Research - (2022) Volume 10, Issue 11
Accuracy of Postpartum Blood Loss Estimation and Its Correlation with Postpartum Drop in Hemoglobin
Amal Abdullah AlManei, Munirah Abdulrahman AlTuraiyef* and Shayma Abdrabalnabi Alsalman
*Correspondence: Munirah Abdulrahman AlTuraiyef, Department of Obstetrics and Gynecology, Saudi Board, Imam Abdulrahman bin Fisal Hospital, National Guard Health Affair, Dammam, KSA, Email:
Abstract
Background: Postpartum hemorrhage (PPH) is a serious obstetric complication, and real-time blood loss assessment is critical for PPH diagnosis and therapy. For assessing postpartum blood loss in a vaginal birth, measured the pre-delivery and post-delivery blood hemoglobin and hematocrit. The goal of this study was to determine the accuracy of estimated blood loss compared to a postpartum drop of hemoglobin and hematocrit. Methods: The current study is a correlational cross-sectional study, which is an observational study that analyzes data from a population at a specific point in time. This study was conducted over eight months for term pregnant women who had vaginal delivery in Imam Abdulrahman Al-Faisal Hospital National Guard in Dammam from January 2021. The hospital provides medical care to National Guard employees and their dependents. In addition to other Saudi citizens that need tertiary care. Results: The study included 344 women as a study sample. The mean age of women included in this study was 29.19 ± 5.99 years with a median age of 28 years. The age ranged from 15 to 51 years. The median value of parity among study women was two. Parity ranged from primigravida to eleven. The mean weight among study participants was 76.66 ± 14.69 kg with a median weight of 75 kg. The weight ranged from 45 to 132 kg among study participants. On the other hand, the mean height was 156.56 ± 5.66 cm with the median height of 157 cm. The mean body mass index (BMI) among study participants was 31.32 ± 5.80 with a median BMI of 30.48. The pre-delivery mean value of hemoglobin was 11.27 ± 1.17 g/dl with a median value of 11.3 g/dl while the mean value of pre-delivery hematocrit was 0.352 ± 0.036 with median value of 0.354. Conclusion: Our findings imply that the PPH criteria of less than 500 mL blood loss are unrelated to PPH-related morbidity as determined by hemoglobin drop and postpartum anemia. These data cast doubt on the usefulness of this threshold as a study endpoint for evaluating the efficacy of PPH treatments.
Keywords
Obstetrics, Gynecology, Postpartum hemorrhage, World Health Organization
Introduction
All women will lose blood in the early postpartum period, but excessive blood loss (i.e., postpartum hemorrhage [PPH]) can be catastrophic and the leading cause of maternal death worldwide [1]. The definition of severe blood loss remains controversial. The most commonly cited definition is that of the World Health Organization (WHO), which defines PPH as blood loss of 500 mL within 24 hours after vaginal delivery and 1000 mL after cesarean delivery [2,3]. During the 1950s and 1960s, several studies [4-7] established the 500 mL standard and developed a consensus on the concept. However, there is little evidence that this threshold is a predictor of PPH-related morbidity [8], and evidence from studies treating women with higher bleeding thresholds (eg, 700 mL) suggests that many women who bleed 500 mL without intervention may be healthy [9,10].
PPH is now defined by the American College of Obstetricians and Gynecologists (ACOG) as "blood loss greater than or equal to 1000 mL or blood loss with signs or symptoms of hypovolemia" [11]. Nonetheless, the term 500mL is still used as a guideline for clinical practice recommendations, program evaluation methods, and research programs in many parts of the world. The physiological effects of labor and postpartum blood loss can be measured using postpartum hemoglobin alone or by comparison with prepartum levels. Changes in perinatal hemoglobin and postnatal blood loss are thought to be significantly associated; however, some studies have found a weak association [12-14]. Recent studies have found that the two are closely related only when postpartum blood loss exceeds 1500 mL [15,16], suggesting that the specific quantity of blood loss below this threshold may have only a little influence on a woman's physiological well-being following delivery.
