Research - (2020) Volume 8, Issue 3
An Analysis of Medication Errors in a Tertiary Care Teaching Hospital
Manasij Mitra1 and Maitraye Basu2*
*Correspondence: Maitraye Basu, Department of Biochemistry, MGM Medical College and LSK Hospital, Kishanganj, Bihar, India, Email:
Abstract
Introduction: Medication errors can occur at any step while handling a medication from prescribing, indenting, dispensing to administration. Medication errors have the potential to cause patient harm to the extent of serious morbidity or even mortality and can have a substantial cost impact on the healthcare system. It can also lead to patient dissatisfaction and loss of confidence on the medical care. This study done with the objective of analysis of medication errors in a teaching hospital with an aim towards process improvement is thus justified.
Materials and methods: This were a retrospective study done on the reported inpatient Medication Errors between January 2018 to December 2019 in a 600-bed tertiary care teaching hospital in Bihar. The total number of Medication errors reported during the study period was 1501 and the total number of orders during the said period was 28,472 as retrieved from the pharmacy software. The data from the Incident Report Form was entered in the Excel Spreadsheet and variables analysed using Descriptive Statistics.
Results: The medication error rate per 100 orders was 5.27. Majority of the Medication errors about 96.8% took place in the Wards. Majority of the Medication Errors i.e. 66.42% occurred between 4 PM to 8 PM. Doctors contributed to the maximum percentage of Medication Errors 69.8%. Majority of the medication errors 67.62% (1015) were a combination of prescription and transcription errors. The major reasons for Medication Errors were Dose related errors which constituted the maximum proportion of 70.43% (1058).
Conclusion: The study concluded that medication errors occur even in hospital settings with established policies for Safe Handling and Use of Medications. However, those can be restricted from reaching the patient with well-structured dedicated strategies and multi-level checks (“Swiss-cheese” Model) in place aimed towards increasing the safety of medication handling and use. Further in-depth studies are recommended on medication errors including “Near miss” which can throw more light on lapses in an existing process and identify the effective intervention strategies to help process improvement.
Keywords
Medication errors, Near miss, “Swiss-cheese” model, Safe medication practices
Introduction
The National Coordinating Council for Medication Error Reporting and Prevention (NCCMERP) defines Medication Error as "any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the health care professional, patient, or consumer. Such events may be related to professional practice, health care products, procedures, and systems, including prescribing, order communication, product labelling, packaging, and nomenclature, compounding, dispensing, distribution, administration, education, monitoring, and use" [1]. As per the American Society of Hospital Pharmacists, it is difficult to ascertain the incidence of Medication Errors due to diversity in the definitions of medication errors [2].
Though studies in hospitalised patients in India have reported ME rate ranging from 15.34% to 25.7%, however, unfortunately many medication errors remain undetected due to lack of structured reporting mechanisms until those cause patient harm [3,4].
Medication errors can occur at any step while handling a medication from prescribing, indenting, dispensing to administration. Medication errors have the potential to cause patient harm to the extent of serious morbidity or even mortality and can have a substantial cost impact on the healthcare system. It can also lead to patient dissatisfaction and loss of confidence on the medical care [5,6].
As per the Institute of Medicine costs due to medication errors in the US was approximately $37.6 billion/year with approximately $17 billion being preventable errors [7].
Some of the common reasons for medication errors cited by the American Hospital Association are incomplete patient or drug information, illegible prescription, therapeutic duplication, inappropriate abbreviations, miscommunications due to inappropriate use of metrics, decimals and zeroes and lack of appropriate labelling [8]. Medication errors in a hospital setting can be committed by any healthcare professional from the doctor to the pharmacist to the nursing staff [9].
When, we talk of Medication Errors, we should not be oblivious of the concept of “Near Miss.” The Institute for Safe Medication Practices defines a near miss as “any event or situation that didn't produce patient injury, but only because of chance” [10].
For the purpose of reporting, a “ near miss ” is a medication error like any other medication error that does not cause patient harm. Near misses are a rich source of information that can help building error prevention strategies [11,12].
This study done with the objective of analysis of medication errors in a teaching hospital with an aim towards process improvement is thus justified.
Materials and Methods
This study was conducted following approval of the Institutional Ethics Committee in MGM Medical College and LSK Hospital which is a 600 bed Multispecialty teaching hospital in Bihar.
