Research - (2021) Volume 9, Issue 5
A Study to Assess Suicidal Behaviour Among Various Psychiatric DisordersLesions
Divya Balachandran and Nambi S*
*Correspondence: Nambi S, Department of Psychiatry, Sree Balaji Medical College and Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
To assess the prevalence of suicidal behaviour in patients suffering from various psychiatric disorders. To correlate the suicidal behaviour with the socio demographic factors. To compare the suicidal ideation and suicidal intent between common mental disorders and severe mental illness. To compare the suicidal ideation and suicidal intent between common mental disorders and alcohol use disorder.
Keywords
Behaviours, Demographic factors, Severe mental illness, Psychiatric disorders
Introduction
Suicide (Latin suicidium, from sui caedere,"to kill oneself") is the act of intentionally causing one's own death. It is a global public health issue that is a devastating result of a wide range of factors including genetic, socio-cultural, economic, and psychological causes. Suicidal activity and suicidality can be described as a progression of suicidal ideation to attempted suicide and completed suicide [1-3]. World health organization reported that suicide rated for 1.4% of all deaths throughout the world, making it the18th leading cause of death in 2016. It predicts that nearly 1.53 million people will be killed by suicide by2020andfor every person who die by suicide, 10 to 20 times more people may attempt suicide globally. Out of these quite a number will have mental health issues [4].
The stigma of mental illness isa predominant barrier to access health care and arouses negative attitudes and feelings such as shame, disgrace, fear, disgustor hate which results in discrimination and rejection of the individual thus delaying the care of mentally ill [5]. The existence of a psychiatric disorder is invariably reported to be the strongest predictor of suicidal behaviour. It is also stated that 10% of people with mental health issues kill themselves and ninety percent of those who kill themselves will have a psychiatric morbidity. At the same time, it must be noted that only 2%ofthosewho have psychiatric illness commit suicide. Moreover, presence of alcohol dependence greatly increases the risk of suicide with or without a psychological illness. Hence the relationship between suicide, psychiatric illness and alcohol dependence is complex [6]. Among psychiatric disorders, major depressive disorder is the strongest predictors of suicide and suicidal behaviours. Other psychiatric illness in the background of suicide includes schizophrenia, bipolar disorders, anxiety disorders and substance use disorders. Suicidal behaviours amidst individuals with mental illness are one of the commonest psychiatric emergencies that demands a major public health concern by research and mental health task forces [7].
Suicidal risk is an alarming concern in India and as it is a preventable cause of death, identification of patients with mental disorders with suicidal ideation and suicidal intent would be helpful in implementing suicide preventive strategies. Among those who are mentally ill some may have a higher risk of attempting or committing suicide. It is hence important to identify those who are at a higher risk [8]. One of the methods is to identify the suicidal behaviours which points to the risk. This study was done to find out the suicidal ideation and suicidal intent among persons suffering from various mental illness.
Materials and Methods
Setting of the study
This study was done in the outpatient department of Psychiatry, Sree Balaji Medical College & Hospital, Chennai.
Sample
120 persons suffering from psychiatric disorder along with their relatives were recruited, out of which 40 were suffering from common mental disorders, 40 were suffering from severe mental illness and 40 were suffering from alcohol use disorder.
Inclusion criteria
✓ Patients aged 18 to 60 years.
✓ Common mental disorders–Depressive disorders (Major depressive disorder (mild, moderate/Dysthymia), Anxiety disorders (Generalized anxiety disorder, Panic disorder, phobias, Social anxiety disorder, OCD, Posttraumatic stress disorder) and stress related disorders (adjustment disorder, somatoform disorder) as per ICD10diagnostic criteria.
✓ Severe mental illness includes severe depression, bipolar affective disorder, Schizophrenia, and other Psychotic disorders as per ICD 10 diagnostic criteria.
✓ Clinically stable for an interview.
✓ Patients who gave the consent for the study.
Exclusion criteria
✓ Patient less than 18 years and more than60 yearsof age.
✓ Patients uncooperative for the interview.
✓ Patients having dual diagnosis of psychiatric disorder.
✓ Patients suffering from personality disorders.
Methodology of the study
The patients who fulfilled the inclusion and exclusion criteria and diagnosed to have a psychiatric disorder (Depressive disorder, Neurotic & stress related disorders, Schizophrenia, Bipolar affective disorder, Delusional Disorder and other psychotic disorders and Alcohol use disorder) were included in the study along with their relative after obtaining an informed consent.