Women with mild problems can tolerate small blood loss (500-1000 mL), so the 500 mL threshold may be a poor predictor of a negative outcome [17]. These effects are particularly important for maternal health research, as precise postpartum blood loss and 500 mL PPH thresholds are routinely used endpoints, although they have no clinical value. Postpartum anemia can be caused by clinically significant blood loss during childbirth, which negatively affects the health of the mother and child in the postpartum period [18-20]. Examining the relationship between blood loss and blood loss-based definitions of PPH and postpartum hemoglobin results can help clarify this issue.
To better understand how well postpartum blood loss and common postpartum hemorrhage (PPH) definitions (i.e. blood loss ≥500 ml=PPH, ≥1000 ml=“severe” PPH) correlate with postpartum anemia and fall in hemoglobin, we conducted this study. The current study aimed to compare the efficacy of quantitative measurement using the sterile under drape and weighing compared to the laboratory drop of hemoglobin and hematocrit post vaginal delivery. Moreover, to determine the accuracy of estimated blood loss compared to a postpartum drop of hemoglobin and hematocrit and to determine whether the calculation of maximum allowable blood loss will help in the early detection of the patient at risk of significant blood loss.
Methods
Study design
The current study is a correlational cross-sectional study which is an observational study that analyzes data from a population at a specific point in time.
Study settings
This study was conducted over eight months for term pregnant women who had vaginal delivery in Imam Abdulrahman Al-Faisal Hospital National Guard in Dammam from January 2021. The hospital provides medical care to National Guard employees and their dependents. In addition to other Saudi citizens that need tertiary care.
Sample size
About Imam Abdulrahman Al-Faisal Hospital National Guard in Dammam hospital delivery rate in the last three years, the average rate of vaginal delivery has been 50 vaginal delivery per month. We have used this effect size to calculate the optimal sample size for our study. Applying the categorical sample size formula. The number of patients required detecting a statistical result with a 95% level of confidence and 2% margin of error should be 343 patients.
Participants
Term pregnant women who had vaginal delivery in NGHA, Dammam from January 2021 over eight months.
Eligibility criteria
The study will include all singleton pregnant women, 37 weeks gestational age or more (based on early first-trimester ultrasonography and/or LMP), who had a vaginal delivery either, spontaneous or operative vaginal deliveries. Taking into consideration patients' comorbidities and risk factors that might contribute to increasing the rate of postpartum hemorrhage including gestational diabetes mellitus, diabetes mellitus, previous cesarean section, obesity, induction of labor, and preexisting anemia and whether it was treated or not in the antenatal period.
We excluded all cases of severe postpartum hemorrhage that were managed urgently with blood transfusion. Also, cases of multiple pregnancies, preterm deliveries, and medical history of hematological disorders, preeclampsia, intrauterine fetal death, and active infection (e,g: Chorioamnionitis, COVID-19).
Data collection instruments
All data of patients who meet the inclusion criteria were collected using Excel. All those patients were managed according to our standard admission protocol including blood investigations of CBC (complete blood count), Coagulation profile, and type & screen.
The maximum allowable blood loss will be calculated using this equation: EBV calculation: body weight (kg) x average blood volume (ml/kg) MABL=[EBV x (Hi-Hf)]/Hi
Where:
EBV=Estimated Blood Volume ( 65 ml/kg in adult female) MABL=Maximum Allowable Blood Loss
Hi=initial hemoglobin or hematocrit
Hf=final hemoglobin or hematocrit (Lowest acceptable by clinical judgment 8.5 g/dl)
For a more validated and accurate method of calculating Maximum Allowable Blood Loss in pregnant women, the maternal blood volume is calculated using the maternal height and weight using the formula.
cBV=(0.75 ([maternal height (inches) X 50]± [maternal weight in pounds X 25]) MABL=[cBV x (Hi-Hf)]/Hi
Where:
cBV=Calculated Blood Volume Hi=initial hemoglobin or hematocrit
Hf=final hemoglobin or hematocrit (Lowest acceptable by clinical judgment 8.5 g/dl) During delivery a sterile under-buttock drape was used during all deliveries. And immediately after delivery followed the Active management of the Third stage of labor protocol of 5 units of intramuscular injection of oxytocin and 20 units of oxytocin in 1,000 mL normal saline that was delivered intravenously at 125 mL/hr, combined with an intramuscular injection of Methylergometrine 0.2 mg if not contraindicated as standard medical prevention of immediate PPH.
