetic Nephropathy | 14 |
| Microalbuminuria | 5 | |
| Macroalbuminuria | 9 | |
In our study among the 100 patients, hypomagnesemia (serum Mg <1.7 mg/dl) was found in 42 patients of type 2 diabetic patients.58 patients had normal serum magnesium level. No patient had hypermagnesemia. No significant difference was found in the rate of hypomagnesemia in men and women (42.86% and 57.14% respectively). There was no significant statistical difference found between men and women p value=0.057 (Table 4 and Figure 2).
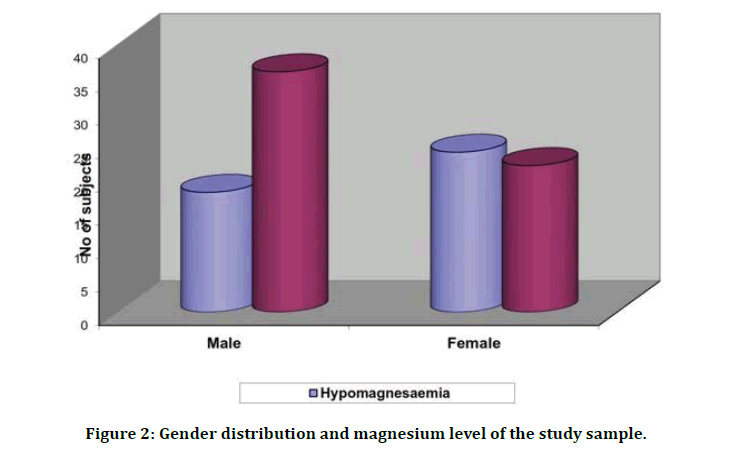
Figure 2: Gender distribution and magnesium level of the study sample.
Table 4: Sex distribution and magnesium levels.
| Hypomagnesemia | Normomagnesemia | Total | ||||
|---|---|---|---|---|---|---|
| Sex | No of patient | Percentage % | No of Patient | Percentage % | No of Patients | Percentage % |
| Male | 18 | 42.86 | 36 | 62.07 | 54 | 54 |
| Female | 24 | 57.14 | 22 | 37.93 | 46 | 46 |
| Total | 42 | 100 | 58 | 100 | 100 | 100 |
| Chi-square | 3.62 | |||||
| Df | 1 | |||||
| Significant | 0.057 Not Significant | |||||
In our study among the 100 diabetic patients 56 patients took OHA whereas 44 patients took insulin therapy. Among the OHA receiving individuals 49 patients had normal magnesium level and only 7 patients had low serum magnesium level (84.48% versus 16.67%). Among the patients receiving insulin therapy 35 patients had low serum magnesium level, whereas 9 patients had normal serum magnesium level. This difference was statistically significant as shown by p value=0.0001 (Figure 3).
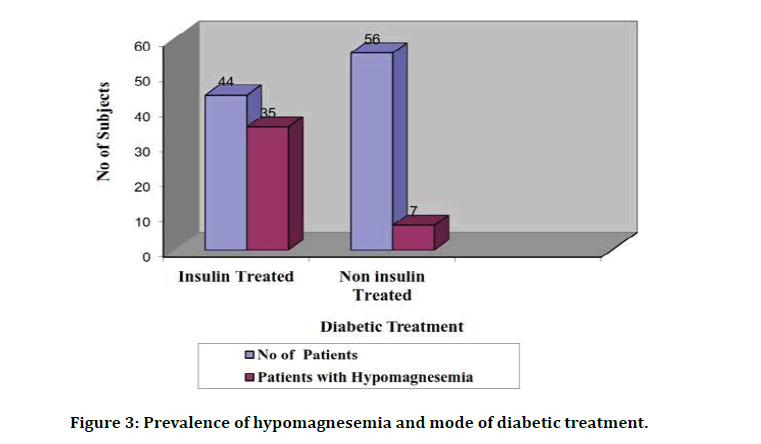
Figure 3: Prevalence of hypomagnesemia and mode of diabetic treatment.
In our study, 22 patient had poor glycemic control as evidenced by FBS >130mg/dl (81.82%). While on treatment, the mean blood sugar level in patient with hypomagnesemia was 128.83 whereas the mean blood sugar level in patients with normomagnesemia was 112.40. Thus the association between the poor glycemic control and hypomagnesemia was statistically significant as shown by the p value of 0.0001 (Figure 4).