Statistical methods
Descriptive analysis: Descriptive analysis was carried out by mean and standard deviation for quantitative variables, frequency and proportion for categorical variables. Data was also represented using appropriate diagrams like bar diagram, pie diagram and box plots.
Results
120 patients suffering from psychiatric illness were included in the study population. The mean duration of illness in the sample was 9.61 ± 7.59 years. 65.83% were males and 34.17% were female among the study population (Figure 1). The mean age of the sample was 37.42 (± 8.54(Figure 2).
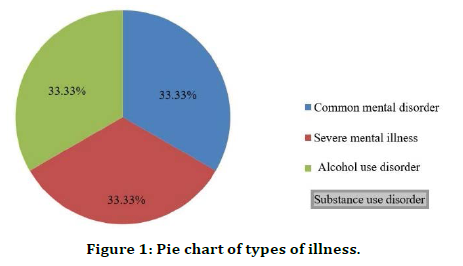
Figure 1. Pie chart of types of illness.
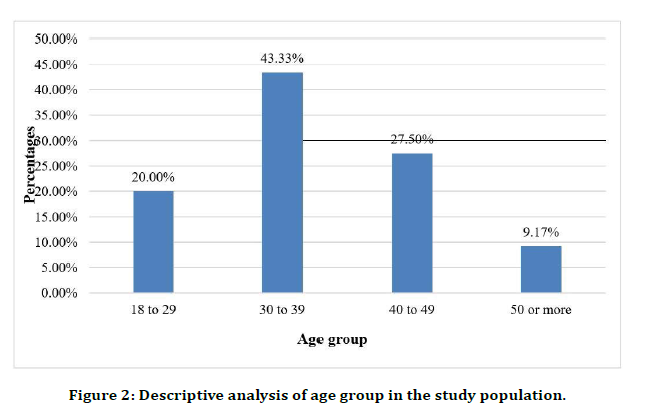
Figure 2. Descriptive analysis of age group in the study population.
Among the common mental disorders 25% had adjustment disorder & somatoform disorder, 25% had anxiety disorder, 25% had depressive disorder, and 25% had obsessive compulsive disorder.
Among the severe mental illness 37.5% had bipolar affective disorder, 37.5% had Schizophrenia and 25% had severe depression & other Psychotic disorders (Table 1).
| Diagnosis | Frequency | Percentages |
|---|---|---|
| Common mental disorders | 40 | |
| Adjustment disorder & somatoform disorder | 10 | 25.00% |
| Anxiety disorder | 10 | 25.00% |
| Depressive disorder | 10 | 25.00% |
| Obsessive compulsive disorder | 10 | 25.00% |
| Severe mental illness | 40 | |
| Bipolar affective disorder | 15 | 37.50% |
| Schizophrenia | 15 | 37.50% |
| Other Psychotic Disorders including severe depression with psychotic symptoms | 10 | 25% |
| Alcohol Use Disorder | 40 | 100% |
Table 1: Diagnosis of the study population.
Out of the study population 30.83% of people had family history of alcohol usage, 30% had family history of psychiatric illness and 9.17% had family history of suicidal death (Figure 3). 10% of the population had diabetes mellitus and Hypertension each followed by 5.8% of hypothyroidism and 1.67% of Bronchial asthma (Table 2).
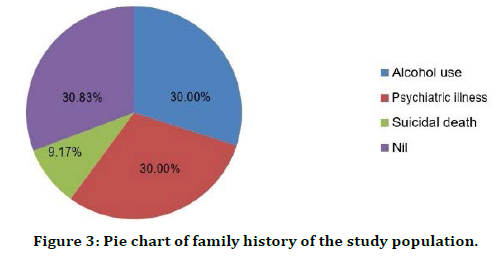
Figure 3. Pie chart of family history of the study population.
| Medical Comorbidity | Frequency | Percentages |
|---|---|---|
| Diabetes mellitus | 12 | 10% |
| Hypertension | 12 | 10% |
| Hypothyroidism | 7 | 5.80% |
| Bronchial asthma | 2 | 1.67% |
| Nil | 87 | 72.50% |
Table 2: Analysis of medical comorbidity in the study population.
The mean HAM A score was 10.12 ± 6.56 in the study population. Among the people with common mental disorder67.5% had mild anxiety, 22.5% had mild to moderate anxiety and 5%had moderate to severe and very severe anxiety each (Table 3). According to the YBOCS rating,20%ofthestudy population had mild symptoms of OCD, 50%had moderate symptoms of OCD and 30% had severe symptoms (Figure 4).
| Anxiety rating | Frequency | Percentages |
|---|---|---|
| Mild severity | 27 | 67.50% |
| Mild to moderate severity | 9 | 22.50% |
| Moderate to severe | 2 | 5% |
| Very severe | 2 | 5% |
Table 3: Hamilton anxiety rating scale.