This was a retrospective study done on the reported inpatient Medication Errors between January 2018 to December 2019. The total number of Medication errors reported through the mechanism of Incident Reporting as per hospital protocol during the study period was 1501 and the total number of orders during the said period was 28,472 as was retrieved from the pharmacy software. The data from the Incident Report Form was entered in the Excel Spreadsheet and variables analysed using Descriptive Statistics.
The hospital has a robust process of reporting any inpatient medication error. A pre-structured Incident Reporting Form is raised for any Category of Medication Error which comes to the Administration and Quality Control Department routed through the office of the Nursing Superintendent or Medical Superintendent of the hospital within 48 hours of occurrence. The Incident Reporting Form has a dedicated place for reporting the detailed incident which lead to the medication error, the categorization of the medication error as per the hospital policy and documentation of the immediate reason of the medication error as determined by the reporting department. As per the hospital policy any individual can raise the incident report. A detailed root cause analysis is done by the Department of Pharmacology and the Quality Assurance Department for every Medication Error Incident raised with three days of receipt of the incident with an aim towards corrective and preventive action. The incident report is used in its true spirit, purely for process improvement purposes and never for any punitive action.
As per the hospital policy and for the purpose of this study Medication errors have been categorised as follows [13].
Category A: No error, capacity to cause error.
Category B: Error that did not reach the patient.
Category C: Error that reached patient but unlikely to cause harm (omissions considered to reach patient).
Category D: Error that reached the patient and could have necessitated monitoring and/or intervention to preclude harm.
Category E: Error that could have caused temporary harm.
Category F: Error that could have caused temporary harm requiring initial or prolonged hospitalization.
Category G: Error that could have resulted in permanent harm.
Category H: Error that could have necessitated intervention to sustain life.
Category I: Error that could have resulted in death.
The hospital has a dedicated inpatient pharmacy which caters to the need of the admitted inpatients. The hospital has a robust mechanism to ensure Safe Medication Practices. Documented policies with easy access to all concerned staffs like doctors, pharmacists and nurses exist concerning selection and procurement of medications, storage, prescribing, transcribing, and indenting, dispensing, preparation and administration. The hospital separately identifies the High Alert Medications and Look Alike and Sound Alike Medications (LASA) and these medications are dispensed from the pharmacy with “ High Alert ” labels. Further there are specified policies to ensure safe handling and use of chemotherapeutic agents, High Alert Medications including drugs with Narrow Therapeutic Indices. Staffs are routinely trained on these policies as a part of the induction training and regular on-job training. The training process of the Nursing staffs is sound to cover not only the hospital policies and medication preparation and administration but also regular knowledge on drug dose calculations and basic knowledge of the drugs. The nursing training is imparted through regular classroom training sessions under the supervision of the Nursing Training Coordinator.
The hospital has a Formulary updated on a yearly basis with oversight from the Hospital Drug Committee. The Hospital Drug Committee reviews the Process of Handling and Storage of Medications to ensure Safe Medication Practices. The Committee meets at quarterly intervals to review the rate of Medication Errors and take necessary actions based on the root cause analysis of the reported medication errors. Physician Sample Medications and Self Medication by patients and medications brought by patients from outside pharmacy are not allowed as per hospital policy. Hard copy of Drug Dictionary to check drug name, dose, route, frequency, side effects are made available at every nursing station and updated on a yearly basis. The hospital has a process of double checking of high alert medications by the senior staff nurses before administration. The in-patient Medication use Process in the hospital is depicted below in Figure 1.
