Research Article - (2021) Volume 9, Issue 12
Assess The Effectiveness of Deep Breathing Exercise with Incentive Spirometer on the Respiratory status of Cardio Thoracic and Vascular Patients
*Correspondence: AR. Bharathi, Department of Nursing, Bharath Institute of Higher Education and Research, Selaiyur, Chennai-600073 Tamil Nadu, India, Email:
Abstract
Incentive spirometer (IS) is a device which inspires the patients to take a deep breath and produce a sustained maximal inspiration for the primary purpose of opening and stabilizing atelectasis areas of the lung. IS is essential to the thoracotomy patients by increasing inspiratory capacity and improves inspiratory muscle strength in patients. IS is designed to mimic natural sighing or yawning by encouraging the patient to take long, slow, deep breaths. People living with chronic lung diseases, such as chronic obstructive pulmonary disease (COPD), COVID 19, emphysema and pulmonary fibrosis, experience similar lung disease symptoms. Shortness of breath and decreased lung function make breathing difficult. Dysfunctions of the breathing pattern can be first indicators of a problem within the human body, be it of mechanical, physiological or mental kind. Incorrect breathing can be caused by blocked ribs or vertebra, dysfunction of breathing and stabilising muscles, allergies, lung diseases, heart failures and above all excessive stress.The Present study focuses on to assess the effectiveness of deep breathing exercise with incentive spirometer on the respiratory status of patients who have undergone cardio thoracic and vascular surgery during post test. There is no significant association between the effectiveness of deep breathing exercise with incentive spirometer on respiratory status of patients who have undergone cardio thoracic and vascular surgery and demographic variables.Keywords
Assess, Effectiveness, Incentive Spirometer, Deep Breathing Exercise, Respiratory Status, Vascular surgeryIntroduction
Incentive spirometry is a device which helps in the improvement of lung function. It motivates the patients by giving visual feedback about their lung volumes1. It is one of the less expensive and user friendly device3. Incentive spirometry facilitates the patients to take slow deep breathe and there by producing a Sustained Maximal Inspiration (SMI) that mainly helps in the prevention of atelectasis. Cardiovascular diseases (CVDs) have now become the leading cause of mortality in India The Global Burden of Disease study estimate of age-standardized CVD death rate of 272 per 100000 population in India is higher than the global average of 235 per 100000 population [1]. Cardiovascular Outcomes after Acute Coronary Syndrome are unpredictable.
Cardiac surgeries are associated with an occurrence of postoperative pulmonary complications (PPC), defined as any pulmonary abnormality that occurs during the postoperative period which produces identifiable disease or dysfunction that is clinically significant, and which adversely affects the clinical course. Patients undergoing coronary artery bypass grafting are at increased risk of pulmonary complications.. The incidence is between 30% and 60%. These complications are the most significant contributor to morbidity, mortality, and expenses associated with the hospitalization [2].
Advancement of technology made lot of improvement in the health care of the patients for specific diseases. One of the important advancement in the area of surgery is cardio thoracic and vascular surgery. Thoracic surgeries are getting its important for the management of many cardiac and pulmonary disorders. The history of thoracic incisions dates to the Hippocratic era when the trephination of empyema cavities was first reported. Cardiothoracic and vascular department is regularly performing all kinds of cardiac as well as vascular and thoracic surgeries with excellent results. But no procedure is completely free of risks [3]. Almost all types of surgeries have accompanying risks and complications. Cardio thoracic and vascular surgery is no exception. Every open heart surgery, whether it is bypass operation, or simply replacing an old pacemaker, presents potential risks to its patients [4].
Pulmonary complications of cardiac surgery range from pulmonary embolism (PE) to pleural effusion. Patients who have undergone cardiac surgery exhibit a 13% to 64% decreased in forced vital capacity (PVC), forced expiratory volume in one second (FEV) and functional residual capacity (FRC). This phenomenon appears to be related to a combination of diaphragmatic dysfunction, atelectasis, and chest wall instability that occur secondary to sternotomy. The presence of diaphgramatic dysfunction and the effects of sternotomy can cause maximal inspiratory and expiratory pressures to decline. The present study to assess the effectiveness of chest physiotherapy and incentive spirometry on postoperative respiratory status and respiratory complications among children [5].
