Research - (2021) Volume 9, Issue 7
Analysis of Plasma Osteocalcin Levels, Status of Oral Disease and Alteration in Mandibular Bone Density in Postmenopausal Women
Bhanupriya Singh1*, Pallavi Gahlowt2, Deepinder Kaur3 and Ishanika Goswami4
*Correspondence: Bhanupriya Singh, Department of Radiodiagnosis, Dr. Ram Manohar Lohiya Institute of Medical Sciences, India, Email:
Abstract
Aim: The present study was undertaken for assessing Plasma Osteocalcin levels, status of Oral Disease and alteration in Mandibular Bone Density in Postmenopausal Women (PMW). Materials and methods: 80 premenopausal women and 80 PMW were enrolled. For analysing the oral dryness, clinical score of oral dryness (CSOD) on a scale of upto 10 was used in all each subject. Complete dental profiling of all the subjects was done. Digital panoramic radiographs were taken for all the subjects. Measurements were made on each PAN and following indices were evaluated for assessing the mandibular BMD: Mandibular cortical index (MCI), Mandibular cortical index (MCI), panoramic mandibular index (PMI), Mandibular cortical width (MCW), and Fractal dimension (FD). Osteocalcin levels were evaluated with ELISA technique. All the results were recorded and analysed. Results: Mean osteocalcin levels of PMW (453.12 ng/mL) were significantly higher in comparison to the premenopausal subjects (249.28 ng/mL). PMW had significantly higher clinical score of oral dryness and number of peri-apical radiolucencies in comparison to premenopausal women. Bone mineral density as assessed by mandibular cortical index were found to be negatively and significantly correlated with oral disease status and osteocalcin levels. Only mandibular cortical index varied significantly statistically in between the two study groups. Conclusion: There is significantly higher prevalence of oral lesions along with oral dryness in postmenopausal women. Also, thinning of mandibular cortex is significantly higher in postmenopausal women. Higher plasma osteocalcin levels helps in predicting osteopenia/osteoporosis at an early stage in such subjects. Clinical significance: Special considerations should be made in postmenopausal women while doing treatment planning for prosthetic purposes (dental implants) as edentulous bone is at higher risk of osteoporosis in such patients.
Keywords
Osteocalcin, Postmenopausal, Mandibular bone density.
Introduction
Menopause is invariable accompanied with a series of physical alterations. Most of these alterations are directly linked to estrogen loss, including vaginal dryness and bone demineralization. Some authors have also reported slight higher prevalence of cardiovascular pathologies in postmenopausal women (PMW). Among PMW, osteoporosis is a prime concern resulting in considerable morbidity and mortality. It has also been reported that more than half of women over the age of sixty five years have a compression fracture. Hence; it is necessary to maintain bone mass for preventing the osteoporosis. Vertebral fractures (due osteoporosis in PMW) can also result in loss of height, kyphosis and lordosis (postural changes) [1-3].
It is probably inappropriate to analyse the incidence and statistical data in relation to menopause as it is a female’s physiologic alteration. However; it increases the risk for development of different pathological lesions. Occurrence of osteoporosis involving the mandible in these patients increases the risk for development of pathologies involving oral soft and hard tissues. This can result in loosening of teeth thereby increasing the chances of tooth loss. Loss of teeth in the posterior tooth region can lead to loss of neuromuscular stability of the mandible, decrease in masticatory efficiency, poor aesthetics etc. [4,5].
For appreciating the pathophysiologic pathways for bone metabolic pathologies, different biochemical markers of bone metabolism are considered as significant tools. The assessment of the protein fragments produced by osteoblasts (osteocalcin, enzymes produced during osteogenesis: Alkaline phosphatase) are of significant importance for analysing the osteoblastic activity [6,7]. Hence the present study was undertaken for assessing Plasma Osteocalcin levels, status of Oral Disease and alteration in Mandibular Bone Density in Postmenopausal Women.