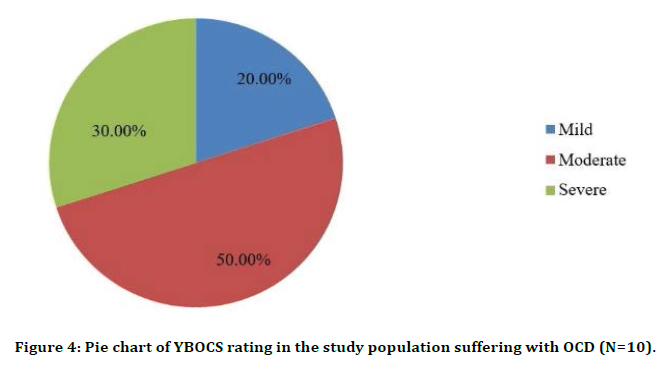
Figure 4. Pie chart of YBOCS rating in the study population suffering with OCD (N=10).
Alcohol use disorder (N=40)
Based on the audit scale used for alcohol usedisorder,5% of the participants were at a high-risk group for addiction while 95% were addicted to alcohol. In persons with Alcohol use disorder 35% of persons had mild depression, 25% persons had moderate depression, 7.5% persons had severe depression and 12.5% of persons had very severe depression. The mean HAM D score was 13.7 ± 6.35 (Figure 5).
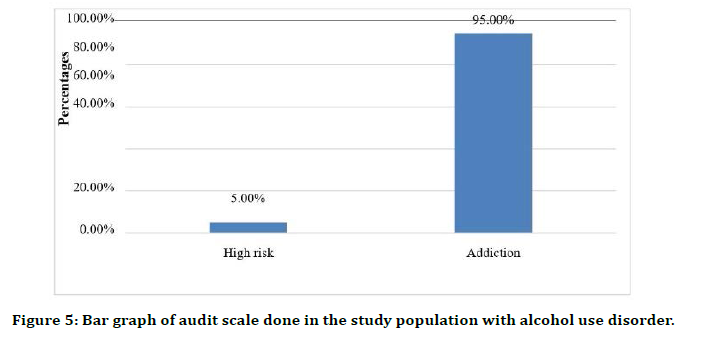
Figure 5. Bar graph of audit scale done in the study population with alcohol use disorder.
In people with Alcohol use disorder 28 (70%) participants had mild anxiety, 7 (17.50%) participants had mild to moderate anxiety and 2 (5%) participants had moderate to severe and 3 (7.50%) participants had very severe anxiety (Table 4). The mean HAM A score was 10.12 ± 6.56.
| Anxiety rating | Frequency | Percentages |
|---|---|---|
| Mild severity | 28 | 70.00% |
| Mild to moderate severity | 7 | 17.50% |
| Moderate to severe | 2 | 5.00% |
| Very severe | 3 | 7.50% |
Table 4: Hamilton anxiety rating scale in persons with alcohol use disorder.
Among the study population with common mental disorders 25% had a history of financial stressor, 7.5% had history of occupational stressor and 37.5% had a history of social/ environmental stressor (Table 5).
| Psychosocial Stressor | ||||
|---|---|---|---|---|
| Types of Illness | Financial | Occupational | Social/Environmental | Nil |
| Common Mental Disorders (N=40) | 10 (25%) | 3 (7.5%) | 15 (37.5%) | 12 (30%) |
| Severe Mental Illness (N=40) | 10 (25%) | 0 (0%) | 15 (37.5%) | 15 (37.50%) |
| Alcohol Use Disorder (N=40) | 4 (10%) | 2 (5%) | 9 (22.5%) | 25 (62.50%) |
Table 5: Comparison of psychosocial stressor between type of illness (N=120).
In people with severe mental illness 25% had history of financial stressor, 5% had history of social/environmental stressor and none reported to have occupational stressor. Among the persons with alcohol use disorder 10%had history of financial stressor, 5% had history of occupational stressor and 22.5% had history of social / environmental stressor.
Family history of psychiatric illness were found among 33.3% of persons with suicidal ideation and 20% of persons who attempted suicide among the study population.
