Research - (2021) Volume 9, Issue 6
Apical Peri-Implantitis: Etiology, Prevention, Diagnosis, Treatment: Literature Review and Case Report
Sofia Zarenti1*, Genovefa Tsompani1, Menelaos Anastasopoulos1, Thomas Gousoulis1 and Aikaterini-Elisavet Doufexi1,2
*Correspondence: Sofia Zarenti, Department of Preventive Dentistry, Periodontology and Implant Biology, School of Dentistry,, Aristotle University of Thessaloniki, Greece, Email:
Abstract
Nowadays dental implants play a major role in mouth rehabilitation. Retrograde peri- implantitis is defined as a lesion at the periapical area of an osseointegrated dental implant. It can be attributed to preoperative or intraoperative factors, such as infection agents, poor surgical technique, – overheating of the bone, overloading of the implant or it can emanate from an active infection of adjacent teeth. The peri-implant lesion can be diagnosed radiographically as a radiolucent area and clinically as an erythematous, edematous area with or without pyorrhea at the apical region of the dental implant. The purpose of this review is to present the etiology of retrograde peri- implantitis, its prevention, proper diagnosis, and treatment strategies. Moreover, this review introduces a treatment protocol, including a conservative approach, different surgical approaches and supplementary local or systemic delivery of antibiotics. Prevention is strongly linked to etiology and can minimize the possibility of retrograde peri-implantitis. Although, the surgical treatment of retrograde periimplantitis is usually successful, the best treatment approach is the prevention of the disease or even early diagnosis.
Keywords
Apical peri-implantitis, Periapical peri-implantitis, Retrograde peri-implantitis, Apical periimplantitis treatment, Peri-implant infectionIntroduction
Nowadays the use of dental implants is one of the most common treatment options for missing teeth. In addition, the advancements in the specialty of Endodontics have led to an increase in the success rate of Endodontic treatment. However, there are still cases of failed endodontic treatment that endanger dental implants in the periapical region. Apical retrograde peri-implantitis is the inflammation that occurs in the apical peri-implant region, causing dental implant failure or loss of osseointegration [1]. If peri-implantitis remains untreated, it can lead implant loss. Apical peri-implantitis is divided in two categories: active and inactive. Pain, redness, and swelling are indicative signs of the disease [2-6]. The symptoms combined with the radiographic image determine the diagnosis [5-7]. The etiopathogenesis is known and consists of infectious and traumatic causes that also indicate the appropriate treatment [1,4,8,9]. The purpose of this literature review is to investigate and cite the cause and predisposing factors as well as to analyse the diagnosis and treatment for apical retrograde periimplantitis.
Materials and Methods
PubMed, Cochrane and Scopus databases were searched up to December of 2020. A manual search of recently published journals was also conducted. The keywords used were the following: apical peri-implantitis, periapical implantitis, retrograde peri-implantitis. The screening included only papers in English language.
Etiology
Apical retrograde peri-implantitis can be associated with an infection in the vicinity of the dental implant or may be the result of an injury, or mishandling intraoperatively and postoperatively when a dental implant is placed. Specifically, and for the needs of clarifying the etiological approach of the disease, two major categories emerge.
The first category includes the causes of traumatic etiology which can happen intraoperatively or postoperatively. Intraoperatively, overheating of bone, excessive tapping of the implant and the placement of a shorter implant in a deeper prepared site [1,8]. Postoperatively, early loading of the implant, as well as the delay of osseointegration due to poor bone quality are also etiologic factors. Moreover, the placement of an implant in patients with osteomyelitis is also mentioned in the literature [9].