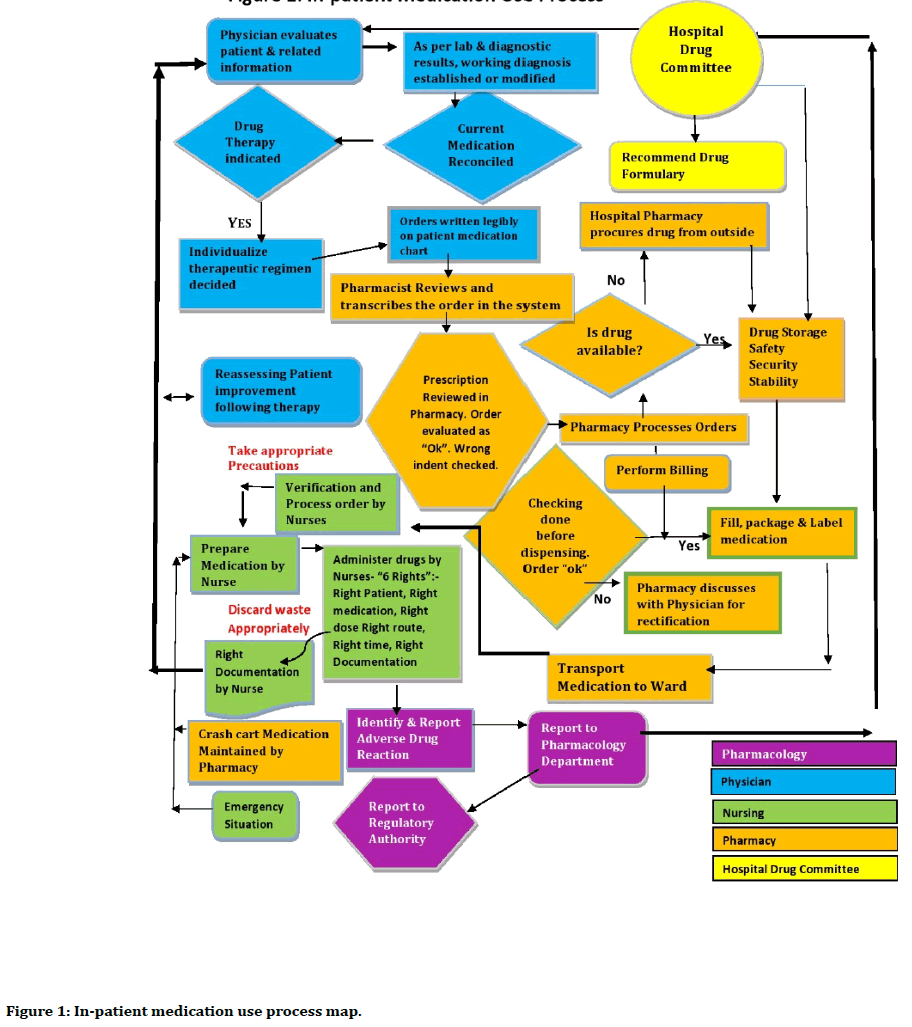
Figure 1. In-patient medication use process map.
Results
The total number of Medication Errors from January 2018 to December 2019 were 1501. The total number of orders during the study period was 28,472. So, the medication error rate per 100 orders was 5.27. Among the patients who had Medication Errors, 874 (58.23%) were male patients while 627 (41.77%) were female patients.
The average age of the study population was 57.31 years (Standard deviation ± 17.24). As depicted in Figure 2, 3.66% of the patients who had Medication Errors belonged to the Pediatric population in the age group upto 18 years, 57.5% belonged to the age group between 19-64 years and 38.84% belonged to the age group 65 years and above.
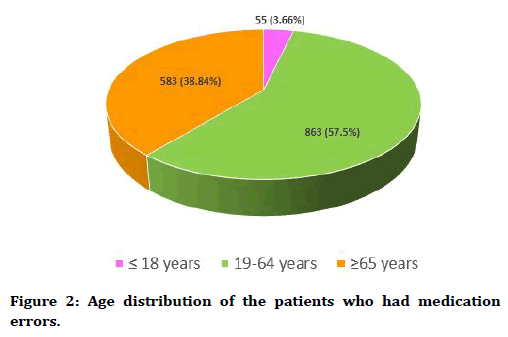
Figure 2. Age distribution of the patients who had medication errors.
Majority of the Medication errors about 96.8% took place in the Wards, while 2.53% of the Medication Errors occurred in the Critical Care units and a very small percentage 0.67% of the Medication Errors occurred in the Day Care unit as depicted in Figure 3.
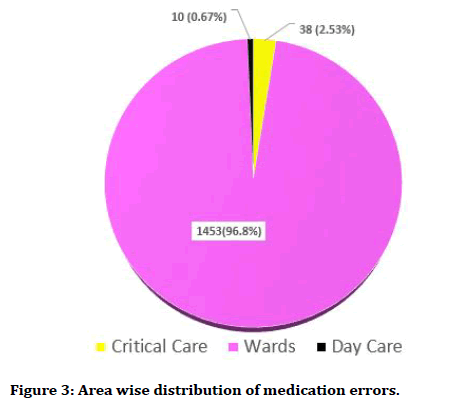
Figure 3. Area wise distribution of medication errors.