Family history of alcohol use was found among 25% of persons with suicidal ideation and 33.3%ofpersonswho had attempted suicide. Family history of suicidal death were found among 16.7%of persons who had suicidal ideations and among 26.7% of persons who had attempted suicide in the study population.
Suicidal ideation
Out of the study population 30% had current suicidal ideation. Among people with common mental disorders, 35% had current suicidal ideation (Table 6).
| Types of illness | Current Suicidal Ideation | Chi square | P-value | |
|---|---|---|---|---|
| Present | Nil | |||
| Common mental disorders (N=40) | 14 (35%) | 26 (65%) | 6.667 | 0.036 |
| Severe mental illness (N=40) | 16 (40%) | 24 (60%) | ||
| Alcohol use disorders (N=40) | 6 (15%) | 34 (85%) | ||
| The mean severity of ideation was 9.77 ± 5.19. | ||||
Table 6: Suicidal ideation between the types of illness.
Suicidal attempt
Out of the study population 12.5% had currently attempted suicide. 15% of patients who suffered from common mental disorder had attempted suicide in the past one year. 10% of patients suffering from severe mental illness had attempted suicide within one year. 12.5% of the sample who had alcohol use disorders had attempted suicide in the past year. However, this difference was not statistically significant (P value 0.796) (Table 7). Figure 6 shows the comparison of current suicidal ideation between types of illness. Table 8 shows the comparison of suicidal ideation and suicidal attempt between individual disorders.
| Suicide attempt | Chi square | P-value | ||
|---|---|---|---|---|
| Types of illness | Yes | Nil | ||
| Common mental disorders (N=40) | 6 (15%) | 34 (85%) | 0.457 | 0.796 |
| Severe mental illness (N=40) | 4 (10%) | 36 (90%) | ||
| Alcohol use disorder (N=40) | 5 (12.5%) | 35 (87.5%) | ||
Table 7: Suicidal attempt between types of illness.
| Diagnosis | Sample size | Suicidal ideation | Suicidal attempt |
|---|---|---|---|
| Depressive disorder (mild & moderate ) | 10 | 6 (60%) | 4 (40%) |
| Anxiety disorder | 10 | 2 (20%) | 0 (0%) |
| OCD | 10 | 3 (30%) | 0 (0%) |
| Adjustment & somatoform disorder | 10 | 3 (30%) | 2 (20%) |
| Schizophrenia | 15 | 5 (33.33%) | 1 (6.7%) |
| BPAD | 15 | 7 (46.7%) | 1 (6.7%) |
| Other psychotic disorders including severe depression with psychotic symptoms | 10 | 4 (40%) | 2 (20%) |
| Alcohol use disorder | 40 | 6 (15%) | 5 (12.5%) |
Table 8: Comparison of suicidal ideation and suicidal attempt between individual disorders (N=120).
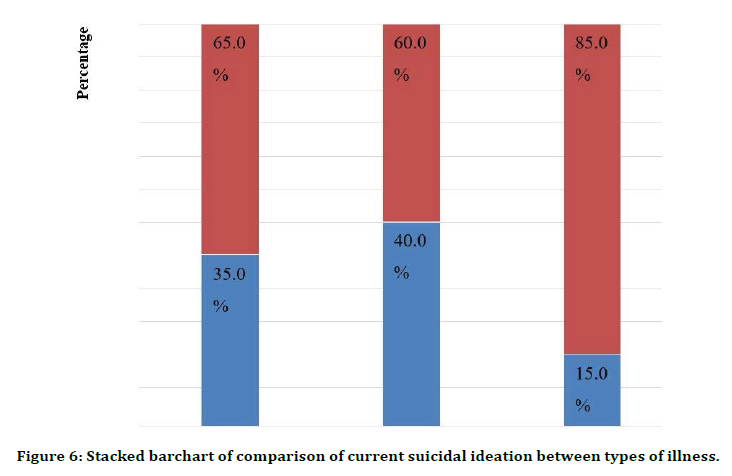
Figure 6. Stacked barchart of comparison of current suicidal ideation between types of illness.
Among the study population who had attempted suicide 13.33% had low suicidal intent and they were suffering from common mental disorder (Table 9). Figure 7 shows the severity of suicidal intent among the study population.
| Disorder | Low intent | Medium intent | High intent |
|---|---|---|---|
| Common mental disorders | 2 (13.33%) | 2 (13.33%) | 2(13.33%) |
| Severe mental illness | nil | 1(6.7%) | 3(20%) |
| Alcohol use disorder | nil | 1(6.7%) | 4(26.7%) |
Table 9: Severity of suicidal intent (N=15).
