Research - (2022) Volume 10, Issue 1
Antibacterial Activity of Different Leaves and Bark Extracts of Ficus Benghalensis
K Mahammad Areef1* and Mohammed Mazher Ahmed2
*Correspondence: K Mahammad Areef, Department of Pharmacy, Dr. K.V. Subba Reddy Institute of Pharmacy, Jawaharlal Nehru Technological University, Anantapur, Andhra Pradesh, India, Email:
Abstract
Ficus benghalensis is one of the important medicinal plants belonging to the family moraceae. It is a tree indigenous to India. Ayurveda and Unani medicinal systems use it for the treatment of several ailments. Ficus benghalensis has Anti pyretic, Anti helminthic, Anti-microbial, Hepato protective and Anti-cancer activities. As per World Health Organization many people are suffering from microbial infections. The present study was designed to evaluate the anti-microbial activity of Ficus benghalensis. The preliminary phytochemical studies determine the various secondary metabolites like Carbohydrates, Glycosides, Saponins, and Alkaloids are present. This aqueous extract was screened for their antimicrobial activity against 2 pathogen bacteria by agar cup-plate method. These methanol extract shows significant activity against E. coli & K. pneumonia 100, 200 and 300µgm/ml. The Activity Index of leaf extract and bark extract is 1.2, 1.23, 1.26 and 1.33, 1.14, 1.18 (E. coli) and 1.8, 1.42, 1.23 and 1.63, 1.53, 1.31(K. pneumonia) respectively and compared with a standard drug Amoxicillin. This study gives the way for further studies to elucidate the exact mechanism of action.
Keywords
Anti-Bacterial activity, Ficus benghalensis, E. coli, Pneumonia
Introduction
The ancient Egyptian polymath Imhotep is believed by James Henry Breasted to have extracted medicine from plants. The word "Pharmacognosy" itself is derived, however, from two Greek words pharmakon (drug), and gnosis (knowledge). The term "Pharmacognosy" was used for the first time by the Austrian physician Schmidt in 1811 and 1815 by Cr. Anotheus Seydler in a work titled Analecta Pharmacogenetics.
Originally—during the 19th century and the beginning of the 20th century—"Pharmacognosy" was used to define the branch of medicine or commodity sciences (Warenkunde in German) which deals with drugs in their crude, or unprepared, form. Crude drugs are the dried, unprepared material of plant, animal or mineral origin, used for medicine. The study of these materials under the name Pharmacognosy was first developed in Germanspeaking areas of Europe, while other language areas often used the older term material medical taken from the works of Galen and Dioscorides. In German the term drogenkunde ("science of crude drugs") is also used synonymously
As late as the beginning of the 20th century, the subject had developed mainly on the botanical side, being particularly concerned with the description and identification of drugs both in their whole state and in powder form. Such branches of Pharmacognosy are still of fundamental importance, particularly for pharmacopoeial identification and quality control purposes, but rapid development in other areas has enormously expanded the subject. The advent of the 21st century brought a renaissance of Pharmacognosy and its conventional botanical approach has been broadened up to molecular and metabolomics level.
Although most Pharmacogenetics studies focus on plants and medicines derived from plants, other types of organisms are also regarded as pharmaco kinetically interesting, in particular, various types of microbes (bacteria, fungi, etc.), and, recently, various marine organisms.
In addition to the previously mentioned definition, the American Society of Pharmacognosy also defines Pharmacognosy as "the study of natural product molecules (typically secondary metabolites) that are useful for their medicinal, ecological, gustatory, or other functional properties. Other definitions are more encompassing, drawing on a broad spectrum of biological subjects, including botany, ethno botany, marine biology, microbiology, herbal medicine, chemistry, biotechnology, photochemistry, pharmacology, pharmaceutics, clinical pharmacy and pharmacy practice [1].
Medical ethno botany: the study of the traditional use of plants for medicinal purposes; ethno pharmacology: the study of the pharmacological qualities of traditional medicinal substances; the study of phytotherapy (the medicinal use of plant extracts); and photochemistry, the study of chemicals derived from plants (including the identification of new drug candidates derived from plant sources). Zoo Pharmacognosy, the process by which animals self-medicate, by selecting and using plants, soils, and insects to treat and prevent disease. Marine Pharmacognosy, the study of chemicals derived from marine organisms.
At the 9th congress of Italian society of Pharmacognosy it was stated that current return of Phyto-therapy was clearly reflected by the increased market of such products. In 1998 the latest figures available for Europe, the total OTC market for herbal medicinal products reached a figure of $6 billion, with consumption for Germany of $2.5 billion, France $1.6 billion and Italy $600 million. In the US, where the use of herbal products has never been as prevalent as in continental Europe, the market for all herb sales reached a peak in 1998 of $700 billion. This welcomed the scientific investigation of a rigorous nature. The plant kingdom still holds many species of plants containing substances of medicinal value which have yet to be discovered. Large numbers of plants are constantly being screened for their possible pharmacological value.
Biological background
The carotenoids in primrose produce bright red, yellow and orange shades. On average, people consuming diets rich in carotenoids from natural foods, such as fruits and vegetables, are healthier and have lower mortality from a number of chronic illnesses.
All plants produce chemical compounds as part of their normal metabolic activities. These phytochemicals are divided into (1) Primary metabolites such as sugars and fats, which are found in all plants; and (2) Secondary metabolites—compounds which are found in a smaller range of plants, serving a more specific function. For example, some secondary metabolites are toxins used to deter predation and others are pheromones used to attract insects for pollination. It is these secondary metabolites and pigments that can have therapeutic actions in humans and which can be refined to produce drugs—examples are inulin from the roots of dahlias, quinine from the cinchona, THC and CBD from the flowers of cannabis, morphine and codeine from the poppy, and digoxin from the foxglove. Plants synthesize a bewildering variety of phytochemicals but most are derivatives of a few biochemical motifs:
Alkaloids
Alkaloids are a class of chemical compounds containing a nitrogen ring. Alkaloids are produced by a large variety of organisms, including bacteria, fungi, plants, and animals, and are part of the group of natural products (also called secondary metabolites). Many alkaloids can be purified from crude extracts by acid-base extraction. Many alkaloids are toxic to other organisms. They often have pharmacological effects and are used as medications, as recreational drugs, or in entheogenic rituals. Examples are the local anaesthetic and stimulant cocaine; the psychedelic psilocin; the stimulant caffeine; nicotine; the analgesic morphine; the antibacterial berberine; the anticancer compound vincristine; the anti-hypertension agent reserpine; the cholinomimetic galantamine; the spasm lysis agent atropine; the vasodilator vincamine; the anti-arrhythmia compound [2].
