Research - (2020) Volume 8, Issue 6
A Systematic Review on Periodontal Disease
Pragati S Dubey* and Neelam Mittal
*Correspondence: Pragati S Dubey, Faculty of Dental Sciences, Institute of Medical Sciences, Banaras Hindu University, Varanasi, India, Email:
Abstract
Periodontal diseases are consisting wide range of inflammatory conditions which causes degeneration of Periodontium and affects all supporting structures of teeth such as gingiva, periodontal ligament, cementum, and alveolar bone etc. followed by teeth loss. WHO had reported about 10-15% of world population is suffering from severe periodontal condition? It is complex infectious disease caused by aggressive microbial growth on teeth. The main aim of this study is to provide systemic update on periodontal disease regarding its stages, occurrence, pathophysiology, diagnosis, treatment, and management. The pathophysiology of periodontal disease is associated with dental plaque, microbial biofilm formation and immunogenicity of host cell. The severity of this disease depends upon risk factors and chronological stages. Prevention is attained by daily maintenance of oral hygiene. Various surgical and non-surgical treatments are available to control the formation of microbial biofilm. Daily maintenance and periodic management of this disease control worsening of condition and shows definite improvement in oral health.
Keywords
Periodontal diseases, Pathophysiology, Oral health, Diagnosis, Periodontal ligament
Background
Periodontitis is an infection of Periodontium. Whereas the word ‘Perio’ means gingiva and other tissues surrounding teeth, ‘don’t’ mean tooth and ‘itis’ means inflammation, So the whole term “Periodontitis” indicates chronic inflammation of gingiva [1] periodontal ligaments, alveolar bone and dental cementum. According to World Health Organization (WHO) it is widely spreadable chronic disease around the world [2]. It begins with accumulation of plaque around teeth which form microbial biofilms with bacteria followed by localized inflammation of gingiva. Negligence of this situation causes chronic condition of periodontal disease. At this stage damage of periodontal structure occurs by baleful byproducts and enzyme from periodontal bacteria such as leukotoxins, collagenase, fibrinolysis and other Bacteroids spp.: B. intermedius and B. gingivalis, fusiform organisms: Actinobacillus actinomycetemcomitans, Wollina recta and Eikenella spp, Porphyromonas gingivalis, Taneerella forsynthesis and various bacilli and cocci, spirochetes, and amoebas and trichomonads [3,4].
By maintaining good oral hygiene, it can be reversed at initial stage but if plaque is not removed at this stage then formation of tartar or calculus occur which is not removable by using toothbrush or floss. Because of this tartar, bacteria start attacking deeper tissues due to which periodontal ligaments around teeth gets degraded and leads to resorption of alveolar bone [5]. A space between gingiva and tooth occurs which is referred as “Periodontal Pocket” and this condition is mainly known as periodontitis or periodontal disease. The severity of this disease depends upon microbial plaque formation [6].
The screening and examination of this disease has been done by various methods, which results in detection of severity of periodontal ligament. Several tests are there to diagnose the periodontal disease such as radiograph technique, hematological screening, laser treatment, tissue engineering, etc. To control the progression of disease there are many treatment options available (surgical as well as non-surgical) depend upon the chronology of disease. The maintenance of this disease is done by intensive care and by sustaining good oral hygiene [7,8].
Stages
There are four stages of periodontal disease which are as follows [9,10]:
Gingivitis: It is the only stage when periodontitis can be reversible. At this stage the plaque formation around teeth occurs. There are mainly few painless symptoms seen at this stage such as bad breath, swollen reddish gums and bleeding while brushing and flossing. It can be reversed by maintaining good oral hygiene and regular checkups.
Early stage: It is the second stage of periodontal disease. It is manageable by oral hygiene but not reversible. At this stage, the infection starts spreading to surrounding tissues and starts degrading it. Symptoms at this stage include inflammation of gums, severe bad breath, and bleeding during brushing or flossing, spacing between teeth become evident and will gradually increase.
Moderate stage: Like second stage moderate stage cannot be reversed. Same symptoms as moderate stage occurs but space between teeth and recessions of gums are more evident. Treatment like deep cleaning, scaling and flap surgeries can be done at this stage.
Advanced stage: Last stage of periodontal disease; wherein 50-90% of loss of periodontal tissues occurs. Also, other symptoms like swollen gums that ooze of pus, cold sensitivity, loosening of teeth, painful chewing and severe halitosis occurs. If left untreated it causes more spaces or gaps between teeth and gums, gum recession, patient needling dentures, and other health problems that can be worst. Treatment includes regular checkups, cleaning and maintaining good oral hygiene can help halt the progression of periodontitis (Figure 1).