Time distribution of Medication Errors during the whole day revealed that 66.42% of the medication Errors occurred between 4 PM to 8 PM, followed by 12 noon to 4 PM which accounted for 16.79% of the Medication Errors while 12.41% Medication Errors occurred between 8 AM to 12 noon. A very small percentage 3.6% of the Medication Errors followed by 0.52% of the Medication Errors and 0.26% of the Medication Errors occurred between 8 PM to 12 midnight, 12 AM to 4 AM and 4 AM to 8 AM respectively.
As depicted in Figure 4, the Doctors contributed to the maximum percentage of Medication Errors 69.8%, the Pharmacists contributed to 25.04% of the Medication Errors while Nurses contributed to only 5.16% of the Medication Errors. 97.67% of the Medication errors were Category B errors while only 2.33% were Category C errors. No medication errors above Category C were reported. This has been depicted in Figure 5.
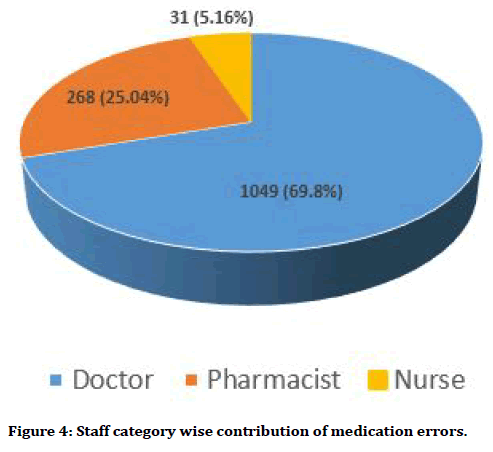
Figure 4. Staff category wise contribution of medication errors.
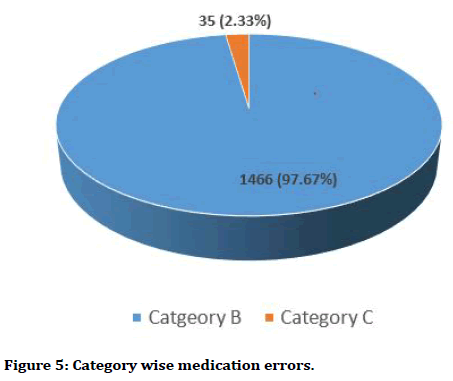
Figure 5. Category wise medication errors.
Medication Errors concerning Chemotherapeutic Medications constituted 1.59% of the Medication Errors, medication errors concerning High Alert Medications like concentrated electrolytes, heparin, Insulin, Narcotics constituted 1.67% medication errors. While other medications like antibiotics, vitamins, antihypertensive agents, Proton pump inhibitors constituted the remaining 96.74% of the medication errors. Fortunately, all the Medication Errors concerning chemotherapeutic agents or High Alert Medications were Category B errors.
Medication Errors Involving different stages in medication handling and usage have been depicted in Table 1. Majority 67.62% (1015) errors were a combination of prescription and transcription errors, followed by 17.52% (263) as only transcription errors, 10.33% (155) were a combination of transcription and dispensing errors, 2.26% (34) were purely prescription errors, 2.07% (31) were purely administration errors while 0.2% (3) errors were purely dispensing errors.
| Different stages in Medication Handling and Usage | Numbers | Percentage |
|---|---|---|
| Prescription | 34 | 2.26 |
| Transcription | 263 | 17.52 |
| Dispensing | 3 | 0.2 |
| Administration | 31 | 2.07 |
| Prescription and Transcription | 1015 | 67.62 |
| Transcription and Dispensing | 155 | 10.33 |
| Total | 1501 | 100 |
Table 1: Medication errors involving different stages in medication handling and usage.
