Research - (2022) Volume 10, Issue 1
A Study of Short-Term Outcomes in Neonates Referred to the Tertiary Care Hospital in Central India
R Abhilasha Singh Panwar1*, Sachin Damke1, Keerti Swarnkar1, Amar Taksande1, Revat Meshram1, Sham Lohiya1 and Bhavana Lakhkar2
*Correspondence: R Abhilasha Singh Panwar, Department of Paediatrics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi, Wardha, Maharashtra, India, Email:
Abstract
Background: The neonatal mortality rate reflects the utilization of the health services and the quality of the health services in a country. In developing countries like India neonatal mortality rate is one of the highest in the world. India has a high NMR of 28/1000 live births. Mortality in babies referred to a tertiary care unit has a fair contribution toward the NMR. This study aims to find the factors affecting mortality in neonates referred to a tertiary care neonatal ICU. Material & Methods: In this prospective observational study all neonates referred to our hospital over a period of 2 years from July 2018- June 2020 were enrolled after informed voluntary consent. Detailed history and transport characteristics were noted in a Performa. The clinical course and treatment with short term outcomes i.e. death or discharge was noted Results: Out of 300 neonates 51% were transported by ambulance and 49% were transported by private vehicle. Among the clinical and biochemical variable (TOPS score) there was a significant mortality associated with hypothermia, prolonged CRT and SpO2 <90% and cyanosis on admission. The most common cause of mortality was sepsis followed by hypoxic ischemic encephalopathy and respiratory distress syndrome. Statistically significant death was found in low-birth-weight babies, home delivered, those transported by a private vehicle, with whom referral note was not available and referral reasons, airway advice and treatment during transport were not given. Conclusion: Transporting a sick neonate is very stressful event for the neonate and more so if his physiological parameters are not maintained, possess a great risk for mortality. Strengthening of this link is required to improve survival in neonates requiring transport.
Keywords
Neonatal mortality, Transport, Sepsis, TOPS score
Introduction
India has a high neonatal mortality rate among the many countries in the world. Most of the deaths occur during early neonatal period [1]. Approximately during the first month of life, 4 million deaths are recorded [2]. India accounts for 20% of the world births which is approximately 27 million live births/ year with about 2 million under –five annual deaths [3]. The sick neonates are referred from subcentre and primary health centre to higher health facilities like secondary and tertiary care centres [4]. The causes of referral include prematurity, birth asphyxia, neonatal jaundice, septicemia, convulsions, congenital malformations, and management for surgical diseases like trachea oesophageal fistula, imperforate anus, congenital heart diseases, diaphragmatic hernia, intestinal obstruction, congenital hypertrophic pyloric stenosis and other surgical conditions [5,6]. According to the WHO, neonatal deaths most commonly are due to prematurity-27%, neonatal septicemia which includes neonatal pneumonia and neonatal meningitis-23%, birth asphyxia 6%, congenital anomalies 4%, tetanus 3% and other causes constitutes around 7% [7].
The neonatal and infant mortality rates are indicators of human developmental index. The utilization of economic funds for the health services and implementation of health services for the benefit of masses should be carried out in phasic and appropriate manner. In a developing country like India the maternal and child health care is getting more attention as indicated by the improvement of health indices, but regionalization of maternal and perinatal care is still deficient [4].
Many sick new-borns can be transported in timely and effective manner if the transport facilities are available. The neonates are inherently immuno incompetent thereby making them prone to infections. Moreover, the cardiorespiratory reserve is less if added by poor transport services and inadequate health infrastructure which may lead to further compromise of the neonatal health. There are many issues related to transport of sick infants like availability of ambulance equipped with oxygen and medications, accompanying personnel, pretreatment before the referral, adequate positioning and feeding of neonates during transport and transport time [5]. We undertook this study to study the various factors associated with the mortality in babies referred to a tertiary care neonatal ICU including transport factors.
Methodology
The objective of this study was to assess the factors affecting outcome of transported neonates and to assess the causes of mortality in neonates. This was a prospective observational study undertaken in 300 neonates for a duration of two years between 2018-2020 in the neonatology unit of Paediatrics department of AVBRH, Sawangi Wardha. Neonates delivered outside and admitted at AVBRH NICU were taken into the study. Neonates whose parents were not willing were excluded from the study.
The approval of the Institutional Ethical Committee of the university of Datta Meghe Institute of Medical Science was taken before commencing the study. IEC no: DMIMS (DU)/IEC/2018-19/7476.