Materials and Methods
The present study was conducted with the aim of assessing Plasma Osteocalcin levels, status of Oral Disease and alteration in Mandibular Bone Density in Postmenopausal Women. Among these, 80 subjects were premenopausal women while the remaining 80 were PMW. Only those subjects were included in the PMW group, in which there was a minimum of 2 years history of start of menopause at the time of study. Written consent was obtained from all the subjects after explaining in detail the entire research protocol. Recording of complete demographic and clinical details of all the patients was done. Blood samples were obtained from all the patients and complete lipid and haematological profile was recorded. From the medical record files, body mass index (BMI) plus waist circumference was recorded. Subjects with body mass index of more than equal to 23 Kg/m2 along with waist circumference of more than or equal to 80 cm were categorised as obese. Complete oral examination was done in all the subjects using mouth mirror, probe and tweeter for identifying presence of any oral lesion (if any) and dryness. For analysing the dryness, clinical score of oral dryness (CSOD) on a scale of upto 10 was used in all each subject, based on criteria described previously in the literature. Scoring of CSOD was as follows [8]:
- Score of 1 to 3 (Low CSOD score): Mild dryness.
- Score of 4 to 6 (Medium CSOD score): Moderate dryness, and
- Score of 7 to 10 (High CSOD score): Extreme dryness.
Complete dental profiling of all the subjects was done, which included recording of the number of missing teeth (except for third molar) and thorough periodontal examination using Hu-Friedy 12 UNC colour-coded periodontal probe. Along the six clinical sites of a tooth (distobuccal, midbuccal, mesiobuccal, distolingual, midlingual, and mesiolingual), measurement of bleeding on probing (BOP), probing depth (PD) and clinical attachment loss (AL) was done for diagnosing periodontal pathologies.
After carrying out the oral examination, digital panoramic radiographs were taken for all the subjects during the same visit. An experienced and radiologist analysed the presence of peri-apical lesions, alveolar bone loss and mandibular bone mineral density indices. After examining digital panoramic radiographs and carrying out clinical examination, diagnoses of diseases teeth was established based on presence of peri-apical radiolucencies and clinical appearance [9]. Alveolar bone loss (ABL) was assessed radiographically be evaluating the mesial and distal surfaces of six teeth and thereby calculating the ABL% based on criteria previously described in literature [10].
Measurements were made on each PAN and following indices were evaluated for assessing the mandibular BMD:
- Mandibular cortical index (MCI).
- Mandibular cortical index (MCI).
- Panoramic mandibular index (PMI).
- Mandibular cortical width (MCW).
- Fractal dimension (FD).
MCI [11]
As per classification given by Klemetti et al. MCI (inferior mandibular cortical thickness) is classified as follows (Figure 1A to 1C):
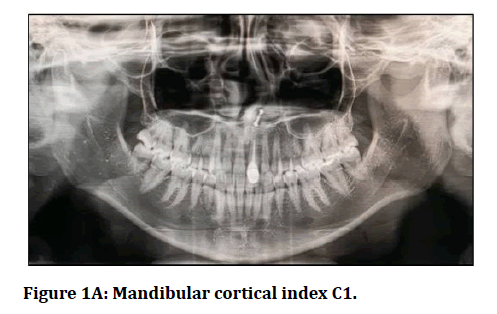
Figure 1A: Mandibular cortical index C1.
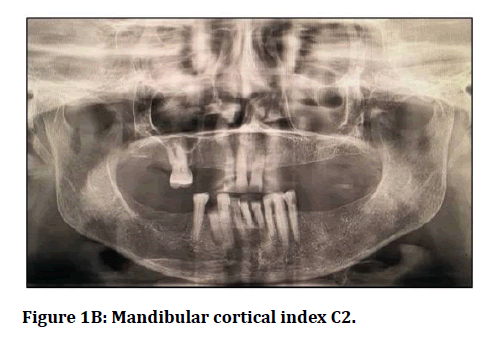
Figure 1B: Mandibular cortical index C2.
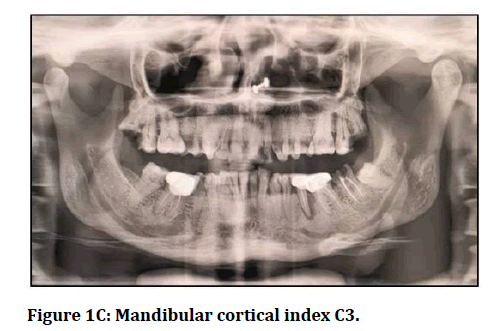
Figure 1C: Mandibular cortical index C3.
C1: Sharp and even endosteal margin of the cortex
C2: Presence of lacunar resorption/ cortical residues on endosteal margin on one or both sides.
C3: Presence of heavy endosteal residues on the cortical layer.
PMI: It refers to the ration obtained by dividing mandibular cortex thickness with distance among mental foramen’s inferior margin and the inferior mandibular cortex [12].