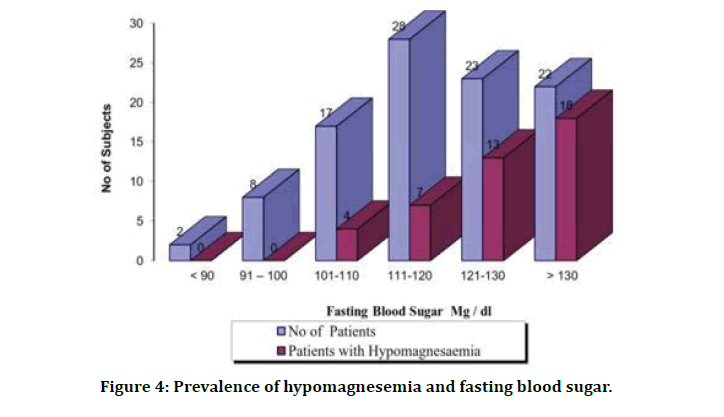
Figure 4: Prevalence of hypomagnesemia and fasting blood sugar.
Prevalence of hypomagnesemia in diabetic patients with complications was significantly higher when compared to diabetic patients with no complications (67.92% versus 17.02%). The difference was statistically significant with p value less than 0.05 (Table 5).
Discussion
Many studies have proven beyond doubt the association between the presence of hypomagnesemia and diabetes mellitus; it has also been proven that hypomagnesemia has been associated with increased incidence of complications in diabetics 7; hence I found it worthy to take up this study in our settings. Previous studies by Nadler JC and Rude RK have reported low serum magnesium status in patients with type 2 DM. The reported prevalence of hypomagnesemia ranged from 13.5% to 47.7% in type 2 DM patients according to Pham PC, Pham PM, Miller JM et al. In our study there were a total of 100 diabetic patients; among them 42 patients had serum Mg below the reference range; Prevalence of hypomagnesemia in type 2 diabetes melli tus according to our study was similar to that reported by Nadler et al. Walti mk et al reported that prevalence of hypomagnesemia in type 2 diabetes at 37.6% versus 10.9% in non diabeteic controls in a study conducted in, Switzerland; this too is in concordance with our study results [10].
The causes for the high prevalence of hypomagnesemia in diabetes may be due to increased urinary loss, low dietary intake or impaired magnesium absorption compared to healthy individuals; Rude RK, Mc Nair P, Christiansen MS et al in their study found excessive urinary magnesium loss in diabetes. Recently defective tubular reabsorption in thick ascending loop of henle is postulated, that results in hypomagnesemia [11]. The reason for the tubular defect is unclear. In diabetes low serum magnesium status due to low dietary intake is unlikely. Only 5.4% of the diabetic groups and 9.1% of the control group in European dietary assessment studies by Walti MK Zimmermann et al had intake of magnesium below their individual requirements. In addition, type 2diabetes patients with reasonable metabolic control absorb dietary magnesium to a similar extent as healthy controls. In diabetes hyperglycemia and osmotic diuresis may cause excessive urinary loss of magnesium and leads to low serum magnesium status [12].
In our study maximum number of diabetics occurred in the age group 51–70 yrs. (35 patients) youngest patient in our study was of the age 45 years; mean age of diabetic patients in our study was 57 .73 hypomagnesemia occurred maximally in the age group 61–70yrs (45%) ; all patients who were > 70 years old were hypomagnesemic (100%); mean age of hypomagnesemia in our study was 63.14 years; As the age increased the prevalence of hypomagnesemia increased in diabetics; p value was 0.0001; according to other studies proved a significant correlation between age and magnesium levels; the former also proved a correlation between the male sex and magnesium levels; our study concurred with the above studies with regards to age but not with sex preponderance and magnesium levels In our study 54 patients were males and 46 were females; 24 among the females had hypomagnesemia (52.17%); 18 of the males had hypomagnesemia (33%); the association between gender and hypomagnesemia was not significant as seen by the p value 0.057 [13-15].