Quinidine
The anti-asthma therapeutic ephedrine; and the antimalarial drug quinine. Although alkaloids act on a diversity of metabolic systems in humans and other animals, they almost uniformly invoke a bitter taste.
Polyphenols
Also known as phenolic are compounds that contain phenol rings. The anthocyanin’s that give grapes their purple colour, the isoflavones, the phytoestrogens from soy and the tannins that give tea its astringency are phenolic.
Glycosides
Glycosides are molecules in which a sugar is bound to a non-carbohydrate moiety, usually a small organic molecule. Glycosides play numerous important roles in living organisms. Many plants store chemicals in the form of inactive glycosides. These can be activated by enzyme hydrolysis, which causes the sugar part to be broken off, making the chemical available for use. Many such plant glycosides are used as medications. In animals and humans, poisons are often bound to sugar molecules as part of their elimination from the body. An example is the cyan glycosides in cherry pits that release toxins only when bitten by an herbivore.
Terpenes
Terpenes are a large and diverse class of organic compounds, produced by a variety of plants, particularly conifers, which are often strong smelling and thus may have had a protective function. They are the major components of resin, and of turpentine produced from resin. (The name "Terpenes" is derived from the word "turpentine"). Terpenes are major biosynthetic building blocks within nearly every living creature. Steroids, for example, are derivatives of the triterpene squalene. When Terpenes are modified chemically, such as by oxidation or rearrangement of the carbon skeleton, the resulting compounds are generally referred to as terpenoids. Terpenes and terpenoids are the primary constituents of the essential oils of many types of plants and flowers. Essential oils are used widely as natural flavour additives for food, as fragrances in perfumery, and in traditional and alternative medicines such as aromatherapy.
Synthetic variations and derivatives of natural Terpenes and terpenoids also greatly expand the variety of aromas used in perfumery and flavours used in food additives. Vitamin A is an example of Terpenes. The fragrance of rose and lavender is due to monoterpenes. The carotenoids produce the reds, yellows and oranges of pumpkin, corn and tomatoes.
A consortium of plant molecular researchers at Washington State University, the Donald Dan forth Plant Science Center, the National Center for Genome Resources, and the University of Illinois at Chicago began an NIH-sponsored study of over thirty medicinal plant species late 2009. The initial work, to develop a sequence reference for the Transcriptomics of each, has led to the development of the Medicinal Plant Transcription.
Issues in phytotherapy
The part of Pharmacognosy focusing on the use of crude extracts or semi-pure mixtures originating from nature, namely phytotherapy, is probably the best known and also the most debated area in Pharmacognosy. Although phytotherapy is sometimes considered as alternative medicine, when critically conducted, it can be considered the scientific study on the effects and clinical use of herbal medicines. Consequently, herbal products might also become officially approved for clinical application as botanical drugs (e.g., Veregen (sinecatechins), a green tea leaves extract, approved for use by FDA.
Constituents and drug synergism
One characteristic of crude drug material is that constituents may have an opposite, moderating or enhancing effect. Hence, the final effect of any crude drug material will be a product of the interactions between the constituents and the effect of each constituent on its own. To effectively study the existence and effect of such interactions, scientific studies must examine the effect that multiple constituents, given concurrently, have on the system. Herbalists assert that as Phyto pharmaceuticals rely upon synergy for their activities, plants with high levels of active constituents like ginsenosides or hypericin may not correlate with the strength of the herbs. In Phyto pharmaceuticals or herbal medicine, the therapeutic effects of herbs cannot be determined unless its active ingredient or cofactors are identified or the herb is administered as a whole. One way to indicate strength is standardization to one or several marker compound that is believed to be mainly responsible for the biological effects. However, many herbalists believe that the active ingredient in a plant is the plant itself.
Sustainable sources of plant and animal drugs
As species face loss of habitat or overharvesting, there have been new issues to deal with in sourcing crude drugs. These include changes to the herb from farming practices, substitution of species or other plants altogether, adulteration and cross-pollination issues. For instance, ginseng which is field farmed may have significant problems with fungus, making contamination with fungicides an issue. This may be remedied with woods grown programs, but they are insufficient to produce enough ginsengs to meet demand. The wild crafted Echinacea, black cohosh and American ginseng often rely upon old growth root, often in excess of 50 years of age and it is not clear that younger stock will have the same pharmaceutical effect. Black cohosh may be adulterated with the related Chinese actea species, which is not the same. Ginseng may be replaced by ginseniodes from Jiaogulan which has been stated to have a different effect than the full panax root [3].
The problem may be exacerbated by the growth of pills and capsules as the preferred method of ingesting medication as they are cheaper and more available than traditional, individually tailored prescriptions of raw medicinally but the contents are harder to track. Seahorses are a case in point: Seahorses once had to be of a certain size and quality before they were accepted by practitioners and consumers. But declining availability of the preferred large, pale and smooth seahorses has been offset by the shift towards pre-packaged medicines, which make it possible for TCM merchants to sell previously unused juvenile, spiny and dark-coloured animals. Today almost a third of the seahorses sold in China are pre-packaged.
The farming of plant or animal species for medicinal purposes has caused difficulties. Rob Parry Jones and Amanda Vincent write: One solution is to farm medicinal animals and plants. Chinese officials have promoted this as a way of guaranteeing supplies as well as protecting endangered species. And there have been some successes —notably with plant species, such as American ginseng —which is used as a general tonic and for chronic coughs. Red deer, too, have for centuries been farmed for their antlers, which are used to treat impotence and general fatigue. But growing your own is not a universal panacea. Some plants grow so slowly that cultivation in not economically viable. Animals such as musk deer may be difficult to farm, and so generate little profit. Seahorses are difficult to feed and plagued by disease in captivity. Other species cannot be cultivated at all. Even when it works, farming usually fails to match the scale of demand. Overall, cultivated TCM plants in China supply less than 20 per cent of the required 1.6 million tonnes per annum. Similarly, China's demand for animal products such as musk and pangolin scales far exceeds supply from captive-bred sources.
Farming alone can never resolve conservation concerns, as government authorities and those who use Chinese medicine realise. For a start, consumers often prefer ingredients taken from the wild, believing them to be more potent. This is reflected in the price, with wild oriental ginseng fetching up to 32 times as much as cultivated plants. Then there are welfare concerns. Bear farming in China is particularly controversial. Around 7600 captive bears have their bile "milked" through tubes inserted into their gall bladders. World Animal Protection states that bear bile farming "causes intense, unjustified suffering to bears”. Chinese officials state that 10,000 wild bears would need to be killed each year to produce as much bile, making bear farming the more desirable option. World Animal Protection, however, states that "it is commonly believed in China that the bile from a wild bear is the most potent, and so farming bears for their bile cannot replace the demand for the product extracted from wild animals".
