Research - (2021) Volume 9, Issue 6
Assessing the Major Life Events, Anxiety and Depression among Patients with Non-Cardiac Chest Pain
*Correspondence: Nambi S, Department of Psychiatry, Sree Balaji Medical College, India, Email:
Abstract
The psychological attributes, quality of life, etiological understanding and pathways of care of patients with a non-cardiac chest pain. Hospital Anxiety and Depression Scale (HADS), Hamilton Depression Rating Scale (HAM D), and Hamilton Anxiety Rating Scale (HAM A) would be used to assess anxiety and depression. HADS was used to screen for Depression and Anxiety. Those with neither Anxiety nor Depression were excluded and the remaining patients were administered HAM–D, HAM–A, PSLES, MSPSS & WHOQOL. In the present study of a psychiatric disorder in patients that were diagnosed with a chest pain, that’s non–cardiac in nature by using a MINI International Neuropsychiatric Interview. The diagnostic criteria were taken from ICD–10.Panic disorder was found to be present in 23% of the patients. MAD, Mild Depressive Disorder & Moderate Depressive Disorder was found to be present in 14% of the patients. GAD was found to be present in 11% of the patients. Dysthymia was found to be present in 9% of the patients & Adjustment Disorder & Somatization Disorder was found to be present in 6% of the patients. Severe Depressive Disorder was found to be present in 3% of the patients.
Keywords
Psychological, Hospital anxiety and depression scale, Non-cardiac chest pain, Neuropsychiatric
Introduction
The early presentation of the patient to the hospital after the onset of an acute chest pain has been promoted by organizations throughout the world, such as The American Heart Association, The British Heart Foundation &The Heart Foundation of Australia [1,2]. Establishing the diagnosis of non–cardiac chest pain can be difficult as the condition as such can be heterogeneous in nature [3].
The clinical observations, that are made from the assessment of patient in relation to the condition begs for important questions to be asked; In the community, how many people suffer from recurrent occurrences of non– cardiac chest pain ? How many of these unfortunate individuals seek medical attention on a repetitive basis for their chest pain, that is non–cardiac in nature? What can we estimate as a probable cost to our health care system, because of this dreadful condition? Can behavioural modulations be implemented into the current health care system so that patients, who are seeking for an answer & a solution to their recurrent chest pains are finally given a solution? [3].
The prevalence of non–cardiac chest pain has been based primarily on the assessments that have been compiled from hospital–based studies or from case studies. These studies have always concentrated on the occurrence of chest pain in relation to Ischemic heart disease [4,5]. Chest pain is one of the most common complaints, which are presented by the patient to his / her doctor in the emergency department [6].
Of these patients, about one third of them are diagnosed with an Acute coronary syndrome (ACS) and the other two thirds of them had presented with a chest pain, that was assessed to be non–cardiac in nature [7]. The occurrence of the chest pain in the patient may be attributed to somatization, whereby a psychological conflict that takes places within the individual is converted into a bodily symptom.
Patients that are diagnosed with non–cardiac chest pain often undergo unnecessary diagnostic evaluations & frequent hospitalizations, which naturally subject the health care system to an unnecessary amount of expenditure [8].
Understanding the psychological mechanisms of non– cardiac chest pain would be rather helpful in refining an appropriate management plan for the concerned patient. Non–cardiac chest in an emergency setting can also be caused by the occurrence of psychiatric disorders, especially Panic, Anxiety & Depressive disorders [8-13]. In developing countries such as India less attention is usually given to a patient’s psychological symptoms.
This could be due to a lack of sensitivity to the psychological issues that may trouble a patient. The occurrence of panic disorder among patients that have been diagnosed with non–cardiac chest pain is 16–43% [9,10-13]. Anxiety and Depressive disorders range between 23–57% in patients that have been diagnosed with non–cardiac chest pain [8,11-13].
Material and Method
The Cross sectional observational study was performed in the out patients from Cardiology/General Medicine/ Psychiatry. Patients approaching the above mentioned departments with a diagnosis of non–cardiac chest pain would be included into the study. The Sampling would be purposive in nature.
An Ethical approval from the Institutional Ethics Committee would be taken prior to conduct of the study. The Patients fulfilling the Inclusion and the Exclusion criteria would be offered a participation in the study. Patients would then be recruited into the study after obtaining an Informed consent from the concerned patient. The Demographic and the Clinical characteristics of the included patients would be recorded.