A Detailed information sheet was given to the parents of all neonates who fulfilled the inclusion criteria, in which the methodology of the study was explained in their local language. The parents of the neonates who were not willing to participate in the study were not included in the study.
Patient’s demographic details- Name, Age at admission, Sex and the place of referral were noted. Presenting complaint’s and on admission baby’s temperature, oxygen saturation, capillary refill time and RBS was noted. The transport history was elicited- if baby had come in an ambulance/private vehicle accompanied by medical personnel during transport. Whether the patient had a referral note with referral reason and advice regarding airway, feeding and temperature advice whether given and duration of transport was noted. Maternal antenatal and obstetric history and baby’s natal and postnatal history was taken. Baby was then examined and NICU stay and treatment received was closely followed up. The babies were managed as per the existing NICU protocol of the institute. During their course of stay we had noted what medications they had received, abnormal investigations and if the patient got discharged or had died. The cause of death was noted down. All the observations were noted down and added to Microsoft excel sheet. Descriptive and inferential statistical analysis was done using Stata software (Stata 10, Stata corporation Texas, USA). Quantitative data was analysed using mean, median and standard deviation. Qualitative data was summarized using percentage and differences in proportion were compared by chi square test. Differences between means were compared by unpaired student’s ‘t’ test. Data was analysed about the various factors affecting the neonatal mortality and the cause of death was analysed.
Definitions[8]
• LBW: Birth weight less than 2.5 Kg irrespective of gestational age.
• Preterm: Baby born before 37 completed weeks of Gestation from history and examination.
• Term: Gestational age between 37-42 completed weeks.
• Post term: Gestational age more than 42 weeks.
• Small for gestational age (SGA): Weight less than 10th percentile for gestation.
• Large for gestational age (LGA): Weight more than 90th percentile for gestation.
• Appropriate for gestational age (AGA): Weight between 10th and 90th percentile for gestation.
• Hypothermia: Axillary temperature was taken by digital thermometer and Observed temperature was graded as per standard guidelines of WHO.
• Cyanosis: Presence of dusky soles with perioral cyanosis.
• Hypoglycaemia: Hypoglycaemia was taken as blood glucose less than 40 mg/dl with reagent strips.
• Delayed capillary filling time (CFT): Was taken as more than two seconds.
• Respiratory distress: Defined as respiratory rate more than 60/minute in a quite baby associated with lower chest wall indrawing with or without nasal flaring and/ or expiratory grunting.
Results
Out of 199 males–165 (83.33%) survived and 33 (37.87%) expired. Out of 102 females–91 (89.22%) survived and 11 (10.78%) expired. Male: Female ratio is 2:1. Statistically significant death was found in low-birthweight babies with a significant mean weight of babies in the expired group was lesser (2 + 0.73) than the survived group (2.35 + 0.53). The gestational age of the survived neonates was 35.8 + 4.42 and in expired neonates 34 + 5.51 which was statistically significant (p value: 0.007). Referred preterm babies had higher percentage of deaths than the term babies, though there was no statistical significance. No statistically significant mortality was found between the SGA and AGA babies. Among home deliveries 4 (57.14%) survived and 3 (42.86%) expired. Statistically significant death was found in neonates delivered at home. Among ambulance neonates 141 (92.16%) survived and 12 (7.84%) expired. Among neonates transported in a private vehicle 115 (78.23%) survived and 32 (21.77%) expired. Statistically significant amount of death was noted in neonates transported by a private vehicle (Table 1).
| Characteristics | Survived n (%) | Expired n (%) | p value |
|---|---|---|---|
| Gender | |||
| Male | 165(83.33) | 33(37.87) | 0.172 |
| Female | 91(89.22) | 11(10.78) | |
| Weight | |||
| <2.5kg | 146(82.02) | 32(17.97) | 0.05 |
| >2.5kg | 110(90.16) | 12(9.84) | |
| Gestational age | |||
| <37 weeks | 61(20.33) | 13(17.57) | 0.416 |
| >37 weeks | 195(86.28) | 31(13.72) | |
| Weight for gestational age | |||
| SGA | 48(85.71) | 8(14.29) | 0.929 |
| AGA | 208(85.25) | 36(14.75) | |
| Place of delivery | |||
| Institution | 252(86) | 41(14) | 0.033 |
| Home | 4(57.14) | 3(42.86) | |
| Mode of transport | |||
| Ambulance | 141(92.16) | 12(7.84) | 0.001 |
| Private vehicle | 115(78.23) | 32(21.77) | |
Table 1: Demographic characteristics.