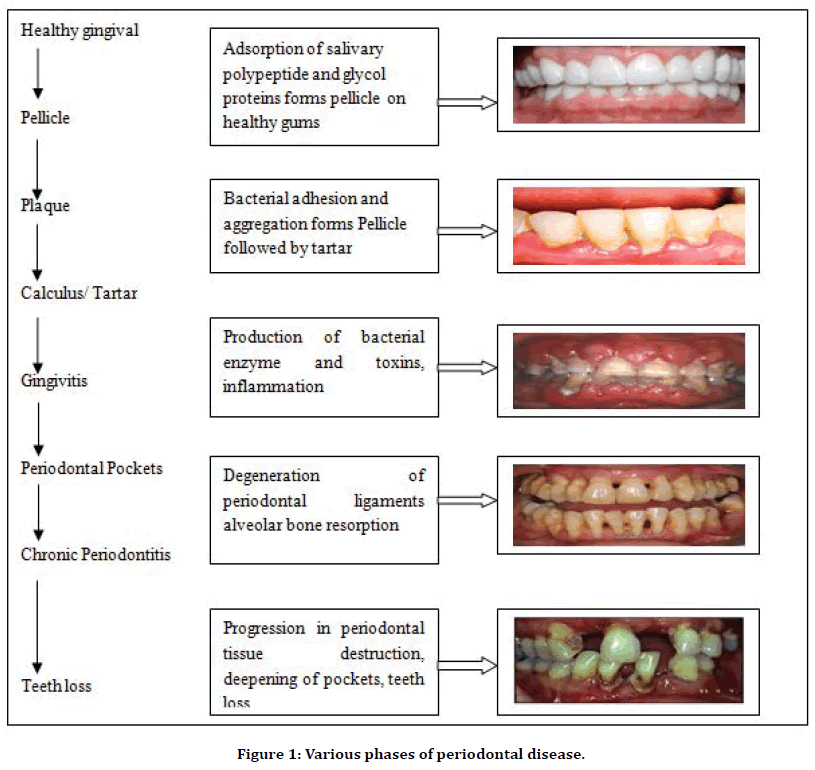
Figure 1. Various phases of periodontal disease.
Types of Periodontitis [11-13]
Gingivitis: As described above, gingivitis is inflammation of gums and can be reversed by maintaining oral hygiene.
Chronic periodontitis: In this type of periodontal disease, symptoms may include chronic inflammation of gums, severe bad breath, and bleeding during brushing or flossing occurs. Loss of epithelial tissue, bone and ligaments which is not reversible.
Aggressive periodontitis: It can be present in localized or generalized forms, both are early onset form of chronic periodontal inflammatory disease, typical manifesting between puberty and early third decade of life. The symptoms are same as chronic periodontitis.
Necrotizing ulcerative gingivitis: It is mainly occurring in people who are suffering from malnutrition, immune suppressive and HIV. Necrosis means death of cell or living tissue. It mainly occurs due to deficiency of nourishment needed by people to remain healthy.
Systemic chronic periodontitis: This type of chronic periodontal disease happens in patient who have systemic syndrome. Inflammation of gums occurs due to systemic disease such as Diabetes, Heart disease, Respiratory disease, etc.
Occurance and Epidemiology
Periodontal disease is mainly prevalent in adults, but it may also occur in children and adolescents [14]. Prevalence of periodontal disease depends on level of dental plaque formation and tissue destruction of gingiva. Site specificity is the key features for chronic and aggressive periodontitis. The severity of this disease depends upon depth of periodontal pocket i.e. attachment loss and bone loss of tooth [15].
The epidemiology of periodontitis may vary across populations substantially. Frequently used parameters to collect data for occurrence of this disease are clinical attachment loss and probing depth of periodontal pockets which was first introduced by US centers for Disease Control Prevention and American Academy of Periodontology [16].
There are various studies conducted by researchers to find out prevalence rate in different countries. Globally 10-15% of populations are suffering from tooth loss due to periodontal disease [17]. A study was conducted in Gautemala in the year of 2001 reported that out of 122 patients, attachment loss was found about 3 and 6 mm in 100% and 56% of overall individuals. Afterward in 2003, another clinical study reported that out of 359 patients of rural Thai population, 92% were diagnosed with higher prevalence of periodontitis with age group of 30-32 years [13]. Also, in 2017, another study was conducted in South India among 1000 individuals who showed prevalence rate of chronic periodontitis among different strata of sample populations (Table 1). Similarly, another clinical study conducted by researchers in 2018 about prevalence rate of periodontitis among different age group of people of South India (Figure 2).
| Population | Periodontitis prevalence (n=1000) | Prevalence percentage n (%) |
|---|---|---|
| Male | 252 | 42.4 |
| Female | 171 | 42.1 |
| Hypertension | 19 | 44.2 |
| Diabetes Type-II | 25 | 43.9 |
| Cigarette smoking | 53 | 44.9 |
| Alcohol consumption | 60 | 39.7 |
| Pan chewing | 35 | 43.2 |
Table 1: Prevalence rate in different strata of sample population.