Material and Method
Setting of the study
Selection of the area for study is one of the essential steps in the research process. The selection of the hospital for the present study was on the basis of availability of subjects, feasibility of conducting study and economy of time. The study was conducted in department of Medical-Surgical Nursing, Selected Hospital, Chennai, Tamil Nadu, India.
Sample size
Sample size was 30.
Sampling technique
Samples will be selected by stratified random sampling technique. Patients who have under gone cardio thoracic and vascular surgery at the cardio thoracic and vascular surgery wards of Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu will be selected. Patients who satisfy the inclusion criteria will be selected by lottery method.
Criteria for sample selection
Inclusion criteria
• Patients above 20 years and below 75 years of age who have under gone cardio thoracic and vascular surgery.
• All cardio thoracic and vascular surgery cases like Congenital Defect Correction, Commissurotomy, Coronary Artery Bypass Graft, Thoracotomy, Pneumonectomy, Lobectomy, Segmentectomy.
• Patients who were willing to participate in the study.
Exclusion criteria
• Patients who were critically ill and on ventilator.
• Patients with chronic neurological problems.
• Patients with immediate post operative problems.
• Patients with chronic pulmonary disease.
• Patients who have psychiatric illness and are mentally challenged.
Development and Description Of Tool
Treece and Treece (1986) emphasized that the instrument selected in the research as far as possible vehicle that would be best to obtain data for drawing conclusion, pertinent to the study. The tool consists of 2 parts;
1. PART A :
Demographic variable includes age, sex, residential area, educational status, occupational status, type of work, family monthly income in rupees, unhealthy habits, source of health information regarding cardio thoracic and vascular surgery and its complication, previous history of cardio thoracic and vascular surgery, presence of co-morbid illness, specific dietary pattern, regular breathing and coughing exercise, alternative therapies and specific respiratory devices.
2. PART B:
Assessment of respiratory status using Respiratory Rate, Modified Borg Dyspnea Scale, Peak Flow Meter and Pulseoxymeter.
1. Respiratory Rate
• <12 breaths/minute- bradypnea
• 12-22 breaths/minute- normal
• >22 breaths/minute- tachypnea
1. Modified Borg Dyspnea Scale
• Grade I- slight breathlessness
• Grade II- moderate breathlessness
• Grade III- severe breathlessness
• Grade IV- maximum breathlessness
Results
Table1: Frequency and percentage distribution of demographic variables of patients who have under gone cardio thoracic and vascular surgery.
| SI No. | Demographic variable | Frequency | Percentage | |
|---|---|---|---|---|
| 1 | Age in years | (N) | (%) | |
| a | 20-39 | 5 | 16.67 | |
| b | 40-59 | 18 | 60 | |
| c | 60 and above | 7 | 23.33 | |
| 2 | Sex | |||
| a | Male | 16 | 53.33 | |
| b | Female | 14 | 46.67 | |
| 3 | Residential Area | |||
| a | Rural | 16 | 53.33 | |
| b | Urban | 1 | 3.33 | |
| c | Suburban | 13 | 43.33 | |
| 4 | Educational Status | |||
| a | Illiterate | 1 | 3.33 | |
| b | Primary | 13 | 43.33 | |
| c | Secondary | 6 | 20 | |
| d | Graduate | 10 | 33.33 | |
| 5 | Occupational Status | |||
| a | Unemployed | 9 | 30 | |
| b | Self employed | 10 | 33.33 | |
| c | Business | 6 | 20 | |
| d | Retired | 4 | 13.33 | |
| e | Government job | 1 | 3.33 | |
| 6 | Type of Work | |||
| a | Sedentary | 17 | 56.67 | |