The major reasons for Medication Errors were Dose related errors which constituted the maximum proportion of 70.43% (1058), followed by wrong medication due errors in Brand or Generic names which constituted 17.46% (262)of the medication errors, problems with wrong route for medication administration constituted 5.73% (86)of the medication errors, errors with frequency of administration constituted 2.53% (38) of the medication errors, therapeutic duplication constituted 2.47% (37)of the medication errors, wrong formulation in prescription, miscommunication and wrong patient identification constituted 0.99% (15), 0.2% (3) and 0.19% (2) of the medication errors respectively. This is depicted in Table 2.
| Reasons | Numbers | Percentage |
|---|---|---|
| Wrong medication (Brand name or Generic name) | 262 | 17.46 |
| Dose and Dilution | 1058 | 70.43 |
| Route | 86 | 5.73 |
| Frequency | 38 | 2.53 |
| Therapeutic duplication | 37 | 2.47 |
| Wrong patient identification | 2 | 0.19 |
| Miscommunication | 3 | 0.2 |
| Wrong formulation | 15 | 0.99 |
| Total | 1501 | 100 |
Table 2: Reasons for the medication errors.
Discussion
As depicted in the study, the medication error rate per 100 orders was 5.27 with no fatality. This rate is in consonance with many studies that reported inpatient medication error rates of 4.8% to 5.3% [14,15]. According to a study by Ashcroft et al. the mean error rate was 8.8% [16]. However, on the contrary, this medication error rate in our study is quite low in comparison to many Indian studies which once again can be attributed to the existing well-structured process in our hospital [3,4].
Our study reported 70.43% of dose related errors which is higher than that reported by Kumar et al. as 17.4% [17] and Agarwal et al. as 45.5% [18]. This could be since this being a teaching hospital, medication orders were given by Post Graduate Students which could have culminated in more dose related errors.
In our study, we noted that majority of the medication errors occurred in the age group of 19-64 years. This finding is in concurrence with findings in studies [19-21]. Our study reported that majority of the medication errors were Category B (97.67%) while only 2.33% were Category C errors. This is in contrary to studies which showed Category B errors as only 22.44% [21]. Again, this finding is in consonance with studies done by Hou Ning et al. who observed 86.45% were Category B errors [22]. This can be explained from the robust process of reporting medication errors and a strong top driven approach to imbibe the spirit of medication management and safety with an aim towards process improvement and not nurturing a punitive environment to promote medication error reporting even for “Near misses”. The organisation not only has a well-established process of medication error reporting and monitoring but also conducts dedicated activities to increase awareness among staffs on safe handling and use of medications.
In our study medication administration error was only 2.07%. The frequency of medication administration errors in different studies ranged from 14 to 46 % in other studies [19,23,24]. This could be due to the robust hospital policy, stringent staff training practices and multiple inbuilt checks in the medication handling and use process which acts like a “swiss-cheese” model and helps in error detection before it reaches the stage of administration.
Medication errors related to Chemotherapeutic agents and High Alert Medications constituted only 3.36% of the Medication errors. This is much lower in comparison to that stated in a review article by Alanazi et al. which cited medication errors related to High Risk Medications ranging from 0.24 to 89.6 errors per 100 orders [25]. This can once again be explained with the robust existing process of medication handling and use.
As stated in many studies’ medication errors occur due to lapses in a complicated interconnected process involving use of medications in which physicians as prescribers, nurses as administrators for medications, pharmacists as transcribers, dispensers and medication handlers are accountable [26]. We also noted that physicians, pharmacists and nurses all contributed to medication errors through the share by the physicians was most i.e. 69.8% which can be attributable to the nature of the hospital which is a teaching hospital with post graduate trainee doctors doing prescriptions.
However, despite well-established policies and processes in place and medication error rates being low as described above, we observed that medication errors did occur in our institution leaving a scope for further improvement.
The reasons for Medication Errors can be categories into Human factors, Systemic factors and Environmental factors as below following in-depth analysis:
Human factors
New staffs like doctors including Post Graduate Trainee Doctors, Pharmacists and Nursing staffs who are not well versed with the hospital polices concerning safe handling and use of medications.
Physicians not checking Drug Dictionary leading to errors while prescription writing and not complying with Prescription writing policies making prescriptions illegible at times.
Inappropriate use of metrics, decimals and zeros violating hospital laid down policy based on international guidelines.
Nursing staffs not complying with the hospital policy of checking the patient identifiers and also the 6 Rights (Right Patient, Right Medicine, Right dose, Right route, Right Frequency and Right documentation), before administering medications.
Physicians and the pharmacists not checking patient’s complete medication profile as a part of medicine reconciliation leading to therapeutic duplication.