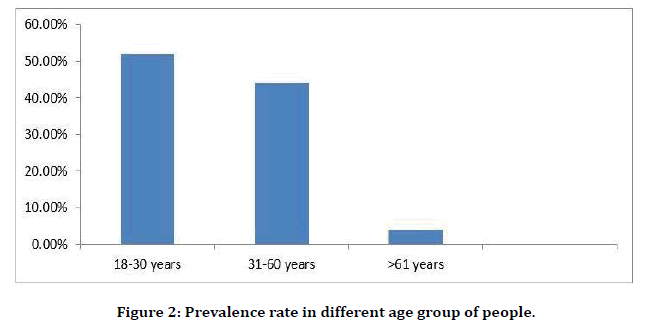
Figure 2. Prevalence rate in different age group of people.
Risk factor: There are two kind of risk factor in case of periodontal disease in which one is modifiable, and another is non-modifiable [18]. Cigarette smoking is one of the vital modifiable risk factors for chronic periodontal disease. Higher progression of microbial film is severe in smokers than nonsmokers and more worsen chronic condition occurs due to habit of smoking [19]. Most prevalent systemic disease is diabetes mellitus predispose to periodontitis. In diabetic patient, prevalence of periodontitis occurs more readily as compare to other immunological diseased patients [20]. Stress is also another consideration as immunosuppression and necrotizing ulcerative gingivitis occurs mainly due to stress [21]. There are many risk factors associated with this disease are given as (Table 2):
| Modifiable risk factor | Non-modifiable risk factor |
|---|---|
| Microorganisms (specific pathogen) | Osteoporosis |
| Smoking | Some hematological disorders |
| Poorly controlled diabetes mellitus | History of periodontitis |
| Stress | Age |
| Poor self-care | Gender |
| Untreated human immunodeficiency virus or acquired immunodeficiency syndrome | Race |
| Oral effects of some metabolism | Genetic disorders |
| Local factors | Bone level |
| Obesity | Drug-induced disorders |
| Improper diet | Some host response |
| Chronic inflammation | Bone levels |
| Some host responses | Normal hormonal variations (e.g. Pregnancy) |
Table 2: Types of risk factor in periodontitis.
Pathophisiology
The dental plaque or calculus: Periodontitis and gingivitis are mainly initiated with dental plaque. There are around 150 species of microbes are found in single person and overall, 800 different types of species of microbes have been identified in calculus of tooth. The species include Gram negative anaerobic bacteria, spirochete and even virus. The imbalance between these microbes’ forms ‘pathogenic unit’ in case of chronic periodontal disease (Figure 3) [22].
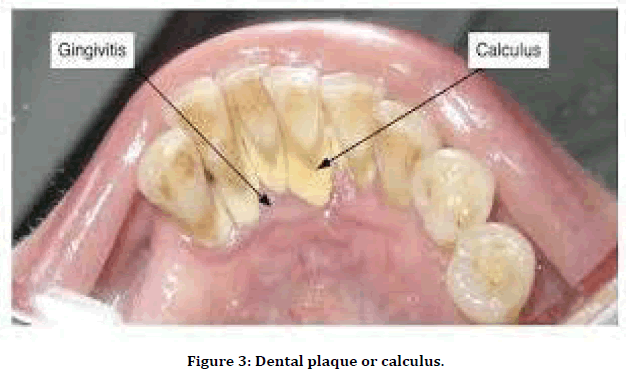
Figure 3. Dental plaque or calculus.
Microbial biofilms: As we discussed earlier, microbial biofilm initiates gingivitis. The progression of microbial biofilm depends upon dysbiotic ecological changes in baleful byproducts and enzyme which results in degradation of periodontal tissue. Microbial biofilms are kind of matrix fixed with different microbial species colony, sticking with each other on tooth surface [23]. There are seven stages of plaque biofilm formation are given as follows (Table 3):
| No. | Stages | Features |
|---|---|---|
| 1 | Pellicle formation | Occurs by adsorption of Host and bacterial molecules, salivary glycoprotein on tooth surface |
| 2 | Transport | Occurs via natural salivary flow, transport of bacteria such as Neisseria, Streptococcus sanguis, S. oralis, S. mitis and Actinomyces to the pellicle occurs. |
| 3 | Long range interactions | This stage leads to reversible adhesion with Vander Wall’s and electrostatic forces between microbial cell surface and the pellicle. |
| 4 | Short range interactions | This stage leads to irreversible interaction between microbial cell surface and pellicle. |
| 5 | Co-aggregation | Increased micro flora diversity due to co-adhesion of new microbes over already attached microbes. |
| 6 | Multiplications | Multiplication of adhered bacteria on tooth surface lead to severity of periodontal disease. |
| 7 | Detachments | Detachment of colonies to the new site for confluent growth. |
Table 3: Stages of microbial biofilm formation.