| b | Moderate | 11 | 36.67 | |
| c | Heavy | 2 | 6.66 | |
| 7 | Family income in rupees | |||
| a | <2000 | 3 | 10 | |
| b | 2001-5000 | 20 | 66.67 | |
| c | 5001-8000 | 6 | 20 | |
| d | >8001 | 1 | 3.33 | |
| 8 | Unhealthy habits | |||
| a | Smoking | 2 | 6.67 | |
| b | Alcoholism | 1 | 3.33 | |
| c | Drug abuse | 0 | 0 | |
| d | Mixed | 11 | 36.67 | |
| e | None | 16 | 53.33 | |
| 9 | Source of health information regarding CTVS and its complication | |||
| a | Peer group | 1 | 3.33 | |
| b | Family members | 4 | 13.33 | |
| c | Health worker | 10 | 33.33 | |
| d | Mass media/ News paper | 15 | 50 | |
| 10 | Previous history of cardio thoracic vascular surgery | |||
| a | Yes | 5 | 16.67 | |
| b | No | 25 | 83.33 | |
| 11 | Presence of co-morbid illness | |||
| a | Diabetes mellitus | 5 | 16.67 | |
| b | Hypertension | 7 | 23.33 | |
| c | Both diabetes mellitus and hypertension | 11 | 36.67 | |
| d | Hyperlipidemia | 1 | 3.33 | |
| e | Respiratory diseases | 6 | 20 | |
| 12 | Any specific dietary practices | |||
| a | Fat rich diet | 7 | 23.33 | |
| b | Protein rich diet | 2 | 6.67 | |
| c | Carbohydrate rich diet | 8 | 26.67 | |
| d | Salt rich diet | 13 | 43.33 | |
| 13 | Do you practice regular breathing/coughing exercise | |||
| a | Yes | 0 | 0 | |
| b | No | 30 | 100 | |
| 14 | Any specific alternative therapy for respiratory disease | |||
| a | Ayurveda | 4 | 13.33 | |
| b | Homeopathy | 4 | 13.33 | |
| c | Naturopathy | 0 | 0 | |
| d | Siddha | 0 | 0 | |
| e | Unani | 0 | 0 | |
| f | None | 22 | 73.33 | |
| 15 | Any specific respiratory assistance device | |||
| a | Spacers | 7 | 23.33 | |
| b | Nebulizers | 23 | 76.67 | |
| c | Rotahaler | 0 | 0 | |
| d | Nasal sprays | 0 | 0 | |
Table 1 reveals that the Frequency and percentage distribution of demographic variables of patients who have under gone cardio thoracic and vascular surgery. With regard to age, the majority of the subjects 18 (60%) belongs to the age group of 40-59 years, seven (23.33%) belongs to the age group of >60 years and five (16.67%) of them were from age group of 20-39 years.Regarding sex, majority of subjects 16 (53.33%) were males, and 14 (46.67%) subjects were females.
Regarding residential area, majority of subjects 16 (53.33%) and (43.33%) were from rural and suburban areas respectively. Only one (3.33%) of them was from urban area. With regard to educational qualification, (42.33%) had primary school education. Out of subjects, (33.33%) was graduate and six (20%) of them had done secondary education. Only one (3.33%) was found illiterate.Regarding occupation, majority of subjects were self employed and unemployed with a number of 10 (33.33%) and nine (30%) respectively. Six (20%) of them were doing own business and four (13.33%) of them were retired. Only one (3.33%) was doing government job.Considering the type of work, majority of them i.e. (56.67%) were doing sedentary work. (36.67%) of them were doing moderate work and only two (6.66%) of them were doing heavy work. Majority of the subjects i.e. (66.67%) had monthly income between 2001-5000. Six (20%) of them were having family income in between 5001-8000 and out of 30 subjects three (10%) got income less than 2000. Only one (3.33%) of them was getting income more than 8001 per month.The above table depicts that, majority of the subjects 16 (53.33%) did not have any unhealthy habits of smoking and alcoholism. Only two (6.67%) were having only smoking and one (3.33%) was having only alcoholism. 11 (36.67%) got mixed bad habit of smoking and alcoholism. None was found with any bad habit of drug abuse.