No statistically significant difference was found between the survived and expired neonates according to the transport duration though more percentage of deaths were found in neonates transported for more than 120 minutes. Statistically significant death was found in neonates in whom referral note was not available and referral reasons not specified, in whom airway, feeding, temperature advice was not given and did not receive oxygen and treatment during transport (Table 2).
| Characteristics | Survived n (%) | Expired n (%) | p value |
|---|---|---|---|
| Mode of transport | |||
| Ambulance | 141(92.16) | 12(7.84) | 0.001 |
| Private vehicle | 115(78.23) | 32(21.77) | |
| Transport duration | |||
| <60 min | 87(89.69) | 10(10.31) | 0.257 |
| Â 60-120 min | 39(86.66) | 6(13.33) | |
| >120min | 130(82.28) | 28(17.72) | |
| Referral note available | 155(91.18) | 15(8.82) | 0.001 |
| 101(77.69) | 29(22.31) | ||
| Referral reason specified | 163(91.06) | 16(8.94) | 0.001 |
| 93(76.89) | 28(23.14) | ||
| Airway advice | 74(93.67) | 5(6.34) | 0.015 |
| 182(82.36) | 39(17.65) | ||
| Feeding advice | 75(80.65) | 18(40.91) | 0.124 |
| 181(70.7) | 26(59.09) | ||
| Temperature advice | 75(29.3) | 17(19.35) | 0.215 |
| 181(87.02) | 27(13) | ||
| Oxygen during transport | 61(92.42) | 5(7.58) | 0.065 |
| 195(83.33) | 39(16.66) | ||
| Treatment during transport | 73(93.59) | 5(6.41) | 0.017 |
| 183(82.43) | 39(17.57) | ||
| Health personnel during transport | 43(93.47) | 3(6.52) | 0.09 |
| 213(83.86) | 41(16.14) | ||
Table 2: Transport characteristics.
Statistically significant deaths were seen in neonates who required resuscitation on admission, who were ventilated and those who received inotropes and blood products. Out of 300 neonates- 25 had hypothermia on admission and 275 did not have hypothermia. Among the neonates with hypothermia 13(52%) survived and 12 (48%) expired. In neonates who don’t have hypothermia 243(88.36%) survived and 32(11.63%) expired. Prolonged CRT was present in 66 neonates and absent in 234 neonates. Those with prolonged CRT-46(69.7%) had survived and 20(30.3%) had expired. In neonates whose CRT was normal 210 (89.74%) had survived and24(10.26%) had expired. SpO2 <90% was seen in 129 neonates and absent in 171 neonates. In those with SpO2 <90%, 92 (71.31%) had survived and 37 (28.68%) had expired. Among those with saturation more than 90%-164(95.91%) had survived and 7 (4.1%) had expired. Cyanosis was seen in 22 neonates and was absent in 278 neonates. Among those with cyanosis- 15 (68.18%) survived and 7 (31.81%) expired. In those with no cyanosis – 241 (86.7%) survived and 37 (13.31%) expired (Table 3).
| Characteristics | Survived n (%) | Expired n (%) | p value |
|---|---|---|---|
| Resuscitation on admission | 6(35.3) | 11(64.7) | 0.001 |
| Inotrope | 39(47) | 44(53.02) | 0.001 |
| Ventilation | 38(46.34) | 44(53.66) | 0.001 |
| Blood products | 42(60) | 28(40) | 0.001 |
| Hypothermia | 13(52) | 12(48) | 0.001 |
| Prolonged CRT | 46(69.7) | 20(30.3) | 0.001 |
| SpO2 <90% | 92(71.31) | 37(28.68) | 0.001 |
| Cyanosis | 15(68.18) | 7(31.81) | 0.018 |
| Hypoglycemia | 24(82.76) | 5(17.24) | 0.68 |
Table 3: Course in hospital.