Immunogenicity: Not only microbial films are responsible for pathogenesis of periodontal disease but also host cells immune system is responsible for degradation of periodontal ligaments [24]. The balance between microbial biofilm and host cell is lost due to which remarkable variance in both dental plaque and host immunity system occurs, which results in increment of inflammatory cells leads to degradation of periodontal tissue and bone [25]. Therefore, decrease of anti-inflammatory cells such as neutrophils, lymphocytes, granulocytes, etc. due to chronic persistence of microbial biofilms which results in severity of alveolar bone resorption by osteoclast and leads to degradation of ligament fibers followed by chronic periodontitis (Figure 4) [26].
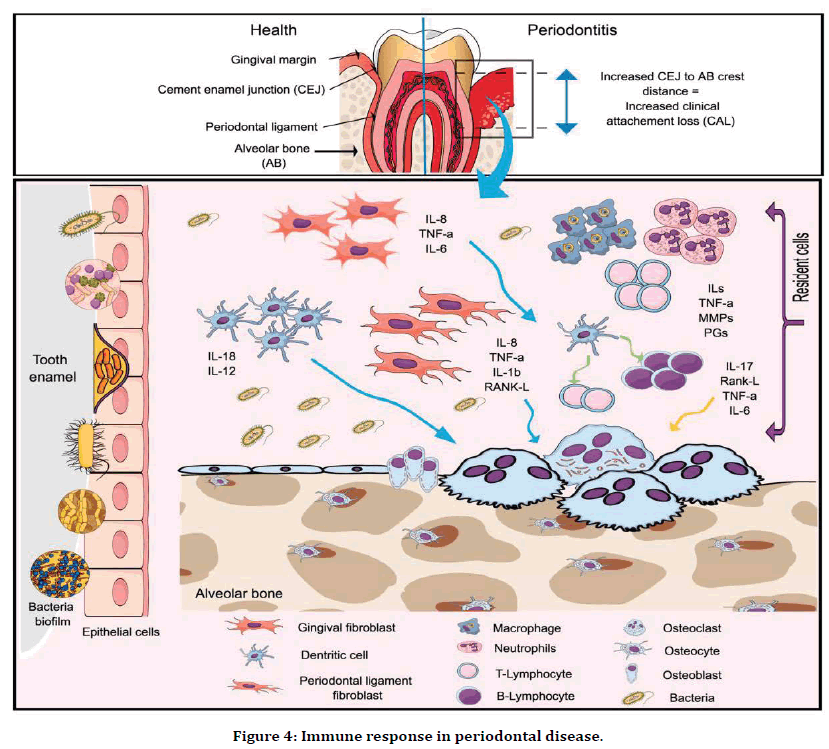
Figure 4. Immune response in periodontal disease.
Periodontal Screening and Examination [27,28]
The dental examination starts with an extra cellular and intra cellular oral examination of soft and hard tissues. The periodontal examination includes these following steps as follows:
General description like:
Quantitative assessment of oral hygiene and presence of calculus deposits.
Presence of gingival inflammation and recession.
Tooth migrating and related problems.
Identification of local periodontal risk factors.
Periodontal screening using Basic Periodontal Examination and Recordings.
Detailed examination of ligament degradation and periodontal pocket depth as (Figure 5)
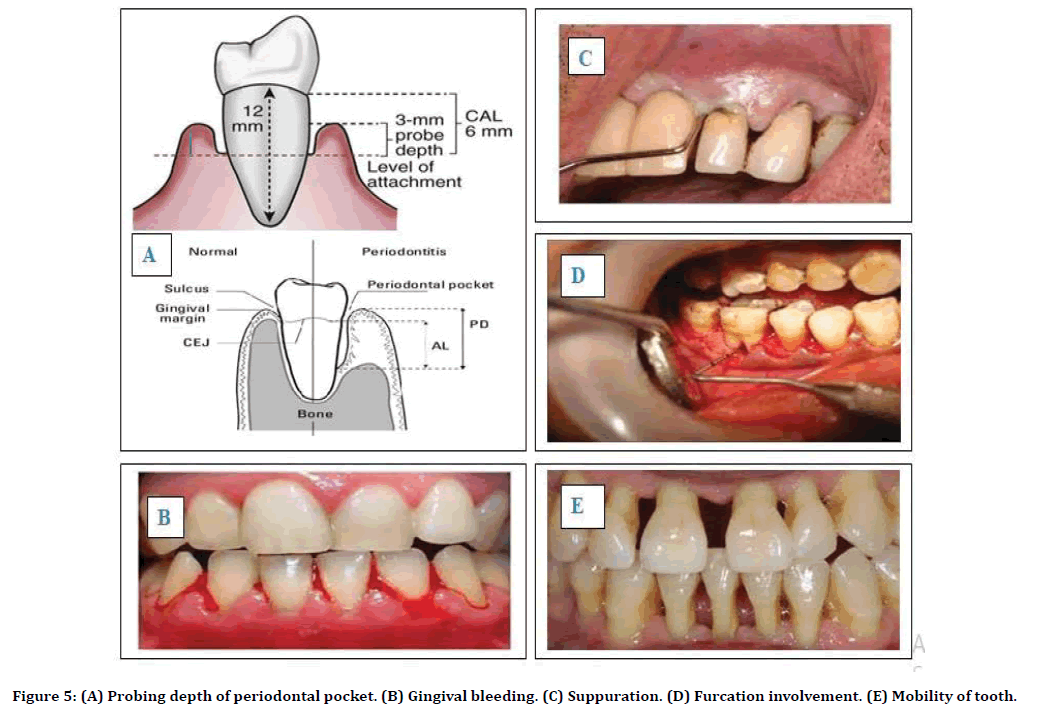
Figure 5. (A) Probing depth of periodontal pocket. (B) Gingival bleeding. (C) Suppuration. (D) Furcation involvement. (E) Mobility of tooth.