Subsequently, after the delivery, the blood from the under-buttock drape and all gauzes are measured by a qualified nurse and midwife and the total blood loss was calculated. Patients with immediate PPH underwent care based on the standard protocol for the management of immediate PPH.
Complete blood count was repeated for all patients twelve to twenty-four hours postpartum to check if there is Hemoglobin and hematocrit drop and managed patient accordingly, the patient who developed hypovolemia signs and symptoms in the early postpartum period who underwent care and management immediately were excluded.
Data analysis
Data obtained from medical records were entered and analyzed using SPSS program version 23 computer software. Sociodemographic data are presented using descriptive statistics as means, median, percentages, and standard deviation. Independent T-test and one-way ANOVA are used to show statistical significance among patients’ characteristics and tool scores. The Chi-square test is used to show the relationship between categorical variables.
Ethical consideration
Privacy and confidentiality were completely protected. No personal information was collected or stored including the patient's name, national ID numbers, and other.
Results
The study included 344 women as a study sample. The mean age of women included in this study was 29.19 ± 5.99 years with a median age of 28 years. The age ranged from 15 to 51 years. The median value of parity among study women was two. Parity ranged from primigravida to eleven. Some women in this study underwent induction of labor (n=84, 24.4%). There were some women included in this study who suffered from certain conditions which are presented in (Table 1).
| Comorbid condition | Frequency | Percentage |
|---|---|---|
| Gestational Diabetes Mellitus | 65 | 18.9 |
| Diabetes Mellitus | 3 | 0.9 |
| Previous Caesarian Section | 27 | 7.8 |
| Anemia | 147 | 24.7 |
Table 1: Comorbid conditions of women included in the study.
As presented in (Table 1), 147 women suffered from anemia and thus antenatal ferrous injection was performed among 71 women only (20.6%). The mean weight among study participants was 76.66 ± 14.69 kg with a median weight of 75 kg. The weight ranged from 45 to 132 kg among study participants. On the other hand, the mean height was 156.56 ± 5.66 cm with a median height of 157 cm. The mean body mass index (BMI) among study participants was 31.32 ± 5.80 with a median BMI of 30.48. The delivery mood varied among study participants, however, most of the study participants gave birth through spontaneous vaginal delivery (Figure 1).
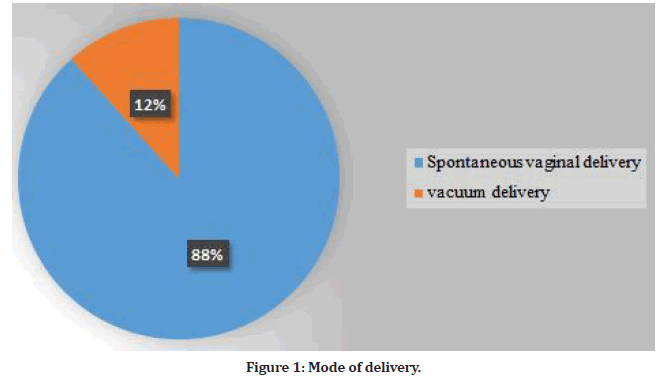
Figure 1: Mode of delivery.
The pre-delivery mean value of hemoglobin was 11.27 ± 1.17 g/dl with a median value of 11.3 g/dl while the mean value of pre-delivery hematocrit was 0.352 ± 0.036 with a median value of 0.354. The quantitative blood loss mean value was 365.64 ± 234.67 ccs with a median value of 309 cc. This is reflected by the mean post-delivery hemoglobin level mean value of 10.27 ± 1.37 g/dl with a median value of 10.4 g/dl. This reflects a mean loss of 1 g/ dl of hemoglobin among study participants. On the other hand, the mean value of post-delivery hematocrit was 0.319 ± 0.042% with median post-delivery hematocrit of 0.323%. The mean value of estimated blood volume is 4900 ± 955 cc with median value of 4875 (Table 2A and Table 2B).