One alternative to farming involves replacing medical ingredients from threatened species with manufactured chemical compounds. In general, this sort of substitution is difficult to achieve because the active ingredient is often not known. In addition, most TCM users believe that TCM compounds may act synergistically so several ingredients may interact to give the required effect. Thus, TCM users often prefer the wild source. Tauro deoxycholic acid, the active ingredient of bear bile, can be synthesised and is used by some Western doctors to treat gallstones, but many TCM consumers reject it as being inferior to the natural substance from wild animals [4].
Introduction To Industrial Microbiology
Industrial microbiology is a field of microbiology science concerned with the utilization of microorganisms in industrial processes. It deals with all forms of microbiology, which have an economic aspect, and is a relative new science. The industrial use of microbiology had their beginning in large scale food fermentation that produced lactic acid from dairy products and ethanol from brewing. As a science, industrial microbiology is little more than 100 years old; as an art, it dates back into antiquity
Industrial microbiology is a field of microbiology science concerned with the utilization of microorganisms in industrial processes. It deals with all forms of microbiology, which have an economic aspect, and is a relative new science. The industrial use of microbiology had their beginning in large scale food fermentation that produced lactic acid from dairy products and ethanol from brewing. As a science, industrial microbiology is little more than 100 years old; as an art, it dates back into antiquity.
In recent years, industrial microbiology has been revolutionized by the application of genetically engineered organisms. The methods for making engineered (modified) organism using recombinant DNA technology to produce specialized product is known as biotechnology. Commercially valuable product produce by microorganisms include acids(acetic lactic, citric) alcohols (butanol, ethanol) solvents (acetone, glycerol), antibiotics (penicillin, streptomycin, tetracyclines) amino acids (glutamic acid, lysine, valine) vitamins (vitamin B2, vitamin B12), growth factors (gibberellin), hormones (corticosterone), enzymes (amylases, proteases, pectinases, invertase), beverages (beer, wine, spirits), bakers’ yeast etc….
The microbial world comprises of microorganisms, the organisms having microscopic size, but these microscopic organisms have several features that are common to higher organisms, eg: DNA. However, a number of significant differences do set microorganism a part and make them unique. As a group microorganism include bacteria, fungi and microscopic algae. It also includes viruses, sometimes recorded has being the border between living and non-living.
All organisms can be distinguished into two broad groups, the prokaryotes and the eukaryotes. These terms were first proposed in 1937 by Edward chatton. Prokaryotes lack a nucleus whereas eukaryotes pocces a well-defined nucleus. A bacteria cyanobacterium represents prokaryotes whereas fungi, protozoa, plantys and animals are eukaryotes. A comparison of prokaryotes and eukaryotes is presented. The cells of prokaryotes and eukaryotes both have a gel like cytoplasm, but eukaryotes cells have a variety of membrane bound components lacking in prokaryotes. These components are called organelles, which include endoplasmic reticulum, series of membranes extending throughout the cytoplasm; the Golgi bodies a number of flattened sacs packaged before release; the lysosome, a somewhat circular, drop-like sac of digestive enzymes within the cytoplasm; and the mitochondrion, the organelle where much chemical energy is released for cell use. Mitochondria are called as the powerhouses of the cells’. In prokaryotic cells chlorophyll is dissolved in cytoplasm but in eukaryotic microorganisms it is contained in the organelle called the chloroplast. The eukaryotic cells possess yet another organelle called the cytoskeleton, which is an inter connected system of fibres, threads, and interwoven molecule that render structure to the cell. The microtubules, microfilaments, and the inter mediate filaments, all assembled from subunits of protein constitute the main component of cytoskeleton centriole is another organelle, which is cylinder like structure occurring in pairs and functioning in cell division
Both, prokaryotes and eukaryotes possess ribosomes, the ultramicroscopic bodies of RNA and protein where synthesis takes place prokaryotic ribosome (70Sribosome) are smaller than eukaryotic ribosomes (80Sribosome). Prokaryotic ribosomes exist free in the cytoplasm, while eukaryotic ribosomes are usually bound to membranes of the endoplasmic reticulum. Several prokaryotic cells contain organelles called flagella and cilia. Flagella are long and hair like and extend from the cell to permit cell moment. In bacteria the flagella rotate like the propeller of a motor boat. In eukaryotic cells such certain protozoa and sperm cells, the flagella whip about. Cilia are shorter and more numerous than flagella. In moving cells, they wave in synchrony and move the cell forward. Both prokaryotic and eukaryotic cells have their hereditary characteristic stored in molecule of DNA organized in chromosomes.in prokaryotic cells, the chromosome consist of a single DNA molecule in a closed loop, while in eukaryotic cells the DNA occurs in multiple chromosomes arranged in nucleus.
The cell membrane or plasma membrane lies at the surface of all cells and is composed primarily of proteins and lipids, especially phospholipids. Many prokaryotic eukaryotic cells contain cell wall, a structure outside the cell membrane. Almost all bacteria have a thick, rigid cell wall. Amongst the eukaryotes, the algae, the fungi, and plants have cell walls. In fungi, the cell wall contains a polysaccharide called chitin while bacteria possess a different polysaccharide called peptidoglycan. It must be remembered that all living things are either prokaryotic or eukaryotes but viruses are neither since they are not living organisms’ viruses are segments of nucleic acid packaged in a protein shell. They are considered as microorganisms due to their infectious nature [5].
Introduction to Micro organisms
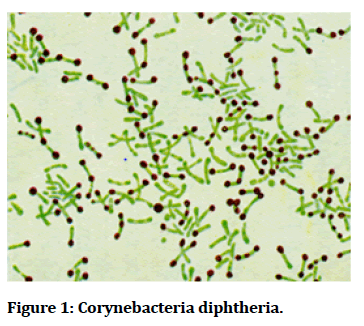
Corynebacteria diphtheria is the pathogenic bacterium that causes diphtheria. It also known as Klebs-Loffler bacillus, because it was discovered in 1884 by German bacteriologists Edwin klebs (1834-1912) and Friedrich Loffler (1852-1915) (Figure 1).
Figure 1: Corynebacteria diphtheria.
Pathogen and disease
Corynebacteria diphtheria is the scientific name for the disease diphtheria. Corynebacteria diphtheria is a rodshaped, gram positive, non-spore- forming, and nonmotile bacterium. Although the geographic occurrence for the disease is world-wide, it mainly found in tropical regions and underdeveloped countries. Those facing the greatest risk of contracting the disease are immune compromised individuals, poorly immunized adults, and unvaccinated children. When an individual contracts diphtheria, the only affected region of the body is the upper respiratory system. Diphtheria can cause a thick grey coating to build up in the throat or nose making it difficult to breathe and swallow. Once individual contracts the disease, they are contagious for two weeks to a month. The portals of entry for Corynebacterium diphtheria are the nose, tonsils, and throat. Diseased individuals may experience a sore throat, overall weakness, fever, and swollen glands. Diphtheria is transmitted from human contact through respiratory droplets, such as coughing or sneezing. Although unlikely, individuals can get sick from touching open sores or clothes that touched open sores of someone sick with the disease. If untreated, the diphtheria toxin can get into the bloodstream causing damage to the kidneys, nerves, and heart. Extremely rare but serious complications include suffocation and partial paralysis. One preventive measure against diphtheria would be to get the D Tap vaccine if available.