Probing depth of periodontal pocket, attachment loss and recession.
Bleeding.
Suppuration.
Furcation involvement.
Mobility of tooth.
All these parameters are measured on six sites per tooth such as mesiobuccally, buccal, distobuccal, mesiolingual, midlingual and distolingual, and all these readings are recorded in periodontal chart.
Diagnosis of periodontal disease has been done by following investigations are given as:
Radiograph
Periapical radiograph, Bitewing radiographs, Panoramic X-ray, or combination of all these is used to diagnose the prognosis of patients. Radiograph provides detailed information about patient’s tooth condition. The degree of bone loss and depth of periodontal pocket can be assessed by using Radiograph and pattern and amount of bone loss (Table 4).
| Radiograph types | Parameters |
|---|---|
| Periapical radiograph | Long cone parallel technique. |
| Good clarity of images as compared to horizontal radiograph. | |
| Time consuming process. | |
| Horizontal bitewings radiograph | Use for caries detection. |
| Alveolar crest can be visualized. | |
| Provides good quality of image for bone loss. | |
| Vertical bitewing radiograph | Shows 90° angle bitewing film image. |
| Better quality of image for extensive bone loss | |
| Panoramic radiograph | All teeth seen in one image or film. |
| Newer machine generated for good quality of images. | |
| Details are much fine as compared to intraoral radiographs. |
Table 4: Types of radiograph and their parameters.
Vitality test
Electric Pulp tester or Thermal stimuli is used to diagnose the pulp vitality of tooth.
Other tests
Full hematological screening.
Blood glucose level test.
INR or microbial plaque sampling.
Treatment and Management
Treatment plan for periodontal disease are divided into three phases as follows (Figure 6)
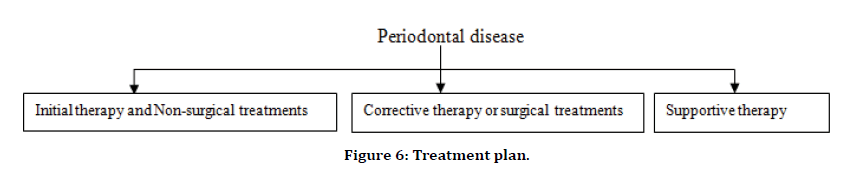
Figure 6. Treatment plan.
Initial therapy
This therapy is given at initial stage of gingivitis to control the microbial plaque formation and identify any modifiable risk factor [32]. Giving advice to the patients regarding oral hygiene technique, cessation of habits like smoking, alcohol consumption, chewing pan masala, etc. and also doctors gives instruction regarding type of toothbrush to be use, use of interdental aids, dentifrices or mouthwash, etc. [33]. If periodontal risk factors like Diabetes mellitus identified, then patient should be advised accordingly. The therapy is revaluated after 8-12 weeks because 6 weeks is minimum period for healing of tissue or periodontal ligaments. The initial treatment includes following therapies:
Tooth brushing: Manual and electronic toothbrush are available to remove dental plaque. Robinson et al in 2005 reported in this study that oscillating, rotating, powered toothbrush shows more efficiency in removing dental plaque [34].
Interdental cleaning: An effective toothbrush can clean only 65% of tooth surface but do not remove overall dental plaque, so interdental cleaning is also necessary to clean the microbial biofilms such as dental floss, tape, and powered flossing device. When interdental papillae completely embrasure then dental floss and tape are advised to the patient which helps to improved periodontal clinical outcomes (Figure 7) [35].