Hospital Anxiety and Depression Scale (HADS), Hamilton Depression Rating Scale (HAM D), and Hamilton Anxiety Rating Scale (HAM A) would be used to assess anxiety and depression. HADS was used to screen for Depression and Anxiety. Those with neither Anxiety nor Depression were excluded and the remaining patients were administered HAM–D, HAM–A, PSLES, MSPSS & WHOQOL. General Health Questionnaire (GHQ) would be used to screen for psychological distress. Mini International Neuropsychiatric Interview (MINI) would be used to assess for presence of a psychiatric diagnosis. Presumptive Stressful Life Events Scale (PSLES) would be used to assess for stressors and Multidimensional Scale of Perceived Social Support (MSPSS) would be used to assess social support. WHOQOL Bref would be used to assess quality of life. Pathways of care would be assessed using WHO encounter form.
Results and Discussion
Among the total number of cases, 60% of them were females and 40% of them were males (Figure 1). In our study, the distribution of the type of family was 11% divorced, 54% married, 9% separated, 23% single, 3% widow or widower (Figure 2). Among the study group, 66% were educated up to school level, 26% were graduates and 8% did not have formal school education (Figure 3). Among the study group, 26% were selfemployed, 9% were into their own business, 23% were working in private organizations and 42% were unemployed (Figure 4). The significant symptoms of the Bradford Somantic Inventory was recorded and it was found that the symptoms of getting mouth or throat getting dry and aches & pains in the abdomen had most of the responses as rated 1 and the symptoms of pain in the chest or heart and pressure or tightness on the chest had most of the responses as rated 2 (Table 1 and Figure 5).
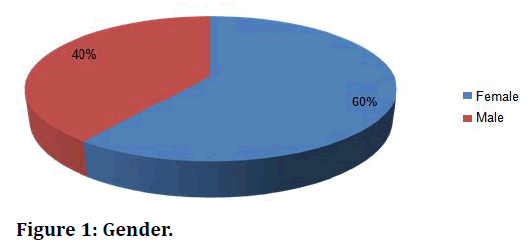
Figure 1. Gender.
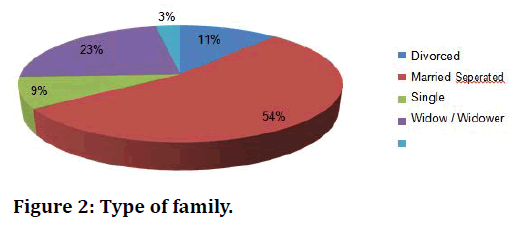
Figure 2. Type of family.
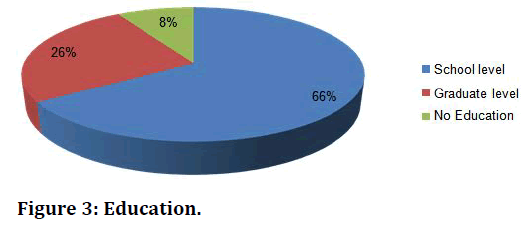
Figure 3. Education.
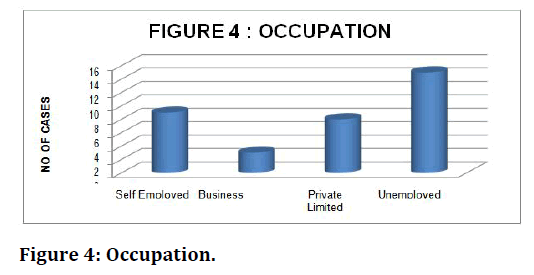
Figure 4. Occupation.
| BSI-Significant symptoms | 1 | 2 |
| Mouth or throat getting dry | 19 | 7 |
| Aches & pains in the abdomen | 16 | 4 |
| Pain in the chest or heart | 2 | 32 |
| Pressure or tightness on the chest | 8 | 24 |
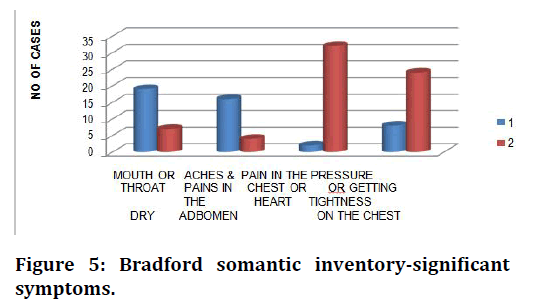
Figure 5. Bradford somantic inventory-significant symptoms.
Table 1: Symptoms.