MCW: It refers to the line that was at right angle to the mandible’s inferior border at the middle of the mental foramen [13].
FD: Digital radiograph were opened with PixelStyle software and Image J software and FD was calculated based on criteria described previously in literature [14,15].
Haematological analysis
All the patients were recalled in the morning and peripheral venous blood samples were obtained after overnight fasting. All the samples were stored at–80 degree centigrade and were sent to pathology department for further analysis. ELISA technique (BGLAP ELISA kit, USA) was used for evaluating the osteocalcin levels as per manufacturer’s instructions.
All the results were recorded in Microsoft excel sheet and were analysed by SPSS software. Mann-Whitney U test, Spearman correlation coefficient and student t test were used for assessment of level of significance. P-value of less than 0.05 was taken as significant.
Results
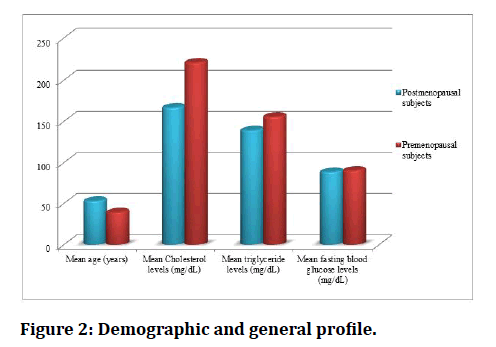
In the present study, 80 PMW and 80 premenopausal subjects were enrolled. Mean age of the PMW and premenopausal subjects was 53.12 years and 39.36 years respectively. Mean fasting blood glucose levels of PMW and premenopausal women was found to be 88.6 mg/dL and 80.4 mg/dL respectively (Figure 2).
Figure 2: Demographic and general profile.
While analysing the plasma osteocalcin levels, it was observed that mean osteocalcin levels of PMW (453.12 ng/mL) were significantly higher in comparison to the premenopausal subjects (249.28 ng/mL) (p- value < 0.05) as shown in Table 1. Average number of missing teeth in postmenopausal women was 7 while in premenopausal women were 2; on comparing the results were found to be statistically significant (Table 2). Mean attachment loss was 3.1 mm and 2.2 mm in postmenopausal women and premenopausal women respectively. Mean ABL% was 27.8% and 20.4% in postmenopausal women and premenopausal women respectively. On comparing statistically, it was observed that PMW had significantly higher clinical score of oral dryness and number of peri-apical radiolucencies in comparison to premenopausal women. Plasma osteocalcin levels among PMW with mandibular cortical index of C2-C3 (435.1 ng/mL) were significantly higher in comparison to PMW with mandibular cortical index of C1 (321.8 ng/mL) as shown in Table 3. It was also seen that mean ABL%, mean number of missing teeth and mean value of clinical attachment loss was significantly higher in PMW with mandibular cortical index of C2-C3 in comparison to subjects with index of C1 (pvalue< 0.05). Also, it was observed that BMD as assessed by mandibular cortical index were found to be negatively and significantly correlated with oral disease status and osteocalcin levels as shown in Table 4. On comparing the different indices and parameters of BMD of mandible between PMW and premenopausal women, it was seen that only mandibular cortical index varied significantly statistically in between the two study groups (pvalue< 0.005) as shown in Table 5.
Table 1: Comparison of plasma osteocalcin levels.
| Osteocalcin levels (ng/mL) | Premenopausal subjects | Postmenopausal subjects | p-value |
|---|---|---|---|
| Mean | 249.28 | 453.12 | 0.0001* |
| SD | 123.48 | 223.75 |
*: Significant
Table 2: Correlation of oral disease status with menopausal status.
| Parameter | Premenopausal subjects | Postmenopausal subjects | p-value | |
|---|---|---|---|---|
| Average missing teeth number | 2 | 7 | 0.001* | |
| Mean value of attachment loss (mm) | 2.2 | 3.1 | 0.003* | |
| Mean ABL% | 20.4 | 27.8 | 0.001* | |
| Number of per-apical radiolucencies | 0 (absent) | 68 | 42 | 0.000* |
| More than 1 | 12 | 38 | ||
| Clinical score of oral dryness | 0 | 45 | 18 | 0.000* |
| 1 to 3 | 32 | 55 | ||
| More than or equal to 4 | 3 | 7 | ||
*: Significant
Table 3: Plasma osteocalcin levels, ABL%, number of missing teeth, and mean value of clinical attachment level among PMW with different mandibular cortical index.