In our study 22 patients had poor control of blood sugar as evidenced by FBS of > 130 mg /dl; Among them 18 had hypomagnesemia (81.8%); 51 patients had FBS in the range 101– 30 mg /dl; among them 20 had hypomagnesemia (40 %. With statistical analysis it is seen that those with poor blood sugar control had higher prevalence of hypomagnesemia as evidenced by the p value of 0.0001 which is significant [16,17]. In the end after comparing all the variables and complications between the normomagnesemic and hypomagnesemic groups, it has been found that complication rate was more in the hypomagnesemia group (67 %) than the normomagnesemic group (40%). The three prominent complications analyzed in the study are retinopathy, nephropathy, and neuropathy; the p value that we got was <0.005 emphasizing the significance of the association; Sharma et al also found that hypomagnesemic diabetic patients had more complications than normomagnesemic diabetic patients.
Conclusion
Low serum magnesium levels are commonly seen in diabetic patients. Hypomagnesemia is more common in diabetic patients with poor glycemic control. Hypomagnesemia in diabetic patients correlates well with duration of illness, glycemic control, and complications of diabetes mellitus-both macro vascular and micro vascular.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
The encouragement and support from Bharath Institute of Higher Education and Research, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- American Diabetes Association–Clinical Practice Recommendations Diabetes care; 2011.
- Powers AC. Harrison’s principles of internal medicine: Diabetes mellitus. 18 thEd. New Delhi: McGraw Hill Medical Publishing Division; 2011.
- Pham PC, Pham PM, Pham SV, et al. Hypomagnesemia in patients with type 2 diabetes. Clin J Am Soc Nephrol 2007; 2:366-373.
- Tosiello L. Hypomagnesemia and diabetes mellitus. A review of clinical implications. Arch Intern Med 1996; 156:1143-1148.
- De valk HW. Magnesium in diabetes mellitus. Neth J Med 1999; 54:139-146.
- Sharma A, Dabla S, Agrawal RP, et al. Serum magnesium: An early predictor of course and complications of diabetes mellitus. J Indian Med Assoc 2007; 105:16-20.
- Sales CH, Pedrosa Lde F. Magnesium and diabetes mellitus: their relation. Clin Nutr 2006; 25:554-562.
- Hatwal A, Gujral AS, Bhatia RP, et al. Association of hypomagnesemia with diabetic retinopathy. Acta Ophthalmol (Copenh). 1989; 67: 714-716.
- Ceriello A, Giugliano D, Dello Russo P, et al. Hypomagnesemia in relation to diabetic retinopathy. Diabetes Care 1982; 5:558.
- McNair P, Christiansen C, Madsbad S, et al. Hypomagnesemia, a risk factor in diabetic retinopathy. Diabetes 1978; 27:1075-1077.
- Liao F, Folsom AR, Brancati FL. Is low magnesium concentration a risk factor for coronary heart disease? The Atherosclerosis riskin communities (ARIC) study. Am Heart J 1998; 136:480-490.
- Reffelmann T, Ittermann T, Dörr M, et al. Low serum magnesium concentrations predict cardiovascular and all-cause mortality. Atherosclerosis 2011; 219:280-284.
- Gupta VK. Does hypomagnesemia have an adaptive role in hypertension? Hypertension 2004; 43.
- Guerrero-Romero F, Rodríguez-Morán M. Low serum magnesium levels and metabolic syndrome. Acta Diabetol 2002; 39:209.
- Cholst IN, Steinberg SF, Tropper PJ, et al. The influence of hypermagnesemia on serum calcium and parathyroid hormone levels in human subjects. N Engl J Med 1984; 310:1221.
- Ma J, Folsom AR, Melnick SL, et al. Associations of serum and dietary magnesium with cardiovascular disease, hypertension, diabetes, insulin and carotid arterial wall thickness. The atherosclerosis risk in communities (ARIC) study. J Clin Epidemiol 1 995; 48:927-940.
- Garber AJ. Magnesium utilization survey in selected patients with diabetes. Clin The 1996; 18:285–294.
Author Info
R Umashankar, C Ramakrishnan and Radhakrishanan A*
Department of General Medicine, Sree Balaji Medical College and Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: R Umashankar, C Ramakrishnan, Radhakrishanan A, A Study of Fasting Serum Magnesium Level in Type 2 Diabetes Mellitus and Its Correlation with its Complications, J Res Med Dent Sci, 2021, 9 (5):220-226.
Received: 25-Mar-2021 Accepted: 21-May-2021 Published: 31-May-2021