The response collected from the male respondents with regard to their sexual difficulty in sustaining full erection was recorded and 2 cases had a rating of 1 and 14 had a rating of 0. Similarly, 4 cases experienced a rating 1 with regard to the feeling of passing semen in the urine and 12 cases had a rating 0. The response collected with the generalized health questionnaire is explained in Figure 6.
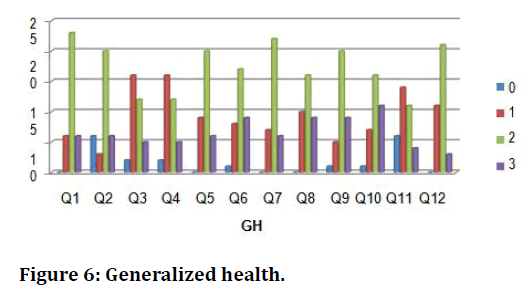
Figure 6. Generalized health.
The response collected with the Hospital Anxiety & Depression Scale significant symptoms are explained as– the symptoms I feel cheerful & I can sit at ease and feel relaxed had the rating 1. The symptoms I still enjoy the things that I used to enjoy and I feel tense or wound up had the rating 2. The symptoms I have lost interest in appearance and I feel cheerful had the rating 3 (Figure 7 to Figure 9).
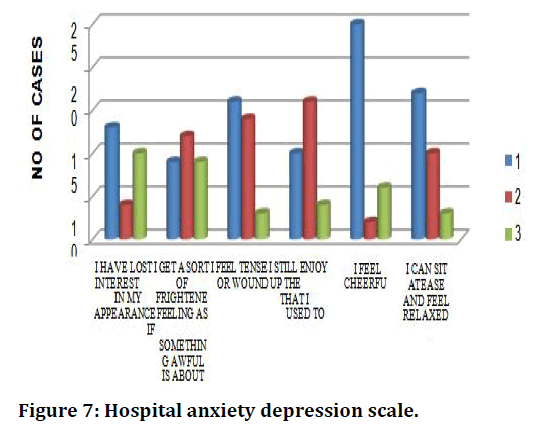
Figure 7. Hospital anxiety depression scale.
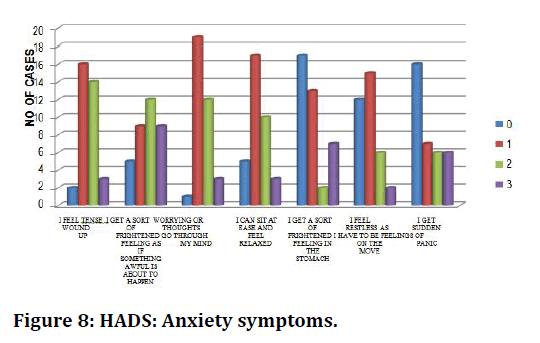
Figure 8. HADS: Anxiety symptoms.
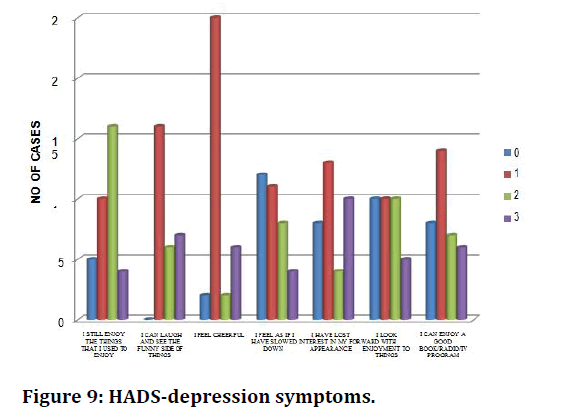
Figure 9. HADS-depression symptoms.
The response collected with the Hamilton Depression Rating Scale significant symptoms are explained as–the symptoms for Q12 & Q14 had the highest rating 1. The symptoms Q7 & Q8 had the highest rating 2 as well as 3 (Figure 10). The response collected with the Hamilton Anxiety Rating Scale significant symptoms are explained as–the symptoms for Q4 & Q9 had the highest rating 1, the symptoms Q1 & Q6 had the highest rating 2 as well as 3 (Figure 11). The response collected with regard to the disorders with the Mini Questionnaire using ICD 10 is given as follows. The adjustment order was found in 6% of the cases, Dysthymia was found in 9% of the cases, GAD was found in 11% of the cases, MAD was found in 14% of the cases, Mild depressive disorder was found in 14% of the cases, Moderate depressive disorder was found in 23% of the cases, Panic disorder was found in 23% of the cases, Severe depressive disorder was found in 3% of the cases, Somatization disorder was found in 2% of the cases (Figure 12).