Pharmacists not cross checking drug orders or question the physicians in case of any controversy due to fear of being rebuked violating the Culture of Safety as envisaged by the Management.
Systemic factors
Inadequate and ineffective orientation of new staffs on hospital policies concerning safe handling and use of Medications.
Sacrificing safety with an aim to complete tasks quickly compromising the Culture of Safety
Failure to implement technology for ordering, indenting, dispending and documenting drug administration.
Failure of teamwork in a complex process like medication handling and use involving multiple healthcare providers.
Environmental factors
Inadequate staffing due to staff attrition rate for nursing staffs and pharmacists.
Managing multiple complex tasks by the nursing staffs like order entry, transcription, IV admixture and drug administration in the scarcity of pharmacists.
Communication failure between staffs during shift handover.
Failure of junior staff supervision by seniors.
Many of the human factors are attributable to behavioural aspects as has been pointed out by many studies. The use of technology like software driven easily accessible drug dictionaries and error proofing through computerised process of ordering, indenting, dispensing and documenting the medication administration through an integrated software can be a good option [27]. The inpatient pharmacy currently uses a software for billing medications only and the hospital management is strongly thinking of a phase wise shift towards imbibing technology as mentioned above. The other interventions undertaken are as follows:
Streamlining and intensifying staff training through mentorship programs for the physicians, pharmacists and nursing staffs in addition to the existing training program. This aims for a dual effect of not only strengthening the staff training but also improving junior/new staff supervision. The importance of encouraging continuous staff education which not only helps knowledge acquisition but also imbibes positive staff attitude and reduces medication errors have been suggested in many studies [28].
Strengthening shift handovers by making patient handoffs documented using SBAR (Situation, Background, Assessment and Recommendation) technique and implementing random checks by the Medical Administration to ensure compliance.
Designating the floor supervisors from the existing senior pool of pharmacy and nursing staffs to improve coordination with the physicians and strengthen teamwork.
Starting prescription audit by a team comprising of members from the Department of Pharmacology and Quality Assurance to review new prescriptions and discharge prescription and spot training of the pharmacists and junior physicians if need be.
Starting with Medication Safety Rounds on alternate days of the week and sharing the round findings with the Medical Superintendent, Nursing Superintendent and Head of the Department, Pharmacology with an aim towards immediate rectification.
Limitations of the Study
As the study was a retrospective study, we could not perform any reconciliation procedure to resolve the medication errors under discussion.
The study could not analyse the pattern of medication errors in the outpatient services as there was no mechanism to track the medication errors for the outpatients or for medications being handled through the outpatient pharmacy.
Conclusion
The study concluded that medication errors occur even in hospital settings with established policies for Safe Handling and Use of Medications. However, those can be restricted from reaching the patient with well-structured dedicated strategies and multi-level checks ( “ Swisscheese” Model) in place aimed towards increasing the safety of medication handling and use. As, Medication errors occur at all stages of medication usage this justifies the “Swiss-cheese” Model with multilevel checks in place. Practice of reporting Category B errors should also be inculcated as Category B errors which are equivalent to “near misses” represent just the tip of the iceberg and have a potential to culminate in medication errors which can not only reach the patient but cause harm. Further in-depth studies are recommended on medication errors including “Near miss” which can throw more light on lapses in an existing process and identify the effective intervention strategies to help further process improvement.
Conflict of Interest
The Authors declare there is no conflict of interest.
Funding
Nil.
Special Acknowledgment
The authors are thankful to the Director, Dr Dilip Kumar Jaiswal and the Registrar, Dr Ichchhit Bharat of MGM Medical College and LSK Hospital, Kishanganj, Bihar for their support in this endeavour. The authors also thank the researchers whose articles have been cited in this article.
References
- https://www.nccmerp.org/about-medication-errors.
- ASHP guidelines on preventing medication errors in hospitals. Am J Hosp Pharm 1993; 50:305-314.
- Gaur S, Sinha A, Srivastava B. Medication errors in medicine wards in a tertiary care teaching hospital of a hill state in India. Asian J Pharm Life Sci 2012; 2:56–63.
- Kumar KS, Venkateswarlu K, Ramesh A. A study of medication administration errors in a tertiary care hospital. Indian J Pharm Pract 2011; 4:37–42.
- Ministry of health Malaysia. Guideline on medication error reporting. 1st Edn 2009.