| Parameter | Mandibular cortical index | p-value | |
|---|---|---|---|
| C1 | C2 – C3 | ||
| Osteocalcin levels (ng/mL) | 321.8 | 435.1 | 0.020* |
| ABL% | 18.3 | 30.7 | 0.000* |
| Number of missing teeth | 4.1 | 8.9 | 0.010* |
| Mean value of clinical attachment loss | 2.5 | 3.3 | 0.001* |
*: Significant
Table 4: Correlation of osteocalcin levels, ABL%, number of missing teeth and mean value of clinical attachment loss with mandibular cortical index in PMW.
| Spearman's rho | Mandibular cortical index | |
|---|---|---|
| Osteocalcin levels | Correlation Coefficient | -0.471 |
| p- value | 0.000* | |
| ABL% | Correlation Coefficient | -0.396 |
| p- value | 0.003* | |
| Number of missing teeth | Correlation Coefficient | -0.513 |
| p- value | 0.001* | |
| Mean value of clinical attachment loss | Correlation Coefficient | -0.493 |
| p- value | 0.002* | |
*: Significant
Table 5: Mandibular bone density comparison.
| Parameter | Postmenopausal subjects | Premenopausal subjects | p- value | |
|---|---|---|---|---|
| Right mandibular cortical index | C1 | 75 | 59 | 0.000* |
| C2 | 5 | 18 | ||
| C3 | 0 | 3 | ||
| Right mandibular cortical index | C1 | 75 | 59 | 0.001* |
| C2 | 5 | 18 | ||
| C3 | 0 | 3 | ||
| Panoramic mandibular index | Right | 2.27 | 2.29 | 0.423 |
| Left | 2.29 | 2.26 | 0.38 | |
| Mandibular cortical width (mm) | Right | 3.42 | 3.57 | 0.721 |
| Left | 3.49 | 3.63 | 0.873 | |
| Fractal dimension | Right | 1.2 | 1.21 | 0.25 |
| Left | 1.22 | 1.25 | 0.336 | |
*: Significant
Discussion
“Menopause” word is of Greek origin referring to month and cessation. At times, the term is used for describing climacteric, which denotes happenings associated with “the changes in life. It has been seen that with advancing age, bone mass decreases in humans. In the approximately thirties and forties, human bones show decline in density along with increasing porosity. This is specifically exaggerated in women after the occurrence of menopause. Hence; significantly higher risk of osteoporosis is associated in such women. Mineral levels of the skeleton have been shown to affect the BMD of mandible, thereby resulting in generalized bone resorption [16,17].
Until the last decade, the association between energy metabolism and osseous tissue was regarded as unidirectional in which there are multifaceted communications between leptin, adiponectin, and neuropeptides. Literature from the animal studies has demonstrated that osseous cells control glucose and fat metabolism through osteocalcin. Osteocalcin is a protein in nature and is found to be present mainly in bone and dentine tissue. It is known to play a crucial role in regulating calcium homeostasis throughout the bone mineralization process. After its formation, a significant proportion of it is assimilated into the bone’s extracellular matrix. However, in systemic circulation, a small proportion of it is released. Hence it is regarded as a specific marker for demonstrating osteoblastic activity [18-22]. Hence the present study was undertaken for assessing Plasma Osteocalcin levels, status of Oral Disease and alteration in Mandibular Bone Density in Postmenopausal Women.
In the present study, 80 PMW and 80 premenopausal subjects were enrolled. Mean osteocalcin levels of PMW were significantly higher in comparison to the premenopausal subjects as shown in Table 1. Also PMW had significantly higher clinical score of oral dryness and number of peri-apical radiolucencies in comparison to premenopausal women (Table 2). Our results were in concordance with the results obtained by Kalaiselvi et al. [23] and Thanakun et al. [24] who also reported similar findings in their respective studies. In the study conducted by Kalaiselvi et al, authors analysed correlation between bone remodelling biomarkers and osteocalcin with BMD in post-menopausal non osteoporotic and osteoporotic women. A total of 30 nonosteoporotic (Group 1) and 30 osteoporotic subjects were (Group 2) were enrolled in their study and serum osteocalcin and BMD was evaluated. In PMW, they observed a negative association among osteocalcin level and the BMD. Also significant results were obtained by the authors while comparing the mean serum osteocalcin and BMD values among both the study groups [23,24]. In another study conducted by Thanakun et al. [24] authors compared the osteocalcin levels, oral pathologies, and mandibular BMD alterations among PMW and premenopausal women. After analysing 92 subjects, they observed significantly higher osteocalcin levels in PMW in comparison to premenopausal women. Similar to our study, they also reported significantly higher incidence of oral lesions in PMW. However; in PMW they reported significantly lower mandibular BMD [24].