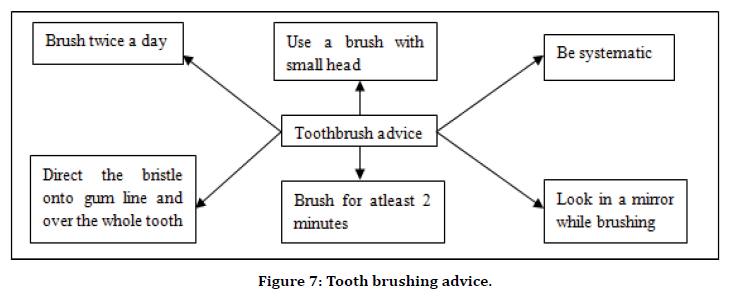
Figure 7. Tooth brushing advice.
Adjunctive Pharmacological agent: Many Pharmaceutical aids have been added into mouthwashes and toothpaste to increase the efficiency of the product. Widely used agent like Chlorhexidine Gluconate is considered as gold standard anti-plaque/ anti-gingivitis agent [36]. It is mainly added into mouth wash, gel, or toothpaste. There are various examples of adjunctive aids are given as (Table 5):
| Compounds | Pharmacological aids |
|---|---|
| Bisguanidine | Chlorhexidine gluconate |
| Enzyme | Protease, dextranase |
| Quaternary ammonium compounds | Cetyl pyridinium chloride |
| Phenols | Triclosan |
| Essential oils | Thymol, eucalyptol |
| Metal ions | Zinc, stannous fluoride |
| Oxygenating agents | Peroxide |
Table 5: Adjunctive pharmacological agents.
Non-surgical treatment [37,38]
At initial stage of gingivitis, the treatment may be less aggressive as given as:
Scaling: Scaling helps to remove calculus and microbial biofilms from gums. It may be operated by using hand instruments or by ultrasonic device.
Root planning: Root planning helps to smooth the root surface and inhibiting further buildup of tartar. It also removes baleful byproducts to reduce the inflammation and increase healing of attachment of gums to tooth surface.
Antibiotics: Topical or Oral antibiotics are used to control the formation of microbial biofilms. Topical antibiotics such as insertion or gels or implants etc. are inserted in gingival sulcus or in periodontal pockets. However, Oral antibiotics eliminate infection caused by bacteria on gums and teeth surfaces.
Corrective therapy or surgical treatments [39-42]
There are several surgical treatments to treat periodontal disease are as follows (Table 6):
| No. | Surgical Treatments | Features |
|---|---|---|
| 1. | Flap surgery | Pocket reduction surgery. |
| Incision on gum tissue for better healing. | ||
| 2. | Soft tissue grafting | Removal of small tissue from palate. |
| Use for reducing gum recession. | ||
| 3. | Bone grafting | Bone grafting of small fragment from own, synthetic or donated bone. |
| Helps in tooth loss problems and regrowth of natural bone. | ||
| 4. | Tissuestimulating proteins | Applying gel to a diseased tooth root. |
| Gel helps in developing tooth enamel and stimulates growth of bone and tissue. | ||
| 5. | Reparative surgery | Modified windman flap technique. |
| Use for better access and direct vision to root surface of debridement. | ||
| 6. | Resective surgery | Gingivectomy. |
| Removal and reshaping of tissue occur. | ||
| 7. | Regenerative surgery | Regeneration of Periodontium. |
| Regrowth of bone that destroyed by bacteria. | ||
| Example as tissue regeneration or enamel matrix derivation. | ||
| 8. | Other surgery | Occlusal adjustment. |
| Endodontitis. | ||
| Extraction of microfilm. | ||
| Fixed/ Removal prosthodontics. | ||
| Implants. | ||
| Host modulation therapy. | ||
| Orthodontics. | ||
| Laser surgery. | ||
| Tissue engineering. |
Table 6: Examples of surgical treatments.
Supportive therapy
This therapy is suggested for prevention of recurrence of disease and also sustenance of periodontal health [43]. This therapy includes regular check-ups of the patient, to monitor the periodontal status and to re-educate to the patient regarding plaque control measures and oral hygiene maintenance [44].
