Research - (2022) Volume 10, Issue 8
Antibiotic Susceptibility of Klebsiella pneumoniae Isolated from Various Clinical Samples from a Tertiary Care, Chennai, India
Kiran Madhusudhan and Bindu D*
*Correspondence: Bindu D, Department of Microbiology, Sree Balaji Medical College and Hospital, India, Email:
Abstract
The genus Klebsiella of Enterobacteriaceae family is ubiquitous in nature. They cause many nosocomial and community acquired infections like pneumonia, urinary tract infections, wound infections, bacteremia and septicemia. Multidrug resistance is seen in Klebsiella which serves as the most common cause of increased morbidity and mortality. Klebsiella pneumoniae is major concern as drug resistance has evolved in them to last resort antibiotics. There are many mechanism that brings about the resistance are ESBL, Amp C beta lactamases and carbapenemases. This study aimed to know the prevalence and antibiotic susceptibility of various antibiotics to Klebsiella pneumoniae infections from various samples. This retrospective study was conducted in our tertiary care hospital during the period from January 2022 to May 2022. A total of 573 samples were tested during this period. The samples include blood, sputum, urine, and pus. Out of the 573 total samples tested,104 samples were identified as Klebsiella pneumoniae and the highest rate of isolation of Klebsiella pneumoniae was from wound sample (41.7 %) followed by urine (24.3 %) and also the same was reported high in surgical wards. The study showed male preponderance of Klebsiella pneumoniae when compared to females. The antibiotic sensitivity pattern was done by Kirby-Bauer's disc diffusion method and the sensitivity was noted to be higher to meropenem, imipenem and piperacillin-tazobactam. Thus, this study shows the prevalence rate of Klebsiella pneumoniae and sensitivity pattern of Klebsiella, which may help select appropriate antibiotics and prevent overuse and misuse of antibiotics.
Keywords
Antibiogram, Antibiotic resistance, Klebsiella pneumoniae
Introduction
Klebsiella pneumoniae (K. pneumoniae) is opportunistic gram negative pathogen belonging to Enterobacteriaceae, which causes various infections ranging from Urinary tract infections, bacteremia, wound infections and pneumonia. It causes both hospital-acquired and community-acquired infections [1]. It carries various genes both in chromosome and plasmid that contributes to the antibiotic resistance. Its resistance profile has increased over the past 20 years leading to Multidrug resistant (MDR) and extremely drug resistant organism (XDR). Resistance to the antibiotics is due to the irrational use which has produced ESBLs and Carbapenamases producing K. pneumoniae. Hence the study was aimed to determine the trend of antibiotic profile of K. pneumoniae among the patients attending our tertiary care centre.
Materials and Methods
This is a retrospective study conducted in the Department of Microbiology in a tertiary care, Chennai from January 2022 to May 2022. A total of 573 clinical samples including pus, blood, wound swab, tissue, Bronchoalveolar lavage (BAL), bile, urine, pleural fluid, endotracheal aspirates and blood were collected from different departments (General surgery, General medicine, Obstetrics and Gynaecology, Orthopedics, dermatology, urology, Nephrology, Intensive Care unit (ICU), ) of Sree Balaji Medical College Hospital. Urine, Pus/wound swab, endotracheal aspirate, sputum, BAL, bile, pleural fluid, tissue were inoculated in Nutrient agar, Blood agar and Mac Conkey agar, For Blood primary inoculation in BacT/Alert followed by subculture in Blood agar and Mac Conkey agar. The colonies were isolated and identified by standard test like Gram staining, Catalase, oxidase, Indole, citrate, urease, Triple sugar agar and Mannitol motility agar.
The isolated K. pneumoniae was inoculated in Muller Hinton agar plates following Clinical and Laboratory Standard Institute (CLSI) guidelines [2]. Escherichia coli ATCC 25922 was used as quality control strain.