The second category includes two major subcategories concerning the presence or absence of adjacent teeth with active or inactive periapical lesions. Thus, regardless of adjacent teeth with perioapical pathology, apical periimplantitis can be caused by contamination of the implant surface during placement by microbes in the oral environment, the presence of residual roots, cysts, granulomatous tissue as well as any foreign bodies at the site [4]. Furthermore, cases of adjacent teeth with pulp necrosis, adjacent to a dental implant can trigger a periapical inflammation [4]. Research has shown that endodontic complications in adjacent teeth can occur simultaneously with the placement of an implant or delayed due to reactivation of an inactive periapical lesion, or pulp necrosis [10]. More precisely, either there is a pre-existing lesion of the adjacent tooth, which successively spreads to the implant, or there is a simultaneous damage in both the tooth and implant. Histologically, there are four different types of tissue that can trigger an apical lesion: granulomatous tissue, tissue from endodontic infection that extends radically-outside the root canal, true cystic fibrosis, and scar tissue [9]. Histopathologically, apical retrograde peri-implantitis involves cyst formation or chronic inflammation. In addition, such lesions have been shown to include microorganisms of chronic inflammation or cysts, such as Porphyromonas gingivalis, streptococcus and Corynebacterium [9,10]. Microbiological findings from various studies have suggested the association of apical retrograde peri-implantitis with the enterobacterium K. Pneumoniae, streptococci and Corynebacterium [11,12]. Finally, a study conducted by Lefever et al. showed the predominance of anaerobic versus aerobic bacteria [11].
Prevention
The prevention of retrograde peri-implantitis is inextricably linked to its etiology. The clinician must be extremely careful after tooth extraction to meticulously remove any cyst or granulomatous tissue. In addition, a preoperative examination -clinical and radiographic- and the prevention of damage to adjacent teeth significantly reduces the chances of apical peri-implantitis. More specifically, cavity treatments (from caries) of varying extent in adjacent teeth, pulp-necrosis, external absorption and failed endodontic treatments that require repetition should precede the placement of the implants. On the same basis, ill-fitting prosthetic restorations, dentures and dentin exposed areas that could potentially cause necrosis of the respective tooth must be restored as part of prevention. Furthermore, an essential preventative measure is the irrigation of saline during drilling to prevent overheating of the bone-causing ischemia and necrosis. In addition, the precise determination of the implant length is important, (using panoramic radiography, periapical X-rays or cone beam computed tomography), to avoid the placement of a shorter. Last but not least, it is crucial to maintain a sterile surgical field during the operation [1,8]. Table 1 summarizes the association between periimplantitis’ cause and its prevention.
| Etiology | Prevention |
|---|---|
| Α. Traumatic cause | Α |
| 1.Overheating of the bone during drilling | 1.Continuous saline irrigation during drilling |
| 2. Excessive screwing of the implant | 2.Exercise of predetermined force |
| 3. Shorter implant in a deeper shaft | 3. Accurate determination of implant length before drilling |
| 4.Early loading or overloading of the implant | 4. Avoid premature implant loading |
| B. Infectious cause | Β |
| 1.Contamination of the implant surface during placement | 1.Reduction of microbial load preoperatively |
| 2.Residues of roots, cysts, granulomatous tissue, foreign bodies in the area of implant placement | 2.Careful scraping after extraction of a tooth with root inflammation and meticulous removal of septic residues |
| 3.Presence of neighboring necrotic teeth, teeth with active or inactive apical lesions incomplete endodontic treatments | 3.Clinical and radiographic examination with elimination of any inflammation before implant placement |
| 4.Neighboring teeth with untreated periodontal inflammation | 4. Reduction of active inflammatory cyst with surgical or non-periodontal treatment and frequent re-examinations with measurements of gingival depth, clinical level of adhesion and bleeding during detection |
| 5. Neighboring teeth vital with extensive damage or caries | 5. Clinical and radiographic examination, restorative work and prevention of caries lesions |
Table 1: Correlation between etiology and prevention of retrograde periimplantitis.