Management: Periodontal disease has capacity to control the progression of disease and inhibit the growth of microorganisms. However, the success of therapy for periodontal disease depends upon appropriate management with proper treatments [45]. The management of periodontal disease consists of removal of supra-gingival and sub-gingival dental plaque followed by healing in tooth loss [46]. In general, it takes around 3 months of treatment interval to control the chronicity of periodontal disease. Maintenance period has been customized depends upon severity of disease. Supportive therapy aims long term maintenance of disease, so proper measures are taken to improve the compliances of management by patients to control the disease progression [47]. Management plan for periodontal disease includes following steps (Figure 8):
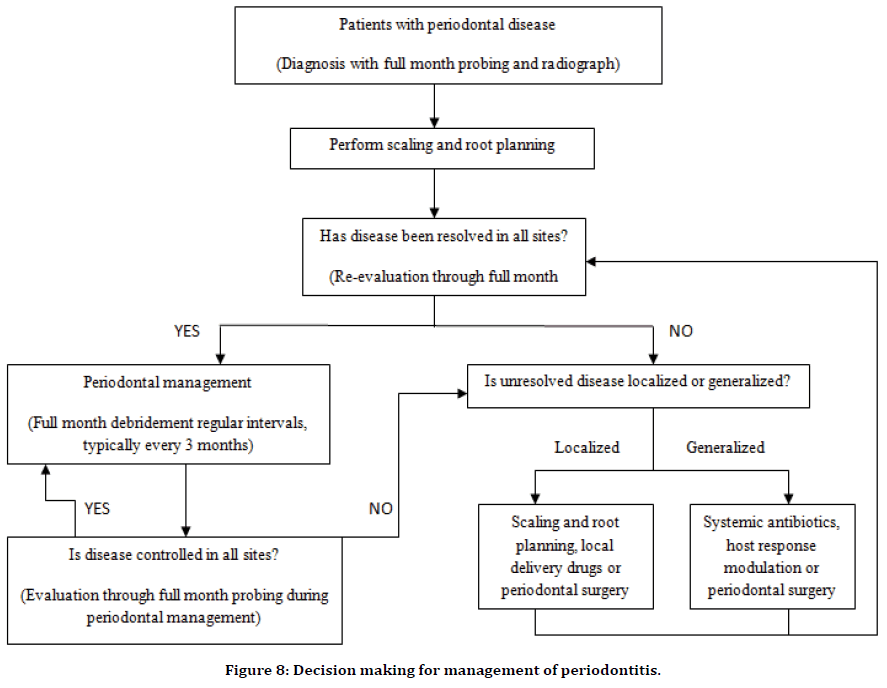
Figure 8. Decision making for management of periodontitis.
Conflict of Interest
None.
References
- Preshaw PM, Bissett SM. Periodontitis: Oral complication of disease. Endocrinol Metabolism Clin North Am 2013; 15:1-9.
- Chapple ILC, Mealey BL, Van Dyke TE, et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J Clin Periodontol 2018; 7:34-41.
- Murakami S, Mealey BL, Mariotti A, et al. Dental plaque–induced gingival conditions. J Clin Periodontol 2018; 42:8-20.
- Darveau RP, Tanner A, Page RC. The microbial challenge in periodontitis. J Periodontol 1997; 4:107-119.
- Alvares OF, Martins SK. Periodontal diseases: An updated review. J Nutritional Aspects Aging 2018; 2:21-28.
- Flemmig TF. Periodontitis: A chronic condition. In: Annals of periodontology/the American Academy of Periodontology 1999; 6:121-129.
- Savage A, Eaton KA, Moles DR, et al. A systematic review of definitions of periodontitis and methods that have been used to identify this disease. J Clin Periodontol 2009; 18:64-72.
- Papapanou PN, Sanz M, Buduneli N, et al. Periodontitis: Consensus report of workgroup 2 of the 2017 world workshop on the classification of periodontal disease and peri-implant diseases and conditions. J Clin Periodontol 2018; 16:30-41.
- Sekino S, Mantyla P. A report: Clinical periodontology. J Academy Clin Dent 2011; 10:116-128.
- Abbott P V, Karring T. Classification, diagnosis, and clinical manifestations of periodontitis. Endodontist Topic J 2004; 4:3-17.
- Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Periodontol 2018; 42:139-144.
- Niemiec BA, Baylin S, Axelsson D, et al. Periodontal disease: Chronological study. Top Companion Dent Med J 2008; 24:354-368.
- Loftus JJ, Keating AP, McCartan BE. Periapical status and quality of endodontic treatment in an adult Irish population. Int Endonot J 2005; 14:874-879.
- Susin C, Haas AN, Albandar JM. Epidemiology and demographics of aggressive periodontitis. Periodontolol 2014; 19:290-296.
- Petersen PE, Ogawa H. The global burden of periodontal disease: Towards integration with chronic disease prevention and control. Periodontol 2012; 17:93-102.
- Eke PI, Dye BA, Wei L, et al. Prevalence of periodontitis in adults in the united states: 2009 and 2010. J Dent Res 2012; 18:182-189.
- Slots J, Breininger D, Scapoli C. Periodontitis: Facts, fallacies and the future. Periodontol 2017; 22:9-21.
- Genco RJ, Borgnakke WS. Risk factors for periodontal disease. Periodontol 2013; 18:460-472.
- Shizukuishi S. Smoking and periodontal disease. Clin Calcium J 2007; 10:155-160.