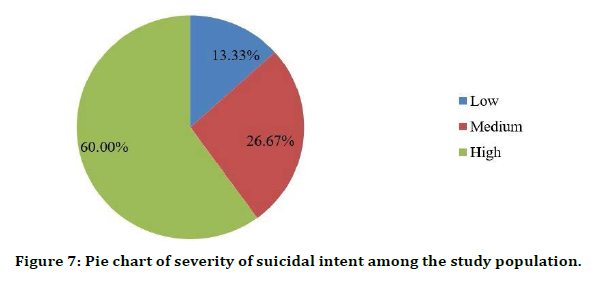
Figure 7. Pie chart of severity of suicidal intent among the study population.
Discussion
120 persons suffering from psychiatric illness were included in the study, out of which 40 were suffering from common mental disorders, 40 were suffering from severe mental illness and 40 were suffering from alcohol use disorder. The mean age of the sample was 37.42(±8.54) since the age selection criteria was set to be above 18th mean age possibly was higher than the Indian mean age. In our current study Suicidal ideation was significantly high in the 4th decade and suicidal attempts were in the 3rd decade which was consistent with the NCRB 2014 reports [9].
Suicidal behaviour was predominantly seen in the younger age group which correlates with studies who reports that the peak incidence of suicidal behaviour was noted in the age group of 15 -44 years [10]. Most suicides occurred intheagesbetween15 and 44 years, with age groups 15 ‐29 and 30‐44 years having almost equal distribution [11]. About 65.83 % of the study population were males and the remaining 34.17% were females. This was because of exclusive presence of men in the alcohol use disorder group. But in most of the studies men have a higher preponderance when completed suicides are considered. Women are more in having suicidal ideations.
In our study population, Suicidal ideation had a preponderance in female while suicidal attempts were more common among males which isin line with previous study. A study conducted by Srivastava et al reported that the proportion of males committing suicide was significantly higher than females, with male to female ratio of almost 70:30 [12].
6.67% belonged to lower socioeconomic status,53.33% belonged to lower middle class, 29.17% belonged to upper lower class and 10.83% belonged to upper middle class. This is in tune with the hospital attending population of this department. Suicidal ideation and attempt were remarkably high among lower middle socioeconomic status which couldbe due to the selection of sample from that particular group.
Based on the family history, out of the 36 who had suicidal ideation from the study population 33.33% had a history of psychiatric illness followed by 25% & suicidal death who had history of alcohol use and suicidal death respectively The present study revealed that among the 40 persons suffering from common mental disorder 14 persons (35%) had suicidal ideation.
Individuals with major depressive disorder had 60% of suicidal ideation, which was consistent [13]. In our study population, 100% of the individuals with major depressive disorder who attempted suicide had suicidal ideations. A study by Sokero et al [12] also identified that, 95% of who had attempted suicide had suicidal ideation [14-16].
Among persons suffering from schizophrenia, 33.33% had suicidal ideation out of which 6.66% had attempted suicide. Earlier studies in individuals with schizophrenia reported that the attempted suicide ranged from 20 to40% [19] and lifetime prevalence of suicide was reported as 4.9% [17]. The variation in the results could be explained by the smaller sample size.
Study conducted by Singh et al showed that more than 60% Schizophrenic spectrum disorders correlated psychotic symptoms as a source for wanting to commit suicide, while more than 50% patients with affective disorders related this to family and personal stressors [18]. Among the 15% who had suicidal ideation, 5(12.5 %) had attempted suicide which was in line with an earlier study that identified that 10% of patients with alcohol dependence syndrome reported suicidal ideas, out of which 7% had attempted suicide [19].
Study by Bhattacharjee et al demonstrated that there was a higher rate of suicide attempt with alcohol use prior to the suicide attempt and it revealed that 17 percent of suicide attempt victims had a record of alcohol intake before the suicide attempt [20]. In our study among the 5 persons whoattempted suicide, 4 had high suicidal intent while one had a medium suicidal intent.
Conclusion
✓ Suicidal ideation was found to be more in persons suffering from severe mental illness (40%) followed by common mental disorders (35%) and Alcohol use disorder (15%) .
✓ Suicidal attempt in the past one year was found to be high in persons suffering from common mental disorders (15%) followed by alcohol use disorder (12.5%) and severe mental illness (10%).
✓ Severity of suicidal intent was found to be high in persons suffering from Alcohol use disorder (26.7%) followed by severe mental illness (20%) and common mental disorders (13.33%).