Diagnosis
Proper diagnosis is the key to the success, and the first step to the proper management of any disease. Apical retrograde peri-implantitis, usually appears with clinical signs of inflammation in the implant, such as pain, redness, tenderness, or the presence of fistula [2-6]. The latter was found to be the most common in the maxilla. In addition, there is a high chance that the formation of the fistula is associated with an apical lesion of the replaced tooth [5]. Regarding pain, there is a correlation with the pathology of the extracted tooth (46%), while it is rarely reported in cases where the adjacent tooth is responsible (7.8%) [5]. A key factor for the differential diagnosis is the history of the tooth, which was removed to place the implant, i.e. if it had a preexisting apical lesion, as well as if the post extraction socket was scraped and disinfected immediately after extraction [3,5,13,14]. Radiographic imaging is important, and in all cases of apical periimplantitis a radiolucent lesion is detected radiographically in the apical region of the implant. Such a finding, in addition to the diagnosis of the disease, will help to determine the etiology (e.g., detection of an apical lesion in the adjacent tooth, responsible for the presence of the microbial load in the area) and consequently in the selection of the initial treatment of the disease -this follows the safe protocol (diagnosis-cause-treatment) for the correct management [5,7]. This process is sometimes challenging. Cases have been reported in which even an asymptomatic, well-treated endodontic tooth was the cause. This is possible since even if there is no radiographic evidence, an infectious microorganism may remain, resulting in a chronic inflammation which in turn can affect the implant [5].
Differential diagnosis is a key station in the evaluation of findings [5,7]. Radiographic examination of the periapical area is especially important for diagnosis, since the disease might be asymptomatic. Since clinical manifestations may be absent (in 16% of cases) in an asymptomatic implant, it is of key significance to correctly assess the apical lesion. An apical peri-impant lesion might be a result of longer preparation of an implant site and placement of a shorter implant or a result of osseonecrosis. In any case a postoperative evaluation is suggested [2-5].
The time of diagnosis varies and affects success and survival of the implant [5,7]. According to research, if symptoms of reversable peri-implantitis appear early, the success rate of the implants is increased. The average time of diagnosis is estimated at 26 weeks after dental implant placement with no significant differences between symptomatic and asymptomatic cases [5]. However, there are conditions that have been recorded, which significantly disrupt this schedule. An important factor that influences the time of diagnosis is the formation of fistula, which can delay the diagnosis by approximately 7 weeks. On the contrary, dental implant mobility due to apical peri-implantitis greatly affects the time of diagnosis by shifting it to approximately 6 weeks [5,15]. Based on the above information a proposed diagnostic model is outlined in the following sequence
A detailed medical and dental history to determine the condition of the replaced tooth as well as the patient's complaints (e.g., Pain).
Clinical examination for any symptoms such as fistula, redness, swelling and edema.
Radiographic examination to detect bone resorption in the peripheral area of the implant or in the adjacent tooth.
From the above, the cause and the risk factors are identified, leading to the diagnosis:
Infectious apical peri-implantitis due to endodontic pathology of the adjacent tooth or extracted tooth or fracture of the root of the adjacent tooth.
Traumatic apical peri-implantitis due to overheating or over-compression of the bone during drilling for implant placement, or reduced bone healing (osseointegration).
Acute retrograde peri-implantitis caused by other etiological or predisposing factors such as placement of the implant very close to the adjacent tooth, which might compromise vascularization of the tooth, vitality of the tooth and consequently possible apical peri-implantitis [5,13].
Treatment
Once reversible peri-implant is diagnosed, the appropriate treatment approach is chosen. A primary distinction of treatment choice lies between non-surgical, surgical, and of course the choice of implant extraction [1,5,6,16-21]. The first is recommended:
Non-surgical
Dental implants that have only radiographic evidence of periapical damage with lack of clinical signs and symptoms while the adjacent tooth is responsible for it. In these cases, endodontic treatment of the tooth should be done, with or without the simultaneous administration of antibiotics. Afterwards, the patient enters a re-examination program for 14 months to evaluate the course of the lesion [5,22].
Asymptomatic dental implants without suspected endodontic pathology in the adjacent tooth. It is recommended to administer antibiotics for 10 days (Amoxicillin 500mg/3 times daily) and the patient enters a re-examination program for a year [3,5].