- Taylor GW, Borgnakke WS. Periodontal disease: Associations with diabetes, glycemic control, and complications. Oral Diseases 2008; 05:601-608.
- Zee KY, Giannobe WK, Stambaugh JS, et al. Smoking and periodontal disease. Australia Dent J 2009; 13:205-211.
- Dye BA, Caton J, Chang K, et al. Global periodontal disease epidemiology. Periodontol 2012; 17:167-178.
- Berglundh T, Donati M. Aspects of adaptive host response in periodontitis. J Clin Periodontol 2005; 15:79-95.
- Kinane DF, Mombelli A. Review on periodontal disease. J Periodont Disease 2011; 15:124-132.
- Listgarten MA, Becker WK, Rios HM. Pathogenesis of periodontitis. J Clin Periodontol 1986; 5:129-138.
- Costalonga M, Herzberg MC. The oral microbiome and the immunobiology of periodontal disease and caries. J Immunological Letter 2014; 35:C673-C679.
- Lang NP, Bartold PM. Periodontal health review. J Clin Periodontol 2018; 22:590-596.
- Williams RC. Periodontal disease: Detail on screening and examination. New England J Med 1990; 3:235-244..
- Oh TJ, Eber R, Wang HL. Periodontal diseases in the child and adolescent. J Clin Periodontol 2002; 12:125-137.
- Highfield J, Brooke M, Wilson T. Diagnosis and classification of periodontal disease. Australian Dent J 2009; 18:505-509.
- Fine DH, Patil AG, Loos BG. Classification and diagnosis of aggressive periodontitis. J Clin Periodontol 2018; 22:77-104.
- Laine ML, Crielaard W, Loos BG. Genetic susceptibility to periodontitis and detail of treatment process. Periodontol 2012; 17:103-108.
- Chapple ILC, Van Der Weijden F, Doerfer C, et al. Primary prevention of periodontitis: Managing gingivitis. J Clin Periodontol 2015; 19:21-28.
- Hine MK. The use of the toothbrush in the treatment of periodontitis. J Med Dent Association 2007; 6:107-119.
- Erbe C, Klees V, Braunbeck F, et al. Comparative assessment of plaque removal and motivation between a manual toothbrush and an interactive power toothbrush in adolescents with fixed orthodontic appliances: A single-center, examiner-blind randomized controlled trial. J Orthodont Dentofacial Orthop 2019; 38:115-119.
- Efstratiou M, Papaioannou W, Nakou M, et al. Use of adjunctive pharmacological aids in a toothbrush with antibacterial properties by oral microorganisms. J Dent 2007; 14:2-12.
- Sanz I, Alonso B, Carasol M, et al. Nonsurgical treatment of periodontitis. J Evidence Based Dent Practices 2012; 20:59-68.
- Cleland WP, Demmer RZ. Nonsurgical periodontal therapy. Clin Technol Small Animal Practice 2000; 8:222-229.
- Friedman S, Abitbol S, Lawrence HP. Treatment outcome in endodontics: The Toronto study. Phase 1: Initial treatment. J Endodont 2003; 11:379-384.
- Jain N, Jain GK, Javed S, et al. Recent approaches for the treatment and management of periodontitis. Drug Discovery Today 2008; 23:194-202.
- Cobb CM. Lasers and the other surgical treatment of periodontitis: The essence and the noise. Periodontol 2017; 16:32-38.
- Nowzari H, Teumer A. Aesthetic osseous surgery in the treatment of periodontitis. Periodontol 2001; 9:174-185.
- Rohlin M, Susanna A, Ekman A, et al. Chronic periodontitis-Prevention, diagnosis, and treatment-A systematic review. Systematic Review Summaries 2004; 19:e211-e219.
- Durham J, Fraser HM, McCracken GI, et al. Impact of periodontitis on oral health-related quality of life. J Dent 2013; 23:507-511.
- Van Dyke TE, Cassier M, Lalla A. The management of inflammation in periodontal disease. J Periodontol 2008; 7:93-100.
- Farzaneh M, Abitbol S, Friedman S. Treatment outcome in periodontitis: The management of study. Phases I and II: Orthograde retreatment. J Endodont 2004; 12:119-126.
- Siqueira JF, Rôças IN, Ricucci D, et al. Causes and management of post-treatment periodontitis in patients. Br Dent J 2014; 6:S49-S56.
Author Info
Pragati S Dubey* and Neelam Mittal
Faculty of Dental Sciences, Institute of Medical Sciences, Banaras Hindu University, IndiaCitation: Pragati S Dubey, Neelam Mittal, A Systematic Review on Periodontal Disease, J Res Med Dent Sci, 2020, 8 (6): 153-162.
Received: 06-Aug-2020 Accepted: 21-Sep-2020