| Pre-delivery Hg | Pre-delivery Hct | EBL | Post- delivery Hg | Post- delivery Hct | EBV | |
|---|---|---|---|---|---|---|
| Mean | 11.27791 | 0.35299 | 365.6 | 10.27994 | 0.31967 | 4990.0 651 |
| Median | 11.3 | 0.354 | 309 | 10.4 | 0.323 | 4875.0 000 |
| Mode | 11.1 | 0.349 | 300 | 10.4 | 0.295a | 4680.0 0 |
| Std. Deviation | 1.174302 | 0.036112 | 234.6 | 1.374159 | 0.042481 | 955.07 671 |
| Minimum | 8.1 | 0.251 | 50 | 6.2 | 0.198 | 2944.5 0 |
| Maximum | 15.1 | 0.456 | 1540 | 14 | 0.418 | 8580.0 0 |
Table 2A: Pre-delivery and post-delivery measurements of study participants.
| MABEL | cBV | cEBL_Hg | cEBL_Hct | |
|---|---|---|---|---|
| Mean | 1194.19472 | 19133.10157 | 437.30159 | 465.07572 |
| Median | 1196.21045 | 19105.12829 | 394.06957 | 424.17273 |
| Mode | 1233.243 | 18776.663 | 0 | 0 |
| Std. Deviation | 485.065032 | 1085.000862 | 441.794419 | 459.057659 |
| Minimum | -170.123 | 16298.867 | -825.991 | -533.872 |
| Maximum | 2662.4 | 22695.282 | 1867.039 | 2049.924 |
Table 2B:Pre-delivery and post-delivery measurements of study participants.
However, this drop in hemoglobin was not statistically significant between pre-delivery measurements and post-delivery measurements. Table 3 shows the statistical relationship between the two methods of estimating postpartum blood. As mentioned in Table 1, some participants had the comorbid condition. However, it was not found that any of the comorbid conditions and risk factors had a statistically significant relationship with blood loss using two assessment methods (Table 4).
| EBL | Blood loss according to drop in hemoglobin | Accuracy (%) | Underestimation (%) | |||||
|---|---|---|---|---|---|---|---|---|
| 0-100 | 101-200 | 201-300 | 301-400 | 401-500 | More than 500 | |||
| 0-100 | 0 | 0 | 0 | 0 | 0 | 2 | 77.8 | 0 |
| 101-200 | 0 | 1 | 2 | 0 | 0 | 67 | 33.7 | 64.4 |
| 201-300 | 0 | 2 | 2 | 2 | 2 | 85 | 11.8 | 86.8 |
| 301-400 | 0 | 0 | 0 | 5 | 2 | 60 | 11.6 | 86 |
| 401-500 | 1 | 0 | 1 | 0 | 1 | 69 | 0 | 100 |
| More than 500 | 0 | 0 | 1 | 1 | 0 | 34 | 34.6 | 65.4 |
Table 3: Comparative analysis between two methods of estimating postpartum blood loss.
The maximum allowable blood loss mean value among study participants was 1194.19 ± 485.06 cc with a median value of 1196.21 ccs. The calculated blood volume means the value was 19133 ± 1085 with a median value of 19105 (Table 4). The postpartum treatment among most of the women included in this study was iron tablets (n=313, 91%). Other treatments were Ferrous injection (Ferrinject) which was used for 8% of those patients, while blood transfusion was only required for 1% of total cases included in this study as demonstrated in (Figure 2).
| Comorbid Condition & Risk Factors | P-value | |
|---|---|---|
| Quantitative method | Laboratory method | |
| Gestational Diabetes Mellitus | 0.08 | 0.12 |
| Diabetes Mellitus | 0.16 | 0.08 |
| Previous Caesarian Section | 0.33 | 0.07 |
| Anemia | 0.05 | 0.05 |
| Induction of Labor | 0.05 | 0.09 |
| BMI >30 | 0.06 | 0.06 |
Table 4: Statistical relationship between comorbid condition and risk factors in estimation of blood loss using two methods.
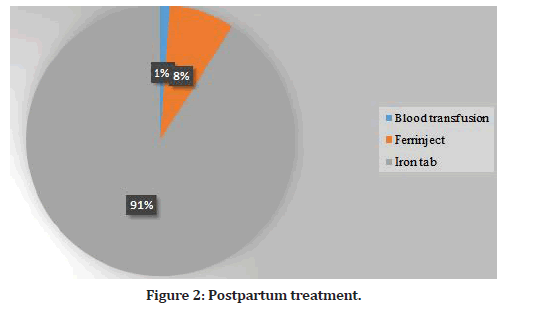
Figure 2: Postpartum treatment.