- Davis NM, Cohen MR. Medication errors: Causes and prevention. Huntingdon Valley, Davis NM Associates 1981.
- http://www.supersalud.gob.cl/observatorio/671/articles-14460_recurso_1.pdf
- Sinha G, Acharya LD, Thunga G, et al. Study of medication errors in general medicine wards of the south Indian tertiary care hospital. Asian J Pharm Clin Res 2016; 9:196-200.
- Karuppannan M, Nee TK, Ali SM, et al. The prevalence of adverse drug event-related orders at a local hospital in Malaysia. Archives Pharm Practice 2013; 4:160.
- https://www.ismp.org/resources/ismp-survey-helps-define-near-miss-and-close-call
- Williamson S. Reporting medication errors and near misses. In: Courtenay M, Griffiths M Edn. Medication safety: An essential guide. Cambridge: Cambridge University Press, 2009; 155-171.
- American society of health-system pharmacists. ASHP guidelines on preventing medication errors in hospitals. Am J Health-Syst Pharm 2018; 75:1493–1517.
- https://www.ahrq.gov/patient-safety/resources/match/matchtab6.html
- Jiménez Muñioz AB, Muiño Miguez A, Rodriguez Pérez MP, et al. Medication error prevalence. Int J Health Care Qual Assur 2010; 23:328-338.
- Bates DW, Boyle DL, Vander Vliet MB, et al. Relationship between medication errors and adverse drug events. J Gen Intern Med 1995; 10:199-205.
- Ashcroft DM, Lewis PJ, Tully MP, et al. Prevalence, nature, severity and risk factors for prescribing errors in hospital inpatients: Prospective study in 20 UK hospitals. Drug Saf 2015; 38:833–843.
- Kumar KS, Venkateswarlu K, Ramesh A. A study of medication administration errors in a tertiary care hospital. Indian J Pharm Pract 2011; 4:37–42.
- Agarwal S, Joshi MC. A study of medication errors associated with prescription drug ordering. Rev Glob Med Healthc Res 2011; 2:166–72.
- Karna KH, Sharma SA, Inamdar SH, et al. Study and evaluation of medication errors in a tertiary care teaching hospital–a baseline study. Int J Pharm Sci 2012; 4:58.
- Solanki ND, Shah C. Root cause analysis of medication errors at a multi-specialty hospital in Western India. Int J Basic Clin Pharmacol 2013; 2:819-823.
- Sandip P, Ashita P, Varsha P, et al. Study of medication error in hospitalised patients in tertiary care hospital. Indian J Pharm Practice 2018; 11:32-36.
- Ning H, Hui T. Analysis of medication errors in provincial hospital. Biomed J Sci Tech Res 2017; 1:962-966.
- Patel N, Desai M, Shah S, et al. A study of medication errors in a tertiary care hospital. Perspectives Clin Res 2016; 7:168-177.
- Al-Jeraisy MI, Alanazi MQ, Abolfotouh MA. Medication prescribing errors in a pediatric inpatient tertiary care setting in Saudi Arabia. BMC Res Notes 2011; 4:294.
- Alanazi MA, Tully MP, Lewis PJ. A systematic review of the prevalence and incidence of prescribing errors with high-risk medicines in hospitals. J Clin Pharm Therapeutics 2016; 41:239–245.
- Keers RN, Williams SD, Cooke J, et al. Causes of medication administration errors in hospitals: A systematic review of quantitative and qualitative evidence. Drug Saf 2013; 36:1045–1067.
- https://www.ncbi.nlm.nih.gov/books/NBK499956/
- Ma´rquez-Herna´ndez VV, FuentesColmenero AL, Cañadas-Nu´ñez F, et al. Factors related to medication errors in the preparation and administration of intravenous medication in the hospital environment. PLoS ONE 2019; 14:e0220001.
Author Info
Manasij Mitra1 and Maitraye Basu2*
1Department of Anesthesiology, MGM Medical College and LSK Hospital, Kishanganj, Bihar, India2Department of Biochemistry, MGM Medical College and LSK Hospital, Kishanganj, Bihar, India
Citation: Manasij Mitra, Maitraye Basu, An Analysis of Medication Errors in a Tertiary Care Teaching Hospital, J Res Med Dent Sci, 2020, 8(3): 17-24
Received: 30-Mar-2020 Accepted: 16-Apr-2020