✓ In persons suffering from common mental disorders, those with depressive disorder had the highest suicidal ideation (60%) and suicidal attempt (40%).
✓ In persons suffering from severe mental illness, those with Bipolar affective disorder had the highest suicidal ideation (46.7%) followed by other psychotic disorders.
✓ Women had a higher rate of suicidal ideation whereas men had higher rate of suicidal attempt.
✓ Suicidal behaviour was found to be highin patients with family history of psychiatric illness and among lower middle class.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Sohaib SA. The role of MRI and ultrasound in patients with adnexal masses. Clin Radiol 2005; 60:340-348.
- Cambell S, Newman GB. Growth of fetal biparietal diameter during normal pregnancy. J Obstet Gynaecol Brit Cwelth 1971; 78:513-519.
- Curry TS, Dowdey JE, Murry RC. Christenses physics of diagnostics radiology. Lea Febiger, 4th edition, 1990.
- Bloch F, Hasen W.W, Packward ME, Nuclear Induction, Phys Rev 1946; 69:127.
- Hawkes RC, Holland GN, Moore WS, et al. Nuclear magnetic resonance (NMR) tomography of the brain: A preliminary clinical assessment with demonstration of pathology. J Computer Assisted Tomography 1980; 4:577-586.
- Rumack CM, Wilson SR. Diagnostic ultrasound, 4th edition, p556 -598.
- Vilaro MM, Rifkin MD, Pennell RG, et al. Endovaginal ultrasound. A technique for evaluation of nonfollicular pelvic masses. J Ultrasound Med 1987; 6:697-701.
- Neeharika C, Ravindran C. Ultrasound and magnetic resonance imaging correlation of adnexallesions. Annals Romanian Society Cell Biol 2021; 3404-3418.
- Levine D. Pelvic doppler seminars in ultrasound, CT and MRI. 1999; 20:239-249.
- Long MG, Boultbee J, Begent RH, et al. Doppler ultrasound of the uterine artery and uterus in invasive mole and choriocarcinoma. Br J Radiol 1987; 60:621.
- Adusumilli S, Hussain HK. MRI of sonologically indeterminate adnexal masses. AJR 2006; 87:732 -740.
- Outwater EK, Sieeelman ES, Chiowanich P, et al. Dilated fallopian tubes: MR imaging characteristics. Radiology 1998; 208:463-469.
- Ha HK, Lim GY, Cha ES, et al. MR imaging of tubo ovarian abscess. Acta Radiol 1995; 36:510 -514.
- Noone TC, Semelka RC, Worawattanakul S, et al. Intraperitoneal abscesses: diagnostic accuracy of and appearances at MR imaging. Radiology 1998; 208:525-528.
- Jain KA. Imaging of peritoneal inclusion cysts. AJR Am J Roentgenol 2000; 174:1559 -1563.
- Kurachi H, Murakami T, Nakamura H, et al. Imaging of peritoneal pseudocysts: value of MR imaging compared with sonography and CT. AJR Am J Roentgenol 1993; 161:589 -591.
- Kim JS, Lee HJ, Woo SK, et al. Peritoneal inclusion cysts and their relationship to the ovaries: evaluation with sonography. Radiology 1997; 204:481-484.
- Sala EJ, Atri M. Magnetic resonance imaging of benign adnexal disease. Top Magn Reson Imaging 2003; 14:305-327.
- Togashi K, Ozasa H, Konishi I, et al. Enlarged uterus: Differentiation between adenomyosis and leiomyoma with MR imaging. Radiology 1989; 171:531-534.
- Kim JC, Kim SS, Park JY. "Bridging vascular sign" in the MR diagnosis of exophytic uterine leiomyoma. J Comput Assist Tomogr 2000; 24:57-60.
- Fleischer AC, Kalemeris GC, Entman SS. Sonographic depiction of the endometrium during normal cycles. Ultrasound Med Biol 1986; 12:271-277.
- Lisa Bame Schwartz, Ellen Panageas. Female pelvis: Impact of MR Imaging on treatment decision and net cost analysis. Radiology 1994; 192:55 -60.
Author Info
Divya Balachandran and Nambi S*
Department of Psychiatry, Sree Balaji Medical College and Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Divya Balachandran, Nambi S, A Study to Assess Suicidal Behaviour Among Various Psychiatric Disorders, J Res Med Dent Sci, 2021, 9 (5):290-297.
Received: 02-Apr-2021 Accepted: 24-May-2021