With regards to the source of information regarding CTVS and its complication, majority 15 (50%) of them were getting information from mass media and news paper. 10 (33.33%) of them were getting information from health members and four (13.33%) of them were getting information from their family members. Only one (3.33%) of them gets information from peer group.Out of 30 subjects majority of them i.e. (83.33%) had no history of any cardio thoracic vascular surgery. Other five (16.67%) had under gone for cardio thoracic vascular surgery before. Considering the co-morbid illness majority of them i.e. 11 (36.67%) were having both diabetes mellitus and hypertension. Seven (23.33%) of them were having hypertension and five (16.67%) were having diabetes mellitus alone. Six (20%) of them were suffering from respiratory diseases. Only one (3.33%) was having hyperlipidemia.
Regarding the dietary pattern of the subjects, majority 13 (43.33%) of them were taking salt rich diet. seven (23.33%) and 8 (26.67%) of them were taking fat rich and carbohydrate rich diet respectively. Only two (6.67%) of them were taking protein rich die .The above table reveals that none of the subjects were practicing breathing and coughing exercise on regular basis. With regards to the alternative therapy for respiratory diseases, majority of them 22 (73.33%) did not rely on any of the alternative medicine. Considering the rest of them, half of them four (13.33%) were taking Ayurveda and rest of them four (13.33%) relied on Homeopathy. Nobody was taking Naturopathy, Siddha and Unani.
As far as respiratory assistance devices were concerned, majority of them 23 (76.67%) were under nebulization and other seven (23.33%) of them were having spacers. None of them were taking rotahaler and nasal sprays.
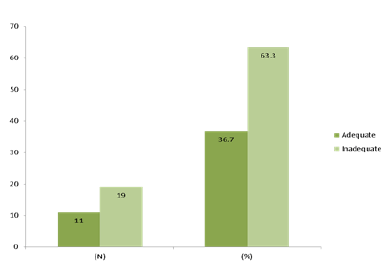
The frequency and percentage distribution of respiratory status of patients according to respiratory assessment with Respiratory Rate, Modified Borg Dyspnea Scale, Peak Flow Meter and Pulseoxymeter during Pre Test. Most of the patients i.e. (63.3%) were having inadequate respiratory status and others i.e. (36.7%) were having adequate respiratory status. It was found that most of the patients were having inadequate respiratory status. It was categorized from the four respiratory assessment parameters like Respiratory Rate, Modified Borg Dyspnea Scale, Peak Flow Meter and Pulseoxymeter (figure 1).
Figure 1: The frequency and percentage distribution of respiratory status of patients
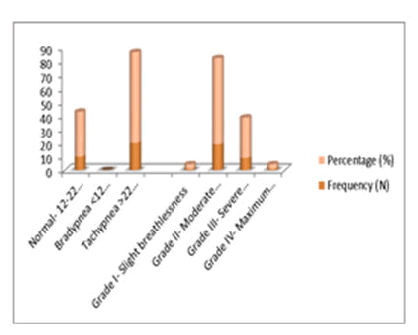
The frequency and percentage distribution of respiratory rate among patients who have under gone cardio thoracic and vascular surgery during pre-test. Most of the subjects i.e. 20(66.7%) were having tachypnea with more than 22 breaths/minute. Rest of the samples i.e. 10(33.3%) were having normal respiratory rate i.e. between 12-22 breaths/minute. None of them were having bradypnea (Figure 2).
Figure 2: The frequency and percentage distribution of respiratory pattern assessed
The frequency and percentage distribution of respiratory pattern assessed with Modified Borg Dyspnea scale among patients who have undergone cardio thoracic and vascular surgery during pretest. Data shows that majority of the subjects 19 (63.3%) were in Grade II category i.e. with moderate breathlessness. Only one (3.3%) subject was found in each category of Grade I- slight breathlessness and Grade IV- maximum breathlessness. About nine (30%) were found in Grade III i.e. severe breathlessness category.
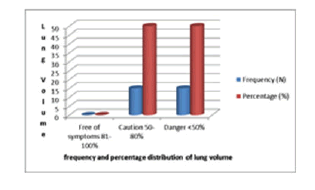
Depicts the frequency and percentage distribution of lung volume assessed with Peak Flow Meter among patients who have undergone cardio thoracic and vascular surgery during pre-test (Figure 3).