Surgical
The standard procedure starts with the elevation of a full thickness flap, removal of the granulomatous tissue, disinfection of the affected area and the surface of the implant, repositioning of the flap and suturing [5,6,15,18,19,23-27]. Regarding the regeneration attempt of the peri-implant lesions, in about half of the cases, mainly in maxillary implants, an attempt can be made for directed bone regeneration by placement of regenerative materials such as xenograft and / or allograft and / or autograft with or without collagen membrane [2,5,18,24,28,29]. The same percentage was recorded for the number of cases where the surface of the implant was disinfected, using chlorhexidine solution or tetracycline paste, throughout the operation [3,5,23,24,30]. Finally, only a few treatment approaches (approximately 14%) were completed with the implant apicoectomy [3,5]. In all cases, postoperative treatment with antibiotics (amoxicillin, metronidazole, or a combination of both) was followed. Patients underwent a re-examination program (27 weeks in those who underwent only surgical cleansing and 18 weeks in those who had a graft) [5]. The affected implants did not lose osseointegration and returned to full function within up to 20 months [3,5,15-17,19,20,31-33].
According to the forementioned classification of treatment approaches the main place in the quiver of treating physicians was occupied by the extraction of the affected implant and in fact in a significant percentage (approximately 35%). The data shows that this treatment approach was chosen mainly when the implant was mobile ignoring the cause of the implant mobility. A subsequent study reveals a positive correlation between implant extraction and endodontic pathology in the adjacent tooth, which was found in 53% of cases [5]. Also, a noteworthy overwhelming difference is observed between the extracted maxillary and mandibular dental implants, with the latter reaching 67% of cases [5,7].
Figure 1 presents a suggested decision-making protocol based on the review of the current evidence.
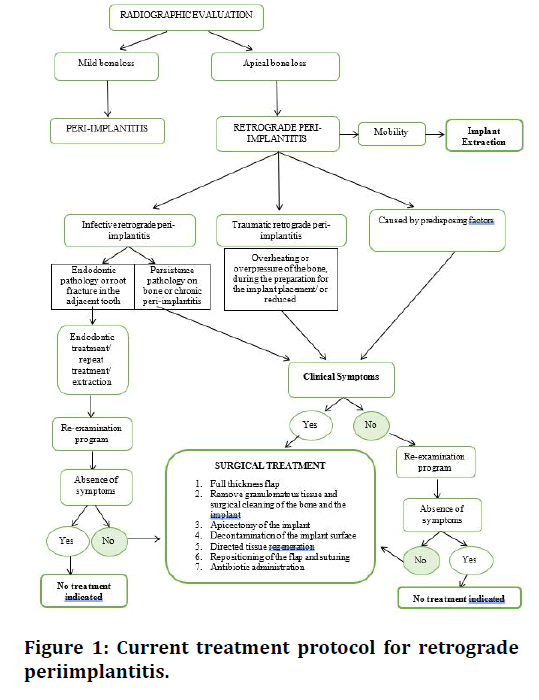
Figure 1. Current treatment protocol for retrograde periimplantitis.
Case Report
A 45-year-old woman, systematically healthy, smoker (10 cigarettes a day for 20 years) presented with severe pain, swelling, and suppuration in the periapical area of #21. Tooth # 21 was endodontically treated and had an apicoectomy due to failure of endodontic treatment (Figure 2A).
The patient was scheduled for extraction of tooth # 21 and dental implant placement 3 months after extraction.
During the extraction of the tooth, granulomatous tissue was removed from the post extraction socket and the area was disinfected with saline. After the tooth was extracted, a collagen sponge and sutures were placed.
3 months after the extraction, a full-thickness flap was elevated a dental implant was placed in area # 21, flaps were repositioned, and primary closure was achieved (Figure 2B).
4 months later the patient presented with edema and suppuration n the periapical area of the implant. Radiographic examination confirmed the clinical diagnosis of retrograde apical peri-implantitis (Figure 2C, D).
The patient was scheduled for surgical treatment. After full thickness flap was elevated, the periapical lesion and the surrounding granulomatous tissues were removed. The implant surface was then disinfected with saline and bone regeneration procedure was performed with allograft and collagen membrane. Finally, the flap was repositioned and sutured (Figure 2e).
4 months later, the implant was uncovered and then prosthetically restored (Figure 2 F, G).