Pathogenesis
In areas where diphtheria is endemic, C. diphtheria in the nasopharyngeal passageways is common. The exotoxin of Corynebacterium diphtheria is absorbed in the blood which in turn kills, heart, kidney, and nerve cells by blocking protein synthesis [5]. Toxigenic strains in susceptible individuals can cause disease by multiplying and secreting diphtheria toxin into either skin or nasopharyngeal lesions. The diphtheritic lesion is often covered by a pseudo membrane composed of fibrin, bacteria, and inflammatory cells. Diphtheria toxin can be proteolytically cleaved into two fragments: an N-terminal fragment A (catalytic domain), and fragment B (Tran’s membrane and receptor binding domain). Fragment catalyses the NAD+ -dependent ADP-ribosylation of elongation factor 2, thereby inhibiting protein synthesis in eukaryotic cells. Fragment B binds to the cell surface receptor and facilitates the delivery of fragment A to the cytosol.
Corynebacterium sensitivity
Antibiotics are the treatment of choice for nondiphtheria Corynebacteria infections. Many species and groups are sensitive to various antibiotics, including penicillin’s, macrolide antibiotics, rifampin, and fluoroquinolones. However, antibiotic susceptibility can vary, and susceptibility testing is recommended
Corynebacterium treatment:
The goal is both to kill the organism and to terminate toxin production. Many antibiotics are effective, including penicillin, erythromycin, clindamycin, rifampin, and tetracycline; erythromycin or penicillin is the treatment of choice and is usually given for 14 days. Children who develop diphtheria should be given diphtheria antitoxin and antibiotics, such as erythromycin or penicillin. They should be isolated to avoid exposing others to the disease. About two days after starting antibiotic treatment patients are no longer infectious [6]. For confirmation of diagnosis, health workers should obtain throat cultures from suspect cases. However, treatment should begin without waiting for culture results (Figure 2).
Figure 2: Staphylococcus aureus.
Staphylococcus aureus: It is gram negative bacteria, non-motile, non-spore-forming bacteria.
Catalase: Positive
Oxidase: Negative
Facultatively anaerobic
Treatment: If susceptible: ampicillin/ sulbactam, amoxicillin/clavulanate, oxacillin, nafcillin, Macrolides, clindamycin.
Alternative’s trimethoprim sulfamethoxazole (TMP-SMX), vancomycin.
Disease caused by S. aureus:
S. aureus can cause a range of illnesses, from minor skin infections, such as pimples, impetigo, boils, cellulitis, folliculitis, carbuncles, scalded skin syndrome, and abscesses, to life-threatening diseases such as pneumonia, meningitis, osteomyelitis, endocarditis, toxic shock syndrome, bacteraemia.
Resistance
The problem in clinical medicine despite much research and development there is no approved vaccine for S. aureus. Emergence of antibiotic-resistant strains of S. aureus such as methicillin-resistant S. aureus (MRSA) is a worldwide (Figure 3).
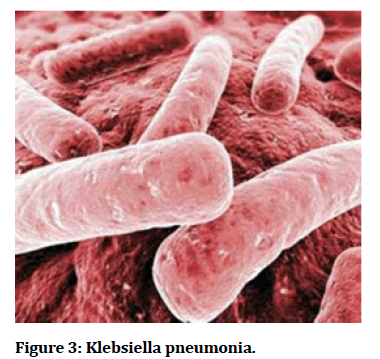
Figure 3: Klebsiella pneumonia.
Klebsiella pneumonia is a gram negative, non-motile encapsulated, lactose, fermenting, facultative anaerobic, rod-shaped bacterium found in the normal flora of intestines. It is clinical the most important member in the Klebsiella genus of enterobacteriaceae.it is naturally occurs in the soil and about 30% of strains can fix nitrogen in aerobic condition.
It occurs in people with weakened immune system, the most of the common infection caused by Klebsiella bacteria is pneumonia resistance it has often resistance to multiple antibiotics. Klebsiella species with the ability to produce extended-spectrum beta lactamases (ESBL) are resistance to virtually all the beta-lactam antibiotics, except carbapenems. Other resistance targets aminoglycosides, fluoroquinolones, tetra clines, chloramphenicol and trimethoprim/sulfamethoxazole.
Treatment
if the specific Klebsiella in a particular patient does not shows antibiotic resistance, then the antibiotics used to treat such as susceptible isolates include ampicillin/ sulbactam, piperacillin/tazobactam, ticarcillin/ clavulanate, ceftazidime, cefepime, levofloxacin, norfloxacin, moxifloxacin, meropenem, ertapenem, ciprofloxacin.
Brucella: is a genus of Gram-negative bacteria, named after David Bruce (1855–1931). They are small (0.5 to 0.7by 0.6 to 1.5 μm), none capsulated, non-motile, Facultatively intracellular coccobacilli. Brucella is the cause of brucellosis, which is a zoonosis transmitted by ingesting contaminated food (such as unpasteurized milk products), direct contact with an infected animal, or inhalation of aerosols. Transmission from human to human, for example through sexual intercourse or from mother to child, is exceedingly rare, but possible. Minimum infectious exposure is between 10 and 100 organisms. The different species of Brucella are genetically very similar, although each has slightly different host specificity. Hence, the NCBI taxonomy includes most Brucella species under B. militancy’s.
The many names of brucellosis include (human disease/ animal disease):
• Malta fever/Bang's disease
• Undulant fever/enzootic abortion
• Mediterranean fever/epizootic abortion
• Rock fever of Gibraltar/slinking of calves
• Gastric fever/ram epididymitis
• Contagious abortion/spontaneous abortion
Characteristics
Brucella species are small, Gram-negative, facultative coccobacilli, most lacking capsule, endospores, or native plasmids.
They are intracellular within the host organism, and show environmental persistence outside the host. The intracellular trafficking includes two to three main steps, starting with endosomal vacuoles, then endoplasmic reticulum-derived compartments and finally vacuoles having several markers of atypical autophagy.
They survive extremes in temperature, pH, and humidity, and in frozen and aborted materials. They infect many species, but with some specificity. The Brucella belongs to the Rhizobia group, in the Alpha proteobacteria class.