Figure 3: lung volume assessed with Peak Flow Meter among patients who have undergone cardio thoracic and vascular surgery during pretest
Half of the subjects i.e. 15(50%) were in caution with a level between 50-80% and the other half 15(50%) in the danger category with <50%. None of them were found with the free of symptoms.
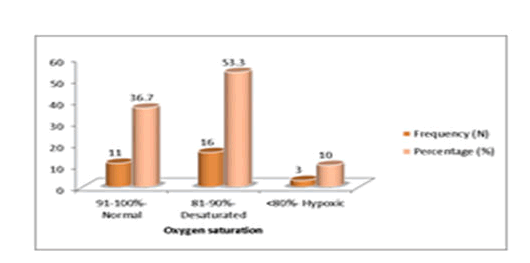
Figure 4: It shows the frequency and percentage distribution of oxygen saturation assessed with Pulseoxymeter among patients who have undergone cardio thoracic and vascular surgery during pretest.
More than half of the subjects i.e. 16(53.3%) were desaturated that is with oxygen saturation level between 81-90% while 11(36.7%) of them were in normal category with oxygen saturation 91-100%. Only 3(10%) of the subjects were hypoxic i.e. with oxygen saturation <80%.
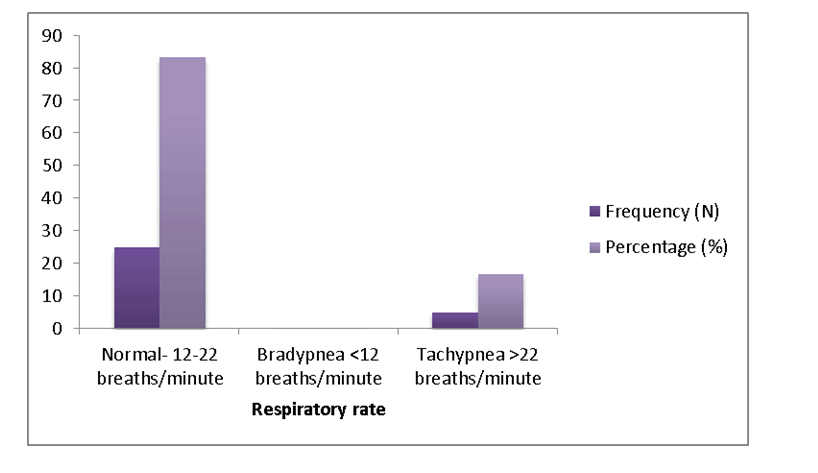
Figure 5: It shows the frequency and percentage distribution of respiratory rate among patients who have under gone cardio thoracic and vascular surgery during post test
Most of the subjects i.e. 25 (83.3%) were having normal respiratory rate with 12-22 breaths/minute. Rest of the samples i.e. 5 (16.7%) were having tachypnea i.e. >22 breaths/minute. None of them were having bradypnea, i.e. <12 breaths/minute.
| Group | Mean | Mean Difference | N | S D | ‘t’ value (df) | P value |
|---|---|---|---|---|---|---|
| Pretest | 1.6 | 0.58 | 30 | 0.488 | 6.595 (29) | 0.000*** |
| Post test | 1.02 | 30 | 0.181 |
***Highly significant at p<0.001
Table1: Reveals the distribution of mean respiratory status of patients who have under gone cardio thoracic and vascular surgery during pretest and post test according to respiratory assessment with Respiratory Rate, Modified Borg Dyspnea Scale, Peak Flow Meter and Pulseoxymeter (Table 1).