Table 4 shows various morbidities in the referred neonates. The most common morbidities in referred neonates were Sepsis, Respiratory distress syndrome, Hypoxic ischemic encephalopathy, Neonatal hyperbilirubinemia, and congenital heart diseases.
| S. No | Major morbidities | N=300 | % |
|---|---|---|---|
| 1 | Sepsis, DIC | 122 | 40.67% |
| 2 | Respiratory distress syndrome | 53 | 17.67% |
| 3 | Hypoxic ischemic encephalopathy | 31 | 10.33% |
| 4 | Neonatal hyperbilirubinemia | 30 | 10% |
| 5 | Congenital heart disease | 13 | 4.33% |
| 6 | Meconium aspiration syndrome | 12 | 4% |
| 7 | Neonatal seizures | 11 | 3.67% |
| 8 | Prematurity | 11 | 3.67% |
| 9 | Surgical cases | 10 | 3.33% |
| 10 | Transient tachypnoea of newborn | 6 | 2% |
Table 4: Morbidities in referred neonates.
The most common cause of mortality was Sepsis followed by Hypoxic ischemic encephalopathy, Respiratory distress syndrome, Intraventricular haemorrhage, Congestive heart failure and Meconium aspiration syndrome (Table 5and Figure 1).
| Cause of Mortality | n=44 | Percentage |
|---|---|---|
| Sepsis, Sepsis with DIC | 26 | 59.10% |
| Hypoxic ischemic encephalopathy | 5 | 11.36% |
| Respiratory distress syndrome | 4 | 1.33% |
| Intraventricular haemorrhage | 4 | 1.33% |
| Congestive heart failure | 3 | 1% |
| Meconium aspiration syndrome | 2 | 0.67% |
| Total number of deaths = 44 (14.67% of the total admission) | ||
Table 5: Causes of mortality.
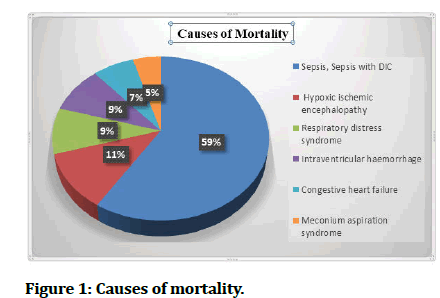
Figure 1: Causes of mortality.
Discussion
Around the globe approximately 4 four million deaths occur in the neonatal period [2]. In India 1 million babies die in the first month of life. Less data is available on the factors associated with mortality in referred new-borns in India which is higher when compared with the mortality in inborn babies. NICU care in our country has developed over the past decade, but India still contributes to major percentage of neonatal deaths in the world. Developed NICU’s are confined to the urban areas only, hence the babies are referred for the want of better care. Government has introduced various programmes to decrease the neonatal mortality, one of which is a level 2 Special Newborn Care units (SNCU). New-borns need to be referred to this SNCU or tertiary care for further management. Many of the neonates referred reach the NICU in unstable condition. So it is important for the referring physician to transport the baby in stable condition and with appropriate transport care. In this study we have assessed the factors associated with neonatal mortality in neonates referred to our NICU.
We had a male: female ratio of 2:1. Trend of male: female ratio in studies by Adikane et al [9], Sachan et al [1], Ghanghoriya et al [6] was 1.4:1, 1.5:1, 2.5:1 respectively.
Male babies had more admission rates than female. It seems like the male babies were brought for treatment more while the treatment of female babies was neglected due to gender bias. Significant mortality rate was found among the males which was like studies by Baidya et al [4] and Bokade et al [10]. In our study 24.67% neonates were preterm which was like Adikane et al [9] -20.28%. Significant mortality was seen in preterm babies which is due to various problems of the preterm babies like Intraventricular haemorrhage, Necrotizing enterocolitis, deficient surfactant production etc. Statistically significant deaths were recorded among low birth weight babies. Ghanghoriya et al. [6] found that 52% of the expired neonates were less than 1.5kg. There was no statistically significant mortality between SGA and AGA babies. Mortality was highest in our study in neonates referred after 14 days of life. Neonates who were referred early had better survival outcome as they had received treatment early.
In our study 2.3% of the deliveries were home deliveries which was like study by Bokade et al. [10]. 38.33% of neonates were born by caesarean section birth in our study which can be due be due to complicated pregnancies leading to caesarean section birth followed by NICU stay. A statistically significant difference in mortality was observed in neonates transported by private vehicle (21.8%) than those transported by ambulance (7.84%). In our study almost half of the neonates were transported by ambulance and rest by private vehicle which was similar to study by Dalal et al [11] where 47.3% of neonates were transported by ambulance. Most of them were a minivan or minibus equipped by an oxygen cylinder, with no warmer or resuscitation materials. Many of these ambulances were brought by medical personnel who were not trained in neonatal resuscitation or only with the ambulance driver alone. More mortality was seen in neonates referred by private vehicle as there was no support to the neonate during transport like warmer, oxygen etc. Neonates requiring more time for transport were at a significant higher risk of mortality. Neonates who were transported for a longer duration had a higher risk for increased mortality as they were prone to infection, hypothermia, hypoglycaemia, circulatory abnormalities during transport.