Results
Among the 573 culture samples from different department, 325 samples were culture positive. 104 (32%) K. pneumoniae were isolated. 56.3% were isolated from male patients and 43.7% were from females. K. pneumoniae was isolated more from Pus/wound sample followed by Urine, sputum as shown in the Table 1. The isolation of K. pneumoniae was (33.5%) highest in 50-60 years age group as shown in Table 2. The isolation was 64.1% in hospitalized patients than outpatients (Table 3). The isolation of K. pneumoniae was high from General surgery department followed by General medicine (Table 4).
| S. No | Sample | Number of Klebsiella pneumoniae | Percentage |
|---|---|---|---|
| 1 | Urine | 25 | 24.30% |
| 2 | Pus/wound sample | 43 | 41.70% |
| 3 | Sputum | 24 | 23.30% |
| 4 | Blood | 1 | 0.97% |
| 5 | Endotracheal aspirate | 3 | 2.90% |
| 6 | Bronchoalveolar lavage | 3 | 2.90% |
| 7 | Tissue | 2 | 1.90% |
| 8 | Bile | 1 | 0.97% |
| 9 | Pleural fluid | 1 | 0.97% |
Table 1: Prevalence of K. pneumoniae in various samples.
| S.No | Age group (years) | No of isolates |
|---|---|---|
| 1 | 20-30 | 05 (4.8%) |
| 2 | 31-40 | 06 (5.8%) |
| 3 | 41-50 | 14 (13.5%) |
| 4 | 51-60 | 35 (33.6%) |
| 5 | 61-70 | 26 (25%) |
| 6 | 71-80 | 18 (17.3%) |
Table 2: Isolation of K. pneumoniae in different age group.
| S.No | Samples from source | Number of isolates |
|---|---|---|
| 1 | Inpatients | 66 (64.1%) |
| 2 | Outpatients | 37 (35.9%) |
Table 3: Frequency of K. pneumoniae in different samples.
| S.No | Department | Number of Klebsiella pneumoniae isolated | % |
|---|---|---|---|
| 1 | General surgery | 38 | 36.89 |
| 2 | General Medicine | 22 | 21.35 |
| 3 | Nephrology | 3 | 2.91 |
| 4 | Urology | 4 | |
| 5 | Respiratory medicine | 17 | 16.5 |
| 6 | Obestetrics and Gynecology | 2 | 1.94 |
| 7 | ICU | 11 | 10.67 |
| 8 | Dermatology | 1 | 0.97 |
| 9 | Orthopedics | 5 | 4.85 |
Table 4: Isolation of Klebsiella pneumoniae in different wards.
Antibiotic susceptibility of K. pneumoniae
The susceptibility pattern of K. pneumoniae isolates is shown in the Figure1. Thse K. pneumoniae isolates were least resistant to piperacillin-tazobactam (29.1%), Imipenam (33.3%), Meropenam (24.2%), Ciprofloxacin (33%), Gentamicin (33%). All the isolates were resistant to ampicillin. About 46.6% of the isolates were ESBL producers.
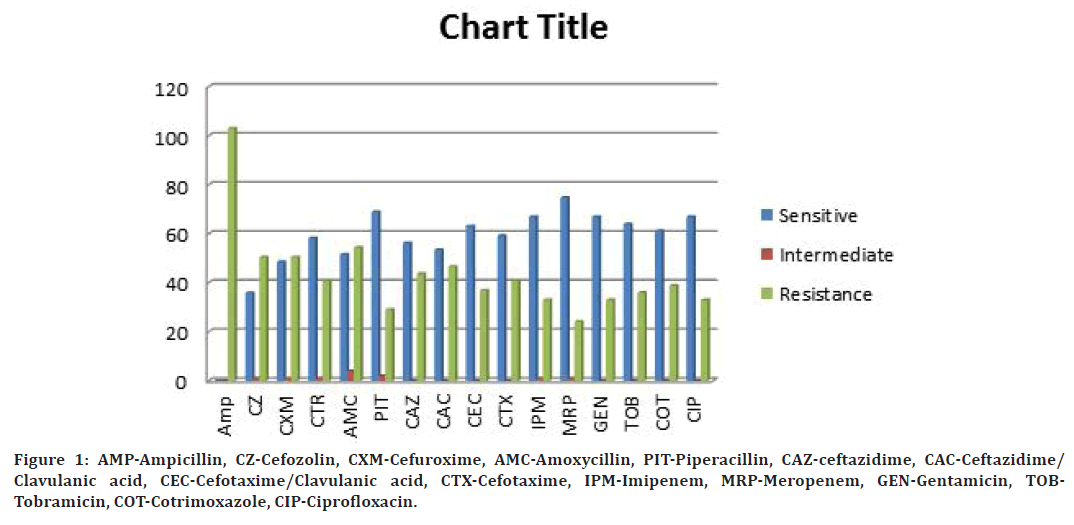
Figure 1. AMP-Ampicillin, CZ-Cefozolin, CXM-Cefuroxime, AMC-Amoxycillin, PIT-Piperacillin, CAZ-ceftazidime, CAC-Ceftazidime/ Clavulanic acid, CEC-Cefotaxime/Clavulanic acid, CTX-Cefotaxime, IPM-Imipenem, MRP-Meropenem, GEN-Gentamicin, TOBTobramicin, COT-Cotrimoxazole, CIP-Ciprofloxacin.