Discussion
Overall, our statistics suggest that the correct amount of blood loss has little effect on determining a woman's postpartum status. This localization is large, as it applies to both a networked setting with few treatments and a nursing home setting with a variety of procedures in 5 countries, as well as intravenous fluid management. To explain why the correlation between blood loss and hemoglobin measurements became so fragile in these obstetric groups, authors of other studies with similar implications suggested that even blood loss was above average (500–1200 ml). This may be related to the general increase in plasma levels throughout pregnancy, which is thought to serve as a protective model for predicted massive blood loss after birth [20-27].
The terms "postpartum blood loss" and "prenatal to postnatal hemoglobin change" are sometimes used interchangeably, on the basis that blood loss estimation can help to determine the hemoglobin changes and the other way around.
Crucially, our statistics confirm that the 500mL threshold for PPH is less significant when comparing PPH results with blood loss of up to 900-1100 ml, there may be a significant clinical drop in hemoglobin of 2 g/dl. In addition, among women with blood loss greater than 500 mL but less than 1000 mL, 31-42% had a hemoglobin drop of less than 2 g/dL, and 31-54% had postpartum hemoglobin levels below the threshold for mild anemia. Notably, 1-3% of women with blood loss of 500-999 mL had postpartum hemoglobin ranges beneath the "severe" anemia threshold, which necessitates blood transfusion [28,29].
The findings of the current study propose that the five hundred ml threshold (which represents almost 10% of a full-term pregnant woman's general blood volume) won't be a dependable predictor of a terrible outcome, as many women can tolerate this degree of blood loss without complications, though this could range relying upon the presence of anemia or different underlying medical conditions [17]. The 1000 ml threshold appears to be more crucial in terms of definitions of PPH, as this is when clinically significant reductions in hemoglobin occurred more frequently and the majority of women had postpartum hemoglobin values below the marker of moderate anemia. It's important to remember that our research focused on the endpoint of blood loss, and it's impossible to know whether a blood loss of more than 500 ml indicates the end of bleeding (in which case minimal intervention is likely) or an earlier point in the course of bleeding (in which case more rigorous intervention is likely necessary). In this light, we feel our findings back up a 1996 WHO guideline that the 500ml mark "should be seen as a warning line; the action line is reached when the woman's vital functions are jeopardized."
This happens only after a blood loss of greater than 1000ml in healthy women" [30]. The findings back up ACOG recommendations that "blood loss of 500–999 ml alone should merit heightened surveillance...", however, PPH criteria aren't reached until blood loss surpasses 1000 ml [11]. In remote places with limited access to emergency obstetric care, 500ml may be a suitable threshold for giving first-line treatment such as uterotonics.
Our results support the idea that future PPH classifications should take into account factors other than blood loss [8]. Difficulties in estimating blood loss are well documented [22,31] and the exact amount of blood loss in most deliveries is uncertain. Close monitoring of a woman's general health after delivery, including regular vital sign measurements, is essential but rarely done in busy, resource-constrained settings. In this regard, studies are underway to better understand the importance of the shock index (ratio of systolic blood pressure to pulse rate) as a secondary indicator of PPH [32-35]. This study has many shortcomings. It included secondary analysis of data from three studies that were not aimed at this. On the other hand, these studies attempted to systematically track blood loss and hemoglobin before and after birth.
Methods of objectively determining blood loss and timing of hemoglobin testing before and after delivery changed during the study period. However, previous studies [36-39] showed that the blood loss measures used in all three studies were valid and accurate, especially when compared to visual blood loss assessments. In addition, hemoglobin levels before and after delivery were calculated and showed slightly higher readings than automated laboratory methods; this may lead to some underestimation of postpartum hemoglobin and postpartum anemia rates, but should not affect our analysis of hemoglobin decline [38, 39]. Nonetheless, the fact that we showed similar effects in various delivery settings (community and hospital) strengthens our conclusions and expands the applicability of our results.