They are growing by unipolar growth, like Agrobacterium tumefactions, Sino rhizobium meliloti and Urobacterium anthropic. They usually have two chromosomes and their replication and segregation are temporally organized (Figure 4).
Figure 4: Escherichia coli.
Commonly abbreviated E. coli; named after Theodor Escherichia) is a Gram-negative rod-shaped bacterium that is commonly found in the lower intestine of warmblooded organisms (endotherms). Most E. coli strains are harmless, but some, such as serotype O157:H7, can cause serious food poisoning in humans, and are occasionally responsible for product recalls [1,2]. The harmless strains are part of the normal flora of the gut, and can benefit their hosts by producing vitamin K2, and by preventing the establishment of pathogenic bacteria within the intestine. E. coli are not always confined to the intestine, and their ability to survive for brief periods outside the body makes them an ideal indicator organism to test environmental samples for fecal contamination [7]. The bacteria can also be grown easily and its genetics are comparatively simple and easily manipulated or duplicated through a process of metagenes, making it one of the best-studied prokaryotic model organisms, and an important species in biotechnology and microbiology. E. coli was discovered by German paediatrician and bacteriologist Theodor Escherich in 1885, and is now classified as part of the Enterobacteriaceae family of gamma-proteobacteria (Figure 5).
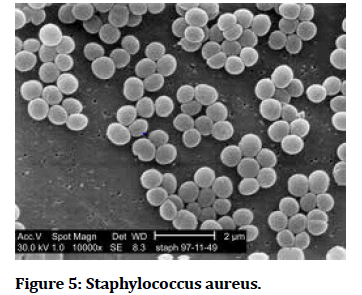
Figure 5:Staphylococcus aureus.
Staphylococcus aureus literally the "golden cluster seed" or "the seed gold" and also known as "golden staph" and Oro staphira) is a facultative anaerobic, Gram-positive coccus, and is the most common cause of staph infections. It is frequently part of the skin flora found in the nose and on skin. About 20% of the human populations are long-term carriers of S. aureus. The carotenoid pigment staphyloxanthin is responsible for its characteristic golden colour, which may be seen in colonies of the organism. This pigment acts as a virulence factor with an antioxidant action that helps the microbe evade death by reactive oxygen species used by the host immune system. Staphylococci which lack the pigment are more easily killed by host defences.
Pathogenesis
S. aureus can cause a range of illnesses from minor skin infections, such as pimples, impetigo, boils (furuncles), cellulitis folliculitis, carbuncles, scalded skin syndrome, and abscesses, to life-threatening diseases such as pneumonia, meningitis, osteomyelitis, endocarditis, toxic shock syndrome (TSS), chest pain, bacteraemia, and sepsis. Its incidence is from skin, soft tissue, respiratory, bone, joint, endovascular to wound infections. It is still one of the five most common causes of nosocomial infections, often causing postsurgical wound infections. Abbreviated to S. aureus or Staph aureus in medical literature, S. aureus should not be confused with the similarly named and similarly dangerous (and also medically relevant) species of the genus Streptococcus. S. aureus was discovered in Aberdeen, Scotland in 1880 by the surgeon Sir Alexander Ogston in pus from surgical abscesses. Each year, some 500,000 patients in American hospitals contract a staphylococcal infection [8].
Review of Literature
India is a varietal emporium of medicinal plant Sandison of their chest countries in the world in regard to genetic resource of medicinal plants. It exhibits a wide range in to pography and climate, which has a bearing on its vegetation and floristic composition. Moreover, the agro climate conditions are conducive for introducing and domesticating new exotic plant varieties. In recent years, secondary plant metabolites (phytochemicals), previously with unknown pharmacological activities, have been extensively investigated as a source of medicinal agents.
Ficus benghalensis Linn. (Syn: Ficusindica: Family: Moraceae), commonly known as Barged grows in tropical and subtropical region of India. Ficus benghalensis has been reported different bioactive compound such as Benghalenosides, Flavonoid’s and Leucocyanidin, Taraxasterol tiglate from heartwood; qucertin-3- galatoside and rutin isolated from leaves. Various scientific studies have been carried out on Benghalensis and various pharmacological activities have been reported. It has been reported to possess immunomodulatory, hypoglycaemic, antioxidant, antistress and anti-allergic and anthelmintic activities. A glucosidal Benghalenosides was isolated from F. Benghalensis and evaluated for hypoglycaemic activity. Efforts are being made all over the world to discover agents that can promote healing and they’re by reduce the cost of hospitalization and save the patient from amputation or other severe complications. The need for safer and effective wound healing agents and the lack of enough scientific data to support the claims made in ancient literature prompted the present study [9]. The aerial root is styptic, aphrodisiac, and useful in gonorrhoea, syphilis, dysentery. In addition, several therapeutic effects have been shown for different parts of Ficus benghalensis such as Anti tumor activity.
On the basis of literature survey, we find may compound isolated from plant Ficus benghalensis Linn some of them are Friedens, beta-sitosterol, Quercetin-3-galactoside, 3,5,7-trimethyl ether of Leucocyanidin, 3,5,7-trimethyl ether of leucocynaidin-3-O-beta-D-glactosylcellobioside, 5,7 dimethyl ether of leucoperlargonidin-3-O-α-Lrhamnoside, Betasitosterol-α-D glucose, 20- tetraiacontene-2-one, 6-heptatriacontene-10-one, pentatriacontene-5-one, Mesoinositol. In the paper we describe the morphological and phytochemical aspects of Ficus benghalensis Linn with the standard drug Silibinin on the basis of Lipinski's rule of five and physiological interpretation by Molinspiration software to explore the Hepato protective activity of this plant.
Botanical review
Ficus benghalensis, large evergreen tree, belongs to the family Moraceae. It is commonly known as “Indian Banyan Tree”. It one among the four sacred trees “Nalpamara” (K Ksirivarkas) meant to be planted around the home and temple. Their ever-extending branch symbolized eternal life, which is why it considered as sacred. The banyan tree also comprises of numerous spiritual and mythological contexts (Figure 6).
Figure 6:Ficus benghalensis.
Background of the study
Taxonomical classification
Distribution
Banyan tree is aboriginal to South Asia especially India, Sri Lanka and Pakistan. It is often being planted around temple and a place of religious importance. It is considered as sacred tree by both Hindus and Buddhists. Banyan tree is widely cultivated in city parks and botanical garden throughout new World and Old-World tropics. It grows well in tropical, semi-tropical regions, monsoon and rain forest with moderate to ample rainfall. Humid air and moist soil and are hardy, drought resistance and withstands mild frost is well suited for its growth.
Morphology
Banyan is a humongous tree, with branches spreading across wide area; it attains a height of about 100 feet tall and, with its massive limbs supported by prop roots, spread over an area of several acres. Its bark is smooth, thick, green when young, greyish white when mature, turning pink when cut, exfoliating in sheaths; wood is soft and porous with milky, sticky latex.