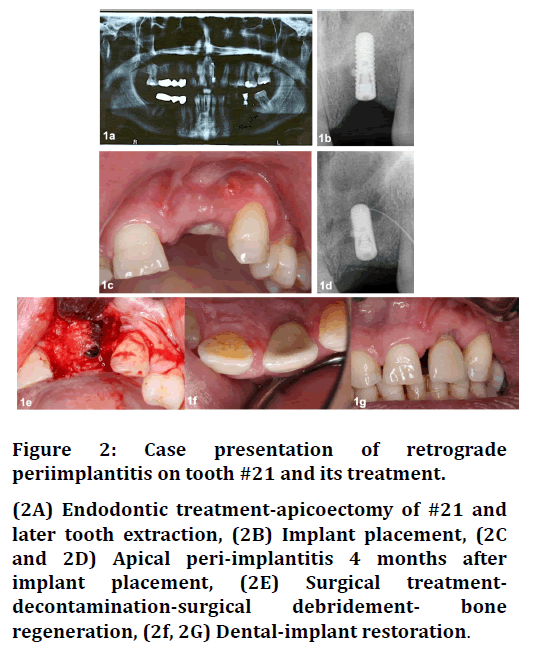
Figure 2. Case presentation of retrograde periimplantitis on tooth #21 and its treatment.
(2A) Endodontic treatment-apicoectomy of #21 and later tooth extraction, (2B) Implant placement, (2C and 2D) Apical peri-implantitis 4 months after implant placement, (2E) Surgical treatmentdecontamination-surgical debridement- bone regeneration, (2f, 2G) Dental-implant restoration.
Conclusion
Apical retrograde peri-implantitis, is a frequent implication of dental implant placement. Given the dubious results of the treatment, the clinician should be aware for both the prevention, correct diagnosis, and treatment of the disease. Re-evaluation exams are also an important to prevent possible recurrences of the disease.
References
- Chan HL, Wang HL, Bashutski JD, et al. Retrograde peri-implantitis: A case report introducing an approach to its management. J Periodont 2011; 82:1080–1088.
- Ayangco L, Sheridan PJ. Development and treatment of retrograde peri-implantitis involving a site with a history of failed endodontic and apicoectomy procedures: A series of reports. Int J Oral Maxillofac Implants 2001; 16:412–417.
- Dahlin C, Nikfarid H, Alsén B, et al. Apical peri-implantitis: Possible predisposing factors, case reports, and surgical treatment suggestions. Clin Implant Dent Related Res 2009; 11:222–7.
- Quirynen M, Vogels R, Alsaadi G, et al. Predisposing conditions for retrograde peri-implantitis, and treatment suggestions. Clin Oral Implants Res 2005; 16:599–608.
- Ramanauskaite A, Juodzbalys G, Tözüm TF. Apical/retrograde periimplantitis/implant periapical lesion. Implant Dent 2016; 25:684–697.
- Tözüm TF, Erdal C, Saygun I. Treatment of periapical dental implant pathology with guided bone regeneration. Turkish J Med Sci 2006; 36:191-196.
- Renvert S, Hirooka H, Polyzois I, et al. Diagnosis and non‐surgical treatment of peri‐implant diseases and maintenance care of patients with dental implants – Consensus report of working group 3. Int Dent J 2019; 69:12–17.
- Nair PNR. On the causes of persistent apical periodontitis: A review. Int Endod J 2006; 39:249–81.
- Marshall G, Canullo L, Logan RM, et al. Histopathological and microbiological findings associated with retrograde peri-implantitis of extra-radicular endodontic origin: A systematic and critical review. Int J Oral Maxillofac Surg 2019; 48:1475–1484.
- Shaffer MD, Juruaz DA, Haggerty PC. The effect of periradicular endodontic pathosis on the apical region of adjacent implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1998; 86:578–81.
- Lefever D, van Assche N, Temmerman A, et al. Aetiology, microbiology and therapy of periapical lesions around oral implants: A retrospective analysis. J Clin Periodontol 2013; 40:296–302.
- Qu C, Meng H, Han J. Implant periapical lesion-a review and a case report with histological evaluation. Clin Oral Implant Res 2014; 25:1099–104.
- Peñarrocha-Oltra D, Blaya-Tárraga JA, Menéndez-Nieto I, et al. Factors associated with early apical peri-implantitis: A retrospective study covering a 20-year period. Int J Oral Implantol 2020; 13:65–73.