In the present study, mean plasma osteocalcin levels among PMW with mandibular cortical index of C2- C3were significantly higher in comparison to PMW with mandibular cortical index of C1 (Table 3). Also, mean ABL %, mean number of missing teeth and mean value of clinical attachment loss was significantly higher in PMW with mandibular cortical index of C2-C3. In the past literature, reliability of MCI as a diagnostic tool has been proved from time to time for screening PMW with osteoporosis. Occurrence of any form of cortical erosion (C2 or C3) could be considered as a valuable indicator of reduced BMD since in nearly more than three fourth of subjects, it is accompanied with at least osteopenia. In a previous study conducted by Gaur et al, authors showed that a significant relationship exists between BMD and MCI. They observed specificity and sensitivity of be 88.9% and 100% respectively [25,26].
In the present study, BMD was found to be negatively and significantly correlated with oral disease status and osteocalcin levels (Table 4). Impact of menopause on BMD and mandibular bone width was evaluated by Munakata M et al, who evaluated 30 premenopausal and 42 postmenopausal subjects. They observed that trabecular BMD of PMW was lower in comparison to premenopausal women. They also reported negative correlation between Trabecular region width with BMD and positive correlation between cortical width and BMD.
Their results showed that both bone (mandible) quality and quantity is affected by menopause [27].
In the present study, it was observed that only mandibular cortical index varied significantly statistically in between the two study groups (Table 5). Previous studies have also demonstrated negative correlation of plasma osteocalcin levels with BMI and BMD. In a study conducted by Sternfeld et al, authors demonstrated that alterations in the menopausal status was not correlated with obesity but was significantly correlated with increased waist circumference [28,29]. In another study conducted by Irie et al. authors evaluated the impact of menopause on mandibular bone by assessing the morphological alterations in the mandible of ovariectomized rats. However; they not only observed significantly reduction for both bone mass and width of trabecular bone but at the same time, also observed significantly augmented distances between trabeculae in ovariectomized rats in comparison to healthy controls [30].
Conclusion
Under the light of above obtained results, the authors conclude that there is significantly higher prevalence of oral lesions along with oral dryness in postmenopausal women. Also, thinning of mandibular cortex is significantly higher in postmenopausal women. Higher plasma osteocalcin levels helps in predicting osteopenia/ osteoporosis at an early stage in such subjects. Hence we recommend maintaining of adequate oral hygiene and regular health check at timely intervals.
References
- Whelan TJ, Goss PE, Ingle JN, et al. Assessment of quality of life in MA.17: A randomized, placebo-controlled trial of letrozole after 5 years of tamoxifen in postmenopausal women. J Clin Oncol 2005; 23:6931–40.
- Żołnierczuk-Kieliszek D, Kulik TB, Jarosz MJ, et al. Quality of life in peri- and post-menopausal polish women living in lublin province-Differences between urban and rural dwellers. Ann Agric Environ Med 2012; 19:129–33.
- Lieben L, Callewaert F, Bouillon R. Bone and metabolism: A complex crosstalk. Horm Res 2009; 71:134-138.
- Fukumoto S, Martin J. Bone as an endocrine organ. Trends Endocrinol Metab 2009; 20:230-236.
- Seibel MJ. Biochemical markers of bone remodelling. Endocrinol Metab Clin North Am 2003; 32:83-113.
- Som N, Ray S. Menopause-specific quality of life of urban women in West Bengal, India. Menopause Int 2012; 18:99–105.
- Boulet MJ, Oddens BJ, Lehert P, et al. Climacteric and menopause in seven South-East Asian countries. Maturitas 1994; 19:157–76.
- Osailan SM, Pramanik R, Shirlaw P, et al. Clinical assessment of oral dryness: development of a scoring system related to salivary flow and mucosal wetness. Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 114:597–603.
- Halse A, Molven O. A strategy for the diagnosis of periapical pathosis. J Endodontics 1986; 12:534–538.
- Beckstrom BW, Horsley SH, Scheetz JP, et al. Correlation between carotid area calcifications and periodontitis: A retrospective study of digital panoramic radiographic findings in pretreatment cancer patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2007; 103:359–366.