Conclusion
Our findings imply that the PPH criteria of less than 500 mL blood loss are unrelated to PPH-related morbidity as determined by hemoglobin drop and postpartum anemia. These data cast doubt on the usefulness of this threshold as a study endpoint for evaluating the efficacy of PPH treatments. Additional research, including metaanalyses, might shed more light on the link between postpartum blood loss and hemoglobin results. Our findings imply that future PPH intervention trials should place less emphasis on endpoints like 500 mL and instead focus on more significant outcomes like severe PPH of blood loss of more than 1000 mL. This method might help researchers identify therapies that are most likely to reduce maternal death and morbidity.
References
- Say L, Chou D, Gemmill A, et al. Global causes of maternal death: A WHO systematic analysis. Lancet Glob Health 2014; 2:e323–e333.
- https://apps.who.int/iris/bitstream/handle/10665/75411/9789241548502_eng.pdf
- Arulkumaran S, Mavrides E, Penney GC. Prevention and management of postpartum haemorrhage guideline. London, UK: Royal College of Obstetricians and Gynaecologists 2009.
- De Boer CN. The aetiology of post-partum haemorrhage. Br Med J 1955; 2:1187.
- Newton M, Mosey LM, Egli GE, et al. Blood loss during and immediately after delivery. Obstet Gynecol 1961;17:9–18.
- Pritchard JA. Changes in the blood volume during pregnancy and delivery. Anesthesiology 1965; 26:393–399.
- Theobald GW. Post-partum haemorrhage. Br Med J 1950; 1:659–661.
- Kerr RS, Weeks AD. Postpartum haemorrhage: A single definition is no longer enough. BJOG 2017; 124:723–726.
- Blum J, Winikoff B, Raghavan S, et al. Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women receiving prophylactic oxytocin: A double-blind, randomised, non-inferiority trial. Lancet 2010; 375:217–223.
- Winikoff B, Dabash R, Durocher J, et al. Treatment of post-partum haemorrhage with sublingual misoprostol versus oxytocin in women not exposed to oxytocin during labour: A double-blind, randomised, non-inferiority trial. Lancet 2010; 375:210–216.
- Menard MK, Main EK, Currigan SM. Executive summary of the reVITALize initiative: Standardizing obstetric data definitions. Obstet Gynecol 2014; 124:150–153.
- Palm C, Rydhstroem H. Association of blood loss during delivery to B- hemoglobin. Gynecol Obstet Invest 1997; 44:163–168.
- Larsson A, Saltvedt S, Wiklund I, et al. Estimation of blood loss after cesarean section and vaginal delivery has low validity with a tendency to exaggeration. Acta Obstet Gynecol Scand 2006; 85:1448–1452.
- Girault A, Deneux-Tharaux C, Sentilhes L, et al. Undiagnosed abnormal postpartum blood loss: Incidence and risk factors. PLoS One 2018; 13:e0190845.
- Conner SN, Tuuli MG, Colvin R, et al. Accuracy of estimated blood loss in predicting need for transfusion after delivery. Am J Perinatol 2015; 32:1225–1230.
- Lilley G, Burkett-st-Laurent D, Precious E, et al. Measurement of blood loss during postpartum haemorrhage. Int J Obstet Anesth 2015; 24:8–14.
- Coker A, Oliver R. Definitions and classifications In: B Lynch C, Keith L, Lalonde A, et al. A Textbook of postpartum hemorrhage. United Kingdom: Sapiens Publishing 2006; 11–16.
- Beard JL, Hendricks MK, Perez EM, et al. Maternal iron deficiency anemia affects postpartum emotions and cognition. J Nutr 2005; 135:267–272.
- Corwin EJ, Murray-Kolb LE, Beard JL. Low hemoglobin level is a risk factor for postpartum depression. J Nutr 2003; 133:4139–4142.
- Perez EM, Hendricks MK, Beard JL, et al. Mother-infant interactions and infant development are altered by maternal iron deficiency anemia. J Nutr 2005; 135:850–855.