Leaves
Leaves are glossy, leathery and glabrous when mature, approximate hear the end of branches, ovate, mostly obtuse, base cordate or rounded, thickly coriaceous, basal nerves 3-7, the midrib with 4-6 Paris of secondary nerves, blade 10-20 cm long, shoot pubescent, 1.5-2 cm in diameter, sessile, scarlet, red when ripe.
Flowers
It has very small, separate, male and female flowers. The male flowers crowded near the mouth of the receptacle, whereas female flowers with shorter perianth, style long, male and female in the same receptacle.
Fruits
Fruits grobose, sessile in axillary Paris, fleshy pericarp and with achene Sen. trenched in them, they are dark red in colour, 10-2.0 cm diameter, red to dark purple when ripe; seeds are tiny. A fruit is not edible for humans but is eaten by birds and monkeys.
Materials and Methods
Collection of plant materials
The plant Holarrhena anti dysenteric was purchased from the market
Extraction of drug
The dried powdered plant material of Holarrhena antidysentrica was extracted with methanol using soxhlate extraction method. After exhaustive extraction the collected methanolic extract was subjected to evaporation to obtain the pure drug of extract [10].
Continuous extraction
Soxhlet extraction is the process of continuous extraction in which the same solvent can be circulated through the extractor several times. The process involves extraction followed by evaporation of the solvent. The vapours of the solvent are taken to a condenser and the condensed liquid is returned to the drug for continuous extraction.
Soxhlet apparatus designed for such continuous extraction consist of the body of the extractor attached with a side tube and siphon tube as shows in (Figure 7). The extractor from the lower side can be attached to distillation flask and the mouth of the extractor is fixed to a condenser by standard joints. The crude drug powder is packed in the soxhlet apparatus directly or in a thimble of filter paper or fine muslin. The diameter of the thimble corresponds to the internal diameter of the soxhlet extractor.
Figure 7:Soxhlet extractions.
Extraction assembly is set up by fixing a condenser and a distillation flask. Initially for the setting of the powder, the solvent is allowed to pass through siphon once before heating. Fresh activated porcelain pieces are added to flask to avoid bumping of the solvent. The vapours pre ass through the side tube and the condensed liquid gradually increases the level of liquid in the extractor and in the siphon tube. A siphon is set up as the liquid reaches the point of return and the content of the extraction chamber are transferred to the flask. The cycle of solvent evaporation and siphoning back can be continued as many times as possible without changing the solvent, so as to get efficient. This method although a continuous extraction process, is nothing but a series of short macertions [11].
Similar methodology can be adopted in large scale production in which the operation priciples may resemble the laboratory equipment. Soxhlet extraction is advantageous in a way that less solvent is needed for yielding more concentrated products. The extraction can be continued until complete exhaustion of the drug. The main disadvantage is that this process is restricted to pure boiling solvents or to azeotrops (Figure 8).
Figure 8:Preliminary phytochemical screening.
Tests for carbohydrates
Molish’S test (General test)
To 2-3ml. aqueous extract, few drops of alpha napthol solution in alcohol, shake and add concentrate H2SO4 from sides of test tube, violet ring. Violet ring is formed at the junction of two liquids.
Tests for reducing sugars
• Fehling’s test: mix 1ml.fehling’s A and 1ml.B solution heat for 1 min. Add equal volume of test solution. Heat in boiling water bath for 5-10 minute. First a yellow or red ppt is observed.
• Benedict’s test: Mix equal volume of Benedict’s reagent. Heat in boiling water bath for 5 minutes. Solution appears green, yellow or red depending on reducing sugar present in solution
Test for monosaccharide’s
Barfoed’s test:
Mix equal volume of Barfoed’s reagent and test solution. Heat for 1-2 min. in boiling water bath and cool. Red ppt is observed
Test for pentose sugars
Pentoses are components of certain gums
• Bial’s Orcinol Test: To boiling Bial’s reagent add few drops test solution. Green or purple coloration appears
• Aniline Acetate Test: Boil test solution in test tube. Hold filter paper soaked in aniline acetate in the vapour. Filter paper turns pink.
• Mix equal amount of test solution and HCl. Heat. Add a crystal of pholoroglucinol. Red colour appears.
Tests for volatile oils
Hydro disilicate material. Separate volatile oil from distillate and perform the following tests;
• Volatile oils have characteristic odour.
• Filter paper is not permanently stained with volatile oil.
• Solubility test; Volatile oils are soluble in 90% alcohol.
Test for glycosides
Determine free sugar content of the extract. Hydrolyse the extract with mineral acid (dil.HCl\dil.H2SO4) Agar determine the total sugar content of the hydrolyse the extract. Increase in sugar content indicate presence of in the extract Glycoside Aglycon (genin) + Glycon (sugar)
Test for cardiac glycosides
• Baljet’s test: A thick section shows yellow to orange colour with sodium picrate.
• Legal’s test (test for cardenoloids): To aqueous or alcoholic extract, add 1 ml. pyridine and 1 ml. sodium nitro prusside. Pink to red colour appears
• Libermann’s test (test for bufadenoloids): see tests for steroids
Tests for anthraquinone glycosides
• Borntrager’s test for Anthraquinone glycosides: To 3 ml. extract, add dil. H2SO4.Boil and filter. Cold filtrate, add equal volume of benzene or chloroform Shake well. Separate the organic solvent. Add ammonium ammonical layer turns pink to red.
• Modified Borntrager’s test for c- glycosides: To 5 ml. extract add 5 ml. 5% FeCl3 and 5 ml. Diluted HCl. Heat for 5 min in boiling water bath. Cool and add benzene or any organic solvent. Shake well. Separate layers add equal volume of dil. ammonia. Ammonical layer shows pinkish red colour
Tests for saponins glycosides
• Foam test: Shake the drug extract or dry powder vigorously with water. Persistent foam observed.
• Haemolytic test: Add drug extract or dry powder to one drop of blood placed on glass slide haemolytic zone appears.
Tests for cyano genetic glycosides
• Guignard reaction or sodium picrate test: Soak a filter paper strip first in 10% picric acid, then 10% sodium carbonate. Dry In a conical flask place moistened powdered drug. Cork it; place the above filter paper strip in the slit in cork. The filter paper turns brick red or maroon.
• To dry drug powder or extract. Add 3% aqueous mercurous nitrate solution. Metallic mercury forms. • Dip a piece of filter paper in guaiacum resin and moist it with dil. Copper sulphur solution. Expose to freshly cut surface of drug, blue strain is produced.
Tests for coumarin glycosides
• Coumarin glycosides have aromatic odour.
• Alcoholic extract when made alkaline. Shows blue or green fluorescence.