Discussion
Klebsiella pneumoniae is one of major species in Enterobacteiceae family casing infections in both immunocompetent and immunocompromised patients. It causes infections in elderly people which are shown in our study. The total number of Klebsiella isolates from various clinical samples in this study is 104 (32 %). It is similar to the isolation rate seen in the studies [3-5].
In this study, Klebsiella species were isolated more from males compared to females. This study is similar to the work conducted by Anu sharma, et al. [6] (males 57% and females 42%).
In our study the prevalence of K. pneumoniae was more in age group 51-60, followed by 60-70 age group which is similar to study by Sharanya, et al. [6] Susethira, et al. [7] but in contrast to the study by In this study, K. pneumoniae were isolated more from inpatients and from surgery wards, which is similar to study by Anu sharma, et al. [6] which showed that these infections are nosc.
Conclusion
In this present study, K. pneumoniae was isolated from Pus followed by urine similar to study by Anu sharma, et al. 46.7% were found to be ESBL producers.
In this K. pneumoniae was the predominant isolate from various samples. IT was isolated more from inpatients and from surgical wards. In this study, multidrug resistant isolates were found. Hence the it is important formulate antibiotic stedwardship programme. Constant mointoring of the infection control policies is necessary to combat the antibiotic resistance.
References
- Gorrie CL, Mirčeta M, Wick RR, et al. Gastrointestinal carriage is a major reservoir of Klebsiella pneumoniae infection in intensive care patients. Clin Infect Dis 2017; 65:208-215.
- Humphries R, Bobenchik AM, Hindler JA, et al. Overview of changes to the clinical and laboratory standards institute performance standards for antimicrobial susceptibility testing, M100. J Clin Microbiol 2021; 59:e00213-221.
- Shilpakar A, Ansari M, Rai KR, et al. Prevalence of multidrug-resistant and extended-spectrum beta-lactamase producing gram-negative isolates from clinical samples in a tertiary care hospital of Nepal. Trop Med Health 2021; 49:23.
- Vivas R, Dolabella SS, Barbosa AAT, et al. Prevalence of Klebsiella pneumoniae carbapenemase—and New Delhi metallo-beta-lactamase-positive K. pneumoniae in Sergipe, Brazil, and combination therapy as a potential treatment option. Rev Soc Bras Med Trop 2020; 53:e20200064.
- Pyakurel S, Ansari M, Kattel S, et al. Prevalence of carbapenemase-producing Klebsiella pneumoniae at a tertiary care hospital in Kathmandu, Nepal. Tropical Med Health 2021; 49:1-8.
- Krishnasamy L, Saikumar C, Kumaramanickavel G. Aerobic bacterial pathogens causing vaginitis in patients attending a tertiary care hospital and their antibiotic susceptibility pattern. J Pure Appl Microbiol 2019; 13:1169-1174.
- Susethira AR, Uma A. Prevalence of Klebsiella bacteriuria and antimicrobial susceptibility in a tertiary care hospital, Tiruchirapalli, India. Int J Pharma and Clin Res 2016; 8:538-542.
- Sharanya K, Cugati S, Saikumar C. Prevalence and Antibiotic susceptibility pattern among Klebsiella isolates from patients attending a tertiary care hospital. Indian J Microbiol Res 2018; 5:208-212.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Kiran Madhusudhan and Bindu D*
Department of Microbiology, Sree Balaji Medical College and Hospital, Chrompet, Chennai, IndiaReceived: 27-Jul-2022, Manuscript No. jrmds-22-70493; , Pre QC No. jrmds-22-70493(PQ); Editor assigned: 29-Jul-2022, Pre QC No. jrmds-22-70493(PQ); Reviewed: 12-Aug-2022, QC No. jrmds-22-70493(Q); Revised: 17-Aug-2022, Manuscript No. jrmds-22-70493(R); Published: 24-Aug-2022