- Mobeen N, Durocher J, Zuberi NF, et al. Administration of misoprostol by trained traditional birth attendants to prevent postpartum haemorrhage in homebirths in Pakistan: A randomised placebo‐controlled trial. BJOG: Int J Obstetr Gynaecol 2011; 118:353-361.
- Kodkany BS. Pitfalls in assessing blood loss and decision to transfer In: Arulkumaran SKM, Keith LG, Lalonde AB, et al. A comprehensive textbook of postpartum hemorrhage: An essential reference for effective management. 2nd Ed London: Sapiens Publishing Ltd 2012; 81–88.
- http://www.who.int/vmnis/indicators/haemoglobin.pdf
- Hinkle DE, Wiersma W, Jurs SG. Applied statistics for the behavioral sciences 5th Ed. Boston: Houghton Mifflin 2003; 756.
- Jansen AJ, leNoble PJ, Steegers EA, et al. Relationship between haemoglobin change and estimated blood loss after delivery. BJOG 2007; 114:657.
- Atukunda EC, Mugyenyi GR, Obua C, et al. Measuring post-partum haemorrhage in low-resource settings: The diagnostic validity of weighed blood loss versus quantitative changes in hemoglobin. PLoS One 2016; 11:e0152408.
- Whittaker PG, Macphail S, Lind T. Serial hematologic changes and pregnancy outcome. Obstet Gynecol 1996; 88:33–39.
- WHO, UNFPA, UNICEF. Managing complications in pregnancy and childbirth: A guide for midwives and doctors 2nd ed Geneva: World Health Organization 2017.
- McLintock C, James AH. Obstetric hemorrhage. J Thromb Haemost 2011; 9:1441–1451.
- Technical Working Group, World Health Organization. Care in normal birth: A practical guide. Birth 1997; 24:121-123.
- Hancock A, Weeks AD, Lavender DT. Is accurate and reliable blood loss estimation the 'crucial step' in early detection of postpartum haemorrhage: an integrative review of the literature. BMC Pregnancy Childbirth 2015; 15:230.
- Pacagnella RC, Souza JP, Durocher J, et al. A systematic review of the relationship between blood loss and clinical signs. PLoS One 2013; 8:e57594.
- Le Bas A, Chandraharan E, Addei A, et al. Use of the "obstetric shock index" as an adjunct in identifying significant blood loss in patients with massive postpartum hemorrhage. Int J Gynaecol Obstet 2014; 124:153–155.
- Nathan H, El Ayadi A, Hezelgrave N, et al. Shock index: An effective predictor of outcome in postpartum haemorrhage? BJOG 2015; 122:268–275.
- El Ayadi AM, Nathan HL, Seed PT, et al. Vital sign prediction of adverse maternal outcomes in women with hypovolemic shock: The role of shock index. PLoS One 2016; 11:e0148729.
- Gulmezoglu AM, Villar J, Ngoc NT, et al. WHO Multicentre randomized trial of misoprostol in the management of the third stage of labour. Lancet 2001; 358:689–695.
- Patel A, Goudar SS, Geller SE, et al. Drape estimation vs. visual assessment for estimating postpartum hemorrhage. Int J Gynaecol Obstet 2006; 93:220–224.
- Sanchis-Gomar F, Cortell-Ballester J, Pareja-Galeano H, et al. Hemoglobin point-of-care testing: the HemoCue system. J Lab Autom 2013; 18:198–205.
- Daves M, Cemin R, Zagler EM, et al. Evaluation of capillary haemoglobin determination for anaemia screening in blood donation settings. Blood Transfus 2016; 14:387–390.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at , Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Amal Abdullah AlManei, Munirah Abdulrahman AlTuraiyef* and Shayma Abdrabalnabi Alsalman
Department of Obstetrics and Gynecology, Saudi Board, Imam Abdulrahman bin Fisal Hospital, National Guard Health Affair, Dammam, KSAReceived: 14-Oct-2022, Manuscript No. jrmds-22-79674; , Pre QC No. jrmds-22-79674(PQ); Editor assigned: 17-Oct-2022, Pre QC No. jrmds-22-79674(PQ); Reviewed: 02-Nov-2022, QC No. jrmds-22-79674(Q); Revised: 01-Nov-2022, Manuscript No. jrmds-22-79674(R); Published: 08-Nov-2022