• Take moistened dry powder in test tube. Cover test tube with filter paper soaked in dil. NaOH. Keep in water bath. After sometime expose filter paper to UV light. It shows yellowish-green fluorescence.
Tests for flavonoids
• Shinoda test: To dry powder or extract, add 5 ml. 95% ethanol, few drops HCl and 0.5 g magnesium turnings. Pink colour observed.
• To small quantity of residue, add lead acetate solution. Yellow coloured ppt is formed.
• Addition of increasing amount of sodium hydroxide to the residue shows yellow colouration, which decolourises after addition of acid.
Tests for alkaloids
Evaporate the aqueous, alcoholic and chloroform extracts separately. To residue, add dil. HCl. Shake well and filter. With filtrate, perform following tests:
• Dragendorff’s test: to 2-3 ml. filtrates, add few drops Dragendorff’s reagent. Orange brown ppt is formed.
• Mayer’s test: 2-3 ml. filtrates with few drops Mayer’s reagent gives ppt.
• Hager’s test: 2-3 mi. filtrate with Hager’s reagent gives yellow ppt.
• Wagner’s test: 2-3 ml. filtrates with few drops Wagner’s reagent gives reddish brown ppt.
• Murex ide test for purine alkaloids: To 3-4 ml. test solution, add 3-4 drops of conc. HNO3. Evaporate to dryness. Cool and add 2 drops of NH4OH. Purple colour is observed.
Tests for tannins and phenolic compounds
To 2-3 ml. of aqueous or alcoholic extract. Add few drops of following reagents;
• 5% FeCl3 solution: deep blue- black colour
• Lead acetate solution: White ppt.
• Gelatine solution: White ppt .
• Potassium dichromate: red ppt.
• Acetic acid solution: Red colour solution.
• Dilute HNO3: reddish to yellow colour.
Test for enzymes
Oxidase
• Too few thick sections of drug, add catechol solution. The sections become yellowish brown. Repeat test with other boil sections. Sections do not turn yellowish brown.
• To drug material, add5 ml. water and 1% alcoholic solution of guaicum resin and H2O2. Blue colour is observed.
Peroxidase
• Too few thick sections of drug add catechol solution. After 2 min remove catechol solution. Add H2O2 Section appear pink.
• Repeat test with boiled sections. Colour change not observed.
Catalase
To thick section of drug, add H2O2 oxygen gas evolve
Dehydrogenase
• To thick section of drug add 5ml. cold water. After 5 min. add few drops of triphenyl tetrazolium chloride solution. Sections appear red colour.
• Repeat test with boiled section. Section does not appear red.
• Take thick section of drug add cold water and few drops methylene blue solution. Methylene blue colour disappears.
• Repeat test with boiled section. Methylene blue colour does not change
Nutrient agar composition, preparation and uses
Nutrient agar is a general-purpose nutrient medium used for the cultivation of microbes supporting growth a wide range of non-fastidious organisms, nutrient agar is popular because it can grow types of types bacteria and fungi and contain many nutrients needed for the bacterial growth.
Composition of nutrient agar
0.5% peptone
It is an enzymatic digest of animal protein. Peptone is the principal source of organic nitrogen for the growing bacteria.
0.3%beef extract
It is the water-soluble substances which aid in bacterial growth, such as vitamins, carbohydrates, organic nitrogen and compounds and salts.
1.5% agar
The presence of sodium chloride in nutrient agar maintains a salt concentration in the medium that is similar to the cytoplasm of the microorganisms.
Distilled water
Water is essential for the growth of and reproduction of microorganisms and also provides through the medium which various nutrients can be transported Ph is adjusted to nutria (7.4) at 25ºc.
Preparation of nutrient agar
• Suspend 28gm of nutrient agar powder in 1 liter of distilled water
• Heat this mixture while stirring fully dissolve all components
• Autoclave the dissolved mixture at 121degree for Celsius for 15min
• Once the nutrient agar has been autoclaved allowed it to cool but not solidify
• Pour nutrient agar into each plate and leave plates and the sterile surface until the agar has solidified
. • Replace the lid of each Petri dish and store the plates in a refrigerator.
Uses of nutrient agar
• It is frequently used for isolation and purification of cultures.
• It can also be used as a means for producing the bacterial lawns needed for antibiotic sensitivity testes in actuality, antibiotic sensitivity testing is typically performed and media specially formulated for that purpose.
Bacterial culture preparation
Bacterial culture slants were grown on stationary phase in nutrient agar. A small portion of the culture was introduced into 7-8ml of peptone containing (l% w/v) sterile water. A day-old culture was used for the testing and for determination of each extract.
Assay procedure
The assay procedure was carried out by Cup plate diffusion method. The sterilized molten agar media was poured in to petridishes, and kept aside. Then 1ml of broth culture of bacterial solution was spread over the solid agar plate. By the use of sterile borer small bores were made over the plate and it was filled with test solution, Standard solution and diluting solution respectively for each bacterial plate. Then the plates were kept under incubation for 48 hours at 370C. The Zone was measured using scale in millimetre [12].
Antibacterial activity
The antibacterial activities of the extracts were determined by agar cup plate method. Nutrient agar medium was used for the test. Under aseptic conditions in the laminar air flow chamber nutrient agar medium was dispensed into pre sterilized Petri dishes to yield a uniform depth of 4mm. The media was allowed to solidify.
Results and Discussion
Preliminary phytochemical screening of the aqueous extract of M. concanensis reveals the presence of Alkaloids, Saponins, Carbohydrates, Amino acids, Flavonoids and Glycosides (Table 1-3).
| Name of phyto constituent | Aqueous extract |
|---|---|
| Alkaloids | + + + |
| Carbohydrates | + + |
| Amino acids | + |
| Tannins | - |
| Steroids | + |
| Saponins | + + + |
| Flavonoids | + |
| Glycosides | + |
| Mucilage’s | - |
| Proteins | - |
Table 1: Phytochemical screening.
| S.no | Name of organism | Conc. µg/ml | Zone of inhibition | Amoxicillin | |||
| FBLE | AI | FBBE | AI | ZOD (mm) | |||
| 1 | Escherichia coli | 100 | 10 | 1.2 | 9 | 1.33 | 12 |
| 200 | 13 | 1.23 | 14 | 1.14 | 16 | ||
| 300 | 15 | 1.26 | 16 | 1.18 | 19 | ||
| 2 | K. pneumonia | 100 | 10 | 1.8 | 11 | 1.63 | 18 |
| 200 | 14 | 1.42 | 13 | 1.53 | 20 | ||
| 300 | 17 | 1.23 | 16 | 1.31 | 21 | ||
Table 2: Antibacterial activities.