The mean difference was 0.58 between pretest mean score (1.60) and post test mean score (1.02). The table shows that there is decrease in standard deviation values from pretest to post test. The obtained paired ‘t’ value was 6.595 and P-value was 0.000***. It was highly significant at p<0.001 % level. Hence the stated null hypothesis H01 was rejected. It was inferred that deep breathing exercise with incentive spirometer is effective in improving the respiratory status of the patients who have under gone cardio thoracic and vascular surgery.
| Group | Mean | Mean Difference | N | S D | ‘t’ value (df) | P value |
|---|---|---|---|---|---|---|
| Pretest | 1.63 | 0.6 | 30 | 0.49 | 8.93 | 0.000*** |
| Post test | 1.03 | 30 | 0.183 | -29 |
***Highly significant at p<0.001
Table2: gives the distribution of mean oxygen saturation of patients who have under gone cardio thoracic and vascular surgery during pretest and post test assessed with Pulseoxymeter (Table 2).
The mean difference was 0.6 between pretest mean score (1.63) and post test mean score (1.03). The table shows that there is decrease in standard deviation values from pretest to post test. The obtained paired‘t’ value was 8.930 and P-value was 0.000***. It was highly significant at p<0.001 It was highly significant at p<0.001 % level. Hence the stated null hypothesis H01 was rejected.It was inferred that deep breathing exercise with incentive spirometer is effective in improving the respiratory status of the patients who have under gone cardio thoracic and vascular surgery.
Discussion
Many of the patients who have endured cardio thoracic and vascular surgery will develop respiratory problems, and their respiratory rank will be remarkably poor. Due to the complications of many of the surgeries are not really getting the projected outcome and these can be prohibited easily with simpler cost effective methods.
In this work, the investigator was evaluating the efficiency of deep breathing exercise with incentive spirometer on the respiratory status of patients who have undergone cardio thoracic and vascular surgery.
The research work was conducted by using Quasi experimental one group pre-test post-test research design. The study was conducted at Bharath Institute of Higher Education and research. 30 samples that have undergone cardio thoracic and vascular surgery who were admitted in the cardio thoracic and vascular surgery wards were selected.
The investigator had trained the subjects about deep breathing exercise and incentive spirometer in the preoperative period and demographic variables were collected from the subjects using pre valuation survey. On the second post operative day pretest was taken by observation method to assess the respiratory status of the subjects using respiratory assessment parameters like Respiratory Rate, Modified Borg Dyspnea Scale, Peak Flow Meter and Pulseoxymeter.
The investigator assisted the subject to perform deep breathing exercise three times per day along with second hourly incentive spirometer from the second post operative day for five days. After five days i.e. on seventh post operative day post test was done using respiratory assessment parameters like Respiratory Rate, Modified Borg Dyspnea Scale, Peak Flow meter and Pulseoxymeter. The response was analyzed through descriptive statistics (Mean, Frequency, Percentage and Standard Deviation) and inferential statistics (Paired‘t’ test and Chi-Square test). Discussions on the findings are arranged based on the objectives of the study.
The first objective of the present study was to assess the respiratory status of the patients who have undergone cardio thoracic and vascular surgery during pretest. Data shows that most of the patients were having inadequate respiratory status. They shows the frequency and percentage distribution of respiratory status among patients who have undergone cardio thoracic and vascular surgery during pretest. It revealed that about 19(63.3%) of the subjects were having inadequate respiratory status and rest of them i.e. 11(36.7%) were having adequate respiratory status.
Figure 1 gives the frequency and percentage distribution of respiratory rate among patients who have undergone cardio thoracic and vascular surgery during pretest and it gave that most of the subjects i.e. 20(66.7%) were having tachypnea with more than 22 breaths/minute. Rest of the samples i.e. 10(33.3%) were having normal respiratory rate i.e. between 12-22 breaths/minute.
Figure 2 depicts the frequency and percentage distribution of respiratory pattern (dyspnea) assessed with Modified Borg Dyspnea Scale among patients who have undergone cardio thoracic and vascular surgery during pretest. Data shows that majority of the subjects 19 (63.3%) were in Grade II category i.e. with moderate breathlessness. Only one (3.3%) subject was found in each category of Grade I- slight breathlessness and Grade IV- maximum breathlessness. About nine (30%) were found in Grade III i.e. severe breathlessness category. Table-4.2.3 reveals the frequency and percentage distribution of lung volume assessed with Peak Flow Meter among patients who have undergone cardio thoracic and vascular surgery during pretest. Half of the subjects i.e. 15(50%) were in caution with a level between 50-80% and the other half 15(50%) in the danger category with <50%. None of them were found with the free of symptoms. The frequency and percentage distribution of oxygen saturation assessed with Pulseoxymeter among patients who have undergone cardio thoracic and vascular surgery during pretest. More than half of the subjects i.e. 16(53.3%) were desaturated that is with oxygen saturation level between 81-90% while 11(36.7%) of them were in normal category with oxygen saturation 91-100%. Only 3(10%) of the subjects were hypoxic i.e. with oxygen saturation <80%.