- Klemetti E, Kolmakov S, Kröger H. Pantomography in assessment of the osteoporosis risk group. Eur J Oral Sci 1994; 102:68–72.
- Benson BW, Prihoda TJ, Glass BJ. Variations in adult cortical bone mass as measured by a panoramic mandibular index. Oral Surg Oral Med Oral Pathol 1991; 71:349–356.
- Dutra V, Devlin H, Susin C, et al. Mandibular morphological changes in low bone mass edentulous females: evaluation of panoramic radiographs. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2006; 102:663–668.
- Koh KJ, Park HN, Kim KA. Prediction of age-related osteoporosis using fractal analysis on panoramic radiographs. Imaging Sci Dent 2012; 42:231–235.
- Yaşar F, Akgünlü F. The differences in panoramic mandibular indices and fractal dimension between patients with and without spinal osteoporosis. Dentomaxillofac Radiol 2006; 35:1–9.
- Von Wowern N. Microradiographic and histomorphometric indices of mandibles for diagnosis of osteopenia. Scand J Dent Res 1982; 90:47–63.
- Lai YL. Osteoporosis and periodontal disease. J Chin Med Assoc 2004; 67:387–388.
- Jeffcoat MK. Osteoporosis: A possible modifying factor in oral bone loss. Ann Periodontal 1998; 3:312–21.
- Reid IR. Relationships between fat and bone. Osteoporos Int 2008; 19:595-606.
- Fukumoto S, Martin J. Bone as an endocrine organ. Trends Endocrinol Metab 2009; 20:230-236.
- Seibel MJ. Biochemical markers of bone remodelling. Endocrinol Metab Clin North Am 2003; 32:83-113.
- Lee NK, Karsenty G. Reciprocal regulation of bone and energy metabolism. J Musculoskelet Neuronal Interact 2008; 8:351.
- Kalaiselvi VS, Prabhu K, Ramesh M, et al. The association of serum osteocalcin with the bone mineral density in post menopausal women. J Clin Diagn Res 2013; 7:814–816.
- Thanakun S, Pornprasertsuk-Damrongsri S, Na Mahasarakham CP, et al. Increased plasma osteocalcin, oral disease, and altered mandibular bone density in postmenopausal women. Int J Dent 2019; 2019:3715127.
- Taguchi A. Triage screening for osteoporosis in dental clinics using panoramic radiographs. Oral Diseases 2010; 16:316–327.
- Gaur B, Chaudhary A, Wanjari PV, et al. Evaluation of panoramic aadiographs as a screening tool of osteoporosis in post menopausal women: A cross sectional study. J Clin Diagnostic Res 2013; 7:2051–2055.
- Munakata M, Tachikawa N, Honda E, et al. Influence of menopause on mandibular bone quantity and quality in Japanese women receiving dental implants. Arch Osteoporos 2011; 6:51‐57.
- Hu WW, Ke YH, He JW. Serum osteocalcin levels are inversely associated with plasma glucose and body mass index in healthy Chinese women. Acta Pharmacologica Sinica 2014; 35:1521–1526.
- Sternfeld B, Wang H, Quesenberry CP. Physical activity and changes in weight and waist circumference in midlife women: Findings from the study of women’s health across the nation. Am J Epidemiol 2004; 160:912–922.
- Irie M, Sakakura Y, Tsuruga E, et al. Three-dimensional changes of the mandible and alveolar bone in the ovariectomized rat examined by micro-focus computed tomography. J Jpn Soc Periodontol 2004; 46:288–293.
Author Info
Bhanupriya Singh1*, Pallavi Gahlowt2, Deepinder Kaur3 and Ishanika Goswami4
1Department of Radiodiagnosis, Dr. Ram Manohar Lohiya Institute of Medical Sciences, Lucknow, UP, India2Department Of Community Medicine, Padmashree Dr. D.Y. Patil Medical College, Nerul, Navi Mumbai, India
3SKSS Dental College Sarabha, Ludhiyana, India
4CHC Sikandara, Kanpur, India
Citation: Bhanupriya Singh, Pallavi Gahlowt, Deepinder Kaur, Ishanika Goswami,Analysis of Plasma Osteocalcin Levels, Status of Oral Disease and Alteration in Mandibular Bone Density in Postmenopausal Women, J Res Med Dent Sci, 2021, 9(7): 442-448
Received: 08-Jul-2021 Accepted: 26-Jul-2021