The various factors studied were the type of transport, duration of transport, referral note given and the referral reason told. We had asked if airway, feeding, and temperature advice were given during transport. If patient received treatment and oxygen during transport and if patient was accompanied by a health personnel during transport. During hospital stay if patient had received resuscitation, inotropes, ventilation, and blood products. If there was hypothermia, prolonged CRT, SpO2 <90%, cyanosis and hypoglycaemia at the time of admission.
Statistically significant mortality was found in transported neonates who did not have a referral note, referral reason not specified, and airway advice and transport treatment were not given. However, more percentage of deaths was found in neonates in whom temperature and feeding advice not given, oxygen not received and not accompanied by a health personnel while transport. Ghanghoriya et al [6] found significant mortality in neonates transported without oxygen support. Baidya et al [4] found that significant mortality in babies transported without any referral note, in whom airway advice was not given showed higher mortality like in our study. Aggarwal et al [12] found in his study that no prior details were given before transportation of the neonates and only 30% of them had a referral note. For a better neonatal transport system, we need more human resources, with vehicles and equipment’s along with good communication and family support. It is always better to have an organized rather than a self-vehicle transport. Care during transport can be given by trained paramedical personnel rather than an ASHA worker or a doctor.
In our study most of the neonates who required resuscitation on admission had significant mortality rate.
TOPS scoring was developed by Mathur et al [13] which is used to assess the acute neonatal physiology of transported neonates the parameters included were temperature, oxygen saturation, skin perfusion and blood glucose level. Statistically significant mortality was found in neonates with hypothermia, prolonged CRT and SpO2 <90% and cyanosis. The mean temperature of the survived (37 ± 0.34) and expired (36.7 ± 0.76) neonates was statistically significant, suggesting hypothermia being significantly present in expired neonates. Advising Kangaroo mother care, using plastic wrap, thermocol boxes in low resource setting is important to maintain the temperature. Neonates with hypoglycaemia did not show any increase in mortality which was like Ghanghoriya et al [6] and Aggarwal et al [12]. There is a decrease in hypoglycaemia, acidosis and mortality in neonates who were stabilized before transport.
66% of the neonates had less than 7 days of NICU stay and 20.67% stayed for 7-14 days and 13.3% stayed for more than 14 days. There was no statistically significant mortality based on the duration of stay, but maximum percentage of death was seen in neonates who stayed less than 7 days. Most neonates had increased chance of death within the first 24hours of life. This can be due to some antenatal and natal complications which leads to higher mortality within the first 24-72 hours.
The most common morbidities in our study were Sepsis, Respiratory distress syndrome, Hypoxic ischemic encephalopathy, Neonatal hyperbilirubinemia and congenital heart disease. The mortality in our study was 14.67% which was like study by Kumar et al [14] and Ghanghoriya et al [6]. Many related studies were reported [15-20]. The most common cause being Sepsis followed by Hypoxic ischemia encephalopathy, Respiratory distress syndrome, Intraventricular haemorrhage, Congestive heart failure and Meconium aspiration syndrome.
Limitations
• The new-borns were not tracked after discharge. Hence follow up of these cases was missed.
• The transport and ambulance characteristics were obtained by asking leading questions in the history. Direct assessment of the ambulance was not performed.
Conclusion
The various factors contributing to the mortality in neonates referred to a tertiary care NICU were studied in this project. A fragile neonate is affected by many factors during transport which have been recognized by many previous studies. We need more better standardized NICU with regionalization of the NICU care. These deaths can be avoided by institutional deliveries, improvement of neonatal transport facilities, better NICU care and maintaining asepsis in the NICU. Primary management by the primary care physician is necessary to curb the death rate of the neonates in a tertiary care hospital. India has still not achieved the millennium developmental goals. New five-year plan must include–improvement of neonatal transport facilities, strict maternal health care and training of primary physicians in neonatal resuscitation.