| S. NO | Organism | Concentration(µg/ml) | Diameter(mm) |
|---|---|---|---|
| 1 | Escherichia coli | 5 | - |
| 10 | 5 | ||
| 15 | 7 | ||
| 20 | 10 | ||
| 2 | Klebsiella pneumonia | 5 | - |
| 10 | 6.6 | ||
| 15 | 9.3 | ||
| 20 | 13.2 |
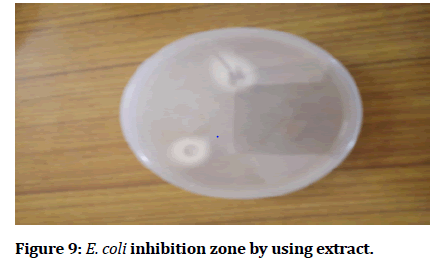
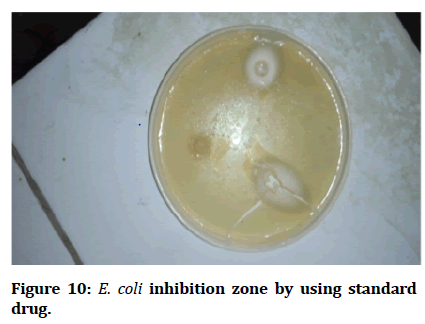
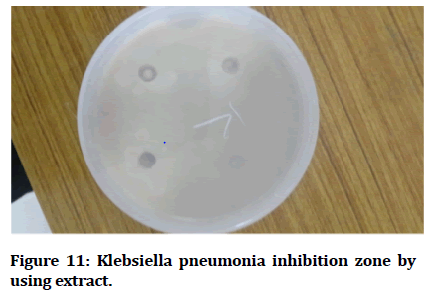
Table 3: Clear pictures of inhibition microbes by using extract and standard drug.
Minimum Inhibitory Concentration of Plant Extract
Different doses of the aqueous extracts were screened for their activity mainly due to the presence of alkaloids and Saponins respectively (Figures 9-14).
Figure 9: E. coli inhibition zone by using extract.
Figure 10: E. coli inhibition zone by using standard drug.
Figure 11: Klebsiella pneumonia inhibition zone by using extract.
Figure 12: Klebsiella pneumonia inhibition zone by using standard.
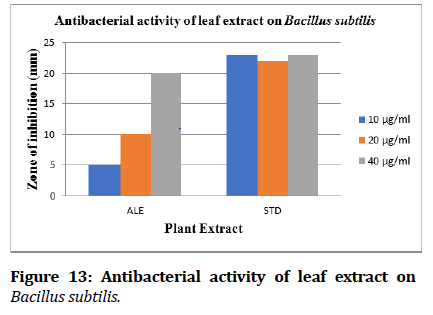
Figure 13: Antibacterial activity of leaf extract on Bacillus subtilis.
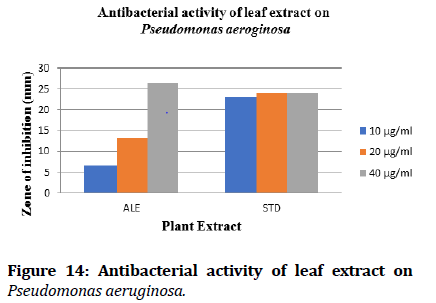
Figure 14: Antibacterial activity of leaf extract on Pseudomonas aeruginosa.
Summary and Conclusion
The plant Moringa concanensis Nimmo was collected from the rural areas of karimnagar. The wet leaves of the plant can be subjected to maceration by using water as a solvent. Then this extraction distilled to get a concentrated mass. Phytochemical investigation was done. The work states that the presence of alkaloids, carbohydrates, glycosides, Saponins and steroids in the extract of Moringa concanensis Nimmo was responsible for its antibacterial activity. These compounds exhibit a maximum zone of inhibition against Pseudomonas aeroginosa and Bacillus subtilis. It is interesting to observe the results of high antibacterial effect of aqueous extract. This study gives the way for further studies should be undertaking to elucidate the exact mechanism of action by which extract exert their antibacterial effect.
References
- Deepak A, Anshu S. Indigenous herbal medicines: Tribal formulations and traditional herbal practices. Jaipur-India: Aavishkar Pub Distrib 2008; 440.
- Anbazhakan S, Dhandapani R, Anandhakumar P, et al. Traditional medicinal knowledge on Moringa concanensis Nimmo of perambalur District, Tamilnadu. Anc sci life 2007; 26:42.
- Sachan D, Jain SK, Singh N. In vitro and In vivo Efficacy of Moringa oleifera plant constituents in urolithiasis as antilithiatic drugs. Int J Pharm Sci Res 2011; 2:1638-44.
- Fredrickson JK, Zachara JM, Balkwill DL, et al. Geomicrobiology of high-level nuclear waste-contaminated vadose sediments at the Hanford Site, Washington State. Appl Environ Microbiol 2004; 70:4230-41.
- Whitman WB, Coleman DC, Wiebe WJ. Prokaryotes: The unseen majority. Proc Nat Acad Sci 1998; 95:6578-83.
- Atlas RM. Principles of microbiology. St. Louis: Mosby 1995.
- Madigan MT. Brock biology of microorganisms. 11th Edn.
- Raymon Lionel P. Comlex level 1 pharmacology lecture notes. Miami, FL: Kaplan.
- https://www.wiley.com/en-in/Biochemistry%2C+4th+Edition-p-9780470570951
- Ng KW, Schantz JT. A manual for primary human cell culture. World Scientific 2010.
- Zhu M, Burman WJ, Jaresko GS, et al. Population pharmacokinetics of intravenous and intramuscular streptomycin in patients with tuberculosis. J Hum Pharm Drug Therap 2001; 21:1037-45.
- https://link.springer.com/book/10.1007/978-94-009-5570-7
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
K Mahammad Areef1* and Mohammed Mazher Ahmed2
1Department of Pharmacy, Dr. K.V. Subba Reddy Institute of Pharmacy, Jawaharlal Nehru Technological University, Anantapur, Andhra Pradesh, India2Department of Pharmaceutics, Luqman College of Pharmacy, Gulbarga, India
Citation: K Mahammad Areef, Mohammed Mazher Ahmed, Antibacterial Activity of Different Leaves and Bark Extracts of Ficus Benghalensis , J Res Med Dent Sci, 2021, 10(1): 242-255
Received: 21-Dec-2021, Manuscript No. JRMDS-21-45222; , Pre QC No. JRMDS-21-45222 (PQ); Editor assigned: 23-Dec-2021, Pre QC No. JRMDS-21-45222 (PQ); Reviewed: 06-Jan-2022, QC No. JRMDS-21-45222; Revised: 10-Jan-2022, Manuscript No. JRMDS-21-45222 (R); Published: 17-Jan-2022