- Sarmast ND, Wang HH, Sajadi AS, et al. Classification and clinical management of retrograde peri-implantitis associated with apical periodontitis: A proposed classification system and case report. J Endod 2017; 43:1921–1924.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. J Clin Epidemiol 2009; 62:1006–1012.
- Esfahrood ZR, Kadkhodazadeh M, Amid R, et al. Is the periapical lesion a risk for periimplantitis? A review. J Dent 2012; 9:162–73.
- Peñarrocha Diago M, Boronat López A, Lamas Pelayo J. Update in dental implant periapical surgery. Med Oral Patol 2006; 11:E429-32.
- Reiser GM, Nevins M. The implant periapical lesion: etiology, prevention, and treatment. Compend Contin Educ Dent 1995; 16:768-772.
- Sussman HI. Periapical implant pathology. J Oral Implantol 1998; 24:133-138.
- Zhou W, Han C, Li D, et al. Endodontic treatment of teeth induces retrograde peri-implantitis. Clin Oral Implants Res 2009; 20:1326–32.
- Piattelli A, Scarano A, Balleri P, et al. Clinical and histologic evaluation of an active “implant periapical lesion”: A case report. Int J Oral Maxillofac Implant 1998; 13:713–716.
- Oh TJ, Yoon J, Wang HL. Management of the implant periapical lesion: A case report. Implant Dent 2003; 12:41–46.
- Ataullah K, Chee LF, Peng LL, et al. Management of retrograde peri-implantitis: A clinical case report. J Oral Implant 2006; 32:308–312.
- Brisman DL, Brisman AS, Moses MS. Implant failures associated with asymptomatic endodontically treated teeth. J Am Dent Assoc 2001; 132:191–195.
- Mohamed JB. The management of retrograde peri-implantitis: A case report. J Clin Diagnostic Res 2012; 32:308-312.
- Tseng CC, Chen YHM, Pang IC, et al. Peri-implant pathology caused by periapical lesion of an adjacent natural tooth: A case report. Int J Oral Maxillofac Implant 2005; 20:632–635.
- Waasdorp J, Reynolds M. Nonsurgical treatment of retrograde peri-implantitis: A case report. Int J Oral Maxillofac Implant 2010; 25:831–833.
- Park SH, Sorensen W, Wang HL. Management and prevention of retrograde peri-implant infection from retained root tips: Two case reports. Int J Periodont Restorative Dent 2004; 24:422–433.
- Tözüm TF, Şençimen M, Ortakogˇlu K, et al. Diagnosis and treatment of a large periapical implant lesion associated with adjacent natural tooth: A case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2006; 101:e132–e138.
- Scarano A, di Domizio P, Petrone G, et al. Implant periapical lesion: A clinical and histologic case report. J Oral Implantol 2000; 26:109-113.
- Bretz WAG, Matuck AN, de Oliveira G, et al. Treatment of retrograde peri-implantitis: Clinical report. Implant Dent 1997; 6:287-290.
- Flanagan D. Apical (Retrograde) Peri-implantitis: A case report of an active lesion. J Oral Implant 2002; 28:92–96.
- Sussman HI. Endodontic pathology leading to implant failure-A case report. J Oral Implantol 1997; 23:112–115.
Author Info
Sofia Zarenti1*, Genovefa Tsompani1, Menelaos Anastasopoulos1, Thomas Gousoulis1 and Aikaterini-Elisavet Doufexi1,2
1Department of Preventive Dentistry, Periodontology and Implant Biology, School of Dentistry,, Aristotle University of Thessaloniki, Greece2Private Practice limited to Periodontics, Thessaloniki, Greece
Citation: Sofia Zarenti, Genovefa Tsompani, Menelaos Anastasopoulos, Thomas Gousoulis, Aikaterini-Elisavet Doufexi, Apical Peri- Implantitis: Etiology, Prevention, Diagnosis, Treatment: Literature Review and Case Report, J Res Med Dent Sci, 2021, 9(6): 1-6
Received: 22-May-2021 Accepted: 09-Jun-2021