References
- Sachan R, Singh A, Kumar D, et al. Predictors of neonatal mortality referred to a tertiary care teaching institute: a descriptive study. Indian J Child Health 2016; 3:154-8.
- Lawn JE, Osrin D, Adler A, et al. Four million neonatal deaths: Counting and attribution of cause of death. Paediatr Perinat Epidemiol 2008; 22:410-416.
- Godinho MA, Murthy S, Lakiang T, et al. Mapping neonatal mortality in India: A closer look. Indian J Community Med 2017; 42:234.
- Baidya M, Shirin M, Saha LC. Transport factors affecting the outcome of referred neonates admitted in a tertiary care hospital. Bangladesh J Child Health 2017; 41:159-64.
- https://www.newbornwhocc.org/SOIN_PRINTED%2014-9-2014.pdf.
- Ghanghoriya P, Agarwal G, Barman ML, et al. Causes and predictors of mortality in newborns referred to tertiary level NICU. J Neonatol 2017; 31:15-21.
- Baqui AH, Darmstadt GL, Williams EK, et al. Rates, timing and causes of neonatal deaths in rural India: implications for neonatal health programmes. Bull World Health Organ 2006; 84:706-713.
- http://seciss.facmed.unam.mx/wp-content/uploads/2021/02/Cloherty-and-Starks-Manual-of-Neonatal-Care-2021-.pdf
- Adikane H, Surwase K, Pawar V, et al. A prospective observational study of morbidity and mortality profile of neonates admitted in neonata intensive care unit of secondary care centre in central Maharastra, India. Int J Contemporary Pediatr 2018; 5:1403-1408.
- Bokade MC, Meshram RM. Mortality and morbidity patterns among outborn referral neonates in central India: Prospective observational study. J Clin Neonatol 2020; 5:168-73.
- Dalal E, Vishal G, Solanki D. Study on neonatal transport at tertiary care centre. IJSR 2013; 84:49.
- Aggarwal KC, Gupta R, Sharma S, et al. Mortality in newborns referred to tertiary hospital: An introspection. J Family Med Prim Care 2015; 4:435-438.
- Rao SK, Bajaj N, Rawat A. Pre transport factors and transport quality affecting the neonatal outcome. J Evolut Med Dent Sci 2015; 4:1991-6.
- Kumar PP, Kumar CD, Venkatlakshmi A. Long distance neonatal transport--the need of the hour. Indian Pediatr 2008; 45:920-922.
- Mudey DG, Tankhiwale DN, Kulkarni DP, et al. Changing pattern of neonatal septicaemia: An epidemiological study conducted at rural tertiary care hospital of central India. Int J Epidemiol 2015; 44:107-107.
- Taksande AM, Yeole M. Risk factors of acute respiratory infection (ARI) in under-fives in a rural hospital of Central India. J Pediatr Neonatal Individualized Med 2016; 5:e050105.
- Patel AB, Simmons EM, Rao SR, et al. Evaluating the effect of care around labor and delivery practices on early neonatal mortality in the global network’s maternal and newborn health registry. Reprod Health 2020; 17:1-1.
- Dangre G, Tankhiwale N, Mudey A. Antimicrobial resistance in neonatal septicaemia: A therapeutic challenge to pediatricians of rural India. Int J Infectious Dis 2012; 16:e412.
- Vinayak D. Neonatal health in India. Indian Pediatr 2008; 45:424.
- Mudey A, Khapre M, Mudey G, et al. Integrated management of neonatal and childhood illnesses-A cost-effective intervention for controlling diarrhoea: Community based study conducted in rural India. Int J Infect Dis 2012; 16:e204.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
R Abhilasha Singh Panwar1*, Sachin Damke1, Keerti Swarnkar1, Amar Taksande1, Revat Meshram1, Sham Lohiya1 and Bhavana Lakhkar2
1Department of Paediatrics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi, Wardha, Maharashtra, India2Department Of Neonatology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi, Wardha, Maharashtra, India
Received: 17-Dec-2021, Manuscript No. JRMDS-21-45004; , Pre QC No. JRMDS-21-45004 (PQ); Editor assigned: 20-Dec-2021, Pre QC No. JRMDS-21-45004 (PQ); Reviewed: 03-Jan-2022, QC No. JRMDS-21-45004; Revised: 06-Jan-2022, Manuscript No. JRMDS-21-45004 (R); Published: 13-Jan-2022