The second objective of the study was to assess the effectiveness of deep breathing exercise with incentive spirometer on the respiratory status of patients who have undergone cardio thoracic and vascular surgery. The present study results indicated that the mean difference was 0.60 between pretest mean score (1.63) and post test mean score (1.03). The obtained paired‘t’ value was 6.595 and P-value was 0.000***. It was highly significant at p<0.001 % level. Hence the stated null hypothesis H01, which states that there is no significant difference between the pre-test and post-test respiratory status of patients who have undergone cardio thoracic and vascular surgery before and after the administration of deep breathing exercise with incentive spirometer was rejected. Thus it was inferred that deep breathing exercise with incentive spirometer is effective in improving the respiratory status of the patients who have undergone cardio thoracic and vascular surgery. This data was supported by Andrew et al. they says that deep breathing exercise along with incentive spirometer as the cheapest method for improving the respiratory status.
The third objective of the study was to associate the effectiveness of deep breathing exercise with incentive spirometer on respiratory status of patients who have undergone cardio thoracic and vascular surgery and selected demographic variables. The pre assessment questionnaire mainly consist of details of Age, Sex, Residential Area, Educational Status, Occupational Status, Type of Work, Family Monthly Income in Rupees, Unhealthy Habits, Source of Health Information regarding Cardio Thoracic Vascular Surgery and its Complications, Previous History of Cardio Thoracic Vascular Surgery, Presence of Co-morbid Illness, Specific Dietary Pattern, Regular Breathing and Coughing Exercise, Alternative Therapies and Specific Respiratory Devices. After the assessment the data shows that there is no significant association between any of these variables with the effectiveness of deep breathing exercise with incentive spirometer in the present study. Thus the null hypothesis H02 which states that there is no significant association between the effectiveness of deep breathing exercise with incentive spirometer on the respiratory status of patient who have undergone cardio thoracic and vascular surgery and demographic variables was accepted
Conclusion
Depending on the statistical investigation, it can be concise that, a deep breathing exercise with Incentive Spirometry is more efficient in averting postoperative complications following cardio-thorax surgery. Moreover, significant improvement was detected in pulmonary function test in study group after use of incentive spirometry.
Acknowledgements
The encouragement and support from Bharath Institute of Higher Education and Research, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- M D Vivek Rao. Exercise oxymetry verses spirometry 9in assessment of risk prior to lung resection. Pulm Med. 2008; 63(5): 49-60.
- Madanmohan, et al. Effect of slow and fast pranayama. Lung India. 2005; 44(6): 54-80.
- Ludwig C, et al. Intermittent positive pressure breathing after lung surgery. Respir Med. 2011; 44(1): 58-74.
- Karin Valkenet. Effect of preoperative exercise therapy on post operative outcome. J cardiovas medi. 2010; 44(12): 74-88.
- Genc A, et al. Effects of deep breathing exercise on oxygenation after head and neck surgery. Eur Clin Respir J. 2008; 50(8): 82-105.
Author Info
Department of Nursing, Bharath Institute of Higher Education and Research, Selaiyur, Chennai-600073 Tamil Nadu, IndiaCitation: AR. Bharathi, Assess The Effectiveness of Deep Breathing Exercise with Incentive Spirometer on the Respiratory status of Cardio Thoracic and Vascular Patients, J Res Med Dent Sci, 2021, 9(11): 165-179.
Received: 01-Dec-2021 Accepted: 15-Dec-2021 Published: 22-Dec-2021