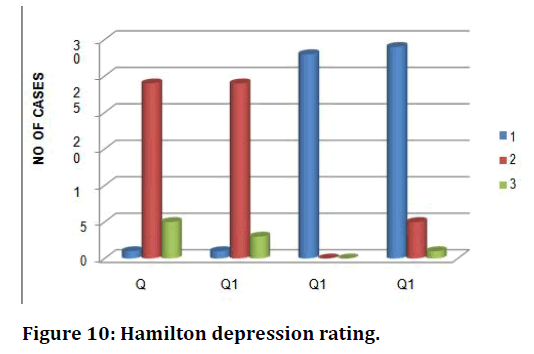
Figure 10. Hamilton depression rating.
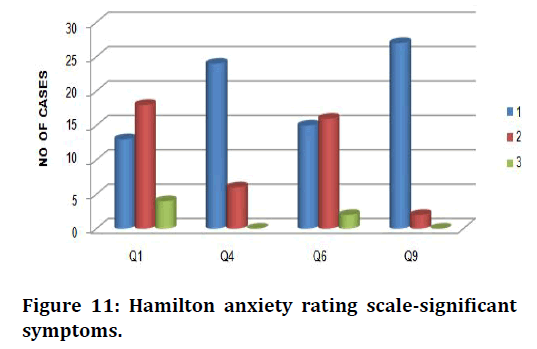
Figure 11. Hamilton anxiety rating scale-significant symptoms.
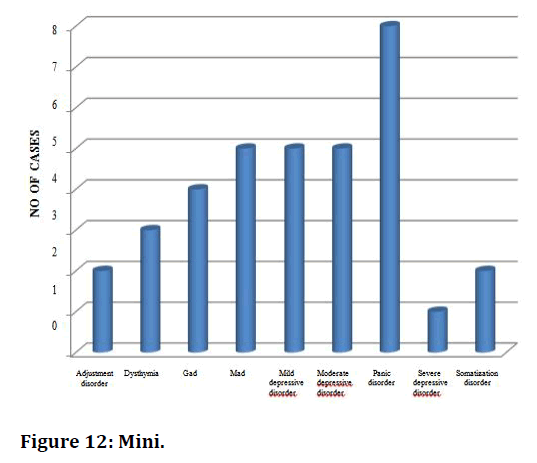
Figure 12. Mini.
The responses were recorded with regard to the PSLES and the significant stressors are explained as follows. Q7- The death of close family member was the significant stressor for 13 cases, Q8-Marital conflict was the significant stressor for 20 cases, Q 12–Excessive alcohol or drug use by family member was the significant stressor for 18 cases, Q17–Financial loss or problems was the significant stressor for 27 cases, Q18–Illness of family member was the significant stressor for 15 cases, Q24–Self or family member unemployed was the significant stressor for 11 cases, Q36–Trouble with neighbour was the significant stressor for 10 cases, Q44– Change in sleeping habits was the significant stressor for 23 cases, Q49–Change in eating habit was the significant stressor for 11 cases (Figure 13).
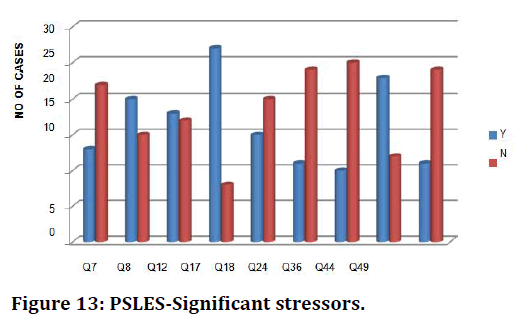
Figure 13. PSLES-Significant stressors.
The responses were recorded with regard to the MSPSS and the significant stressors are explained as follows. Q1–There is a special person who is around when I am in need had the highest score 3 , Q3–My family really tries to help me had the highest score 5, Q4–I get the emotional help and support I need from the family had me had the highest score 2, Q5–I have a special person who is a real source of comfort to me had the highest score 4, Q7–I can count on my friends when things go wrong had the highest score 1, Q9–I have friends with whom I can share my joys and sorrows had the highest score 2, Q10
There is a special person in my life who cares about my feelings had the highest score 6, Q 11–My family is willing to help me make decisions had the highest score 5, Q 12–I can talk about my problems with my friends had the highest score 4 (Figure 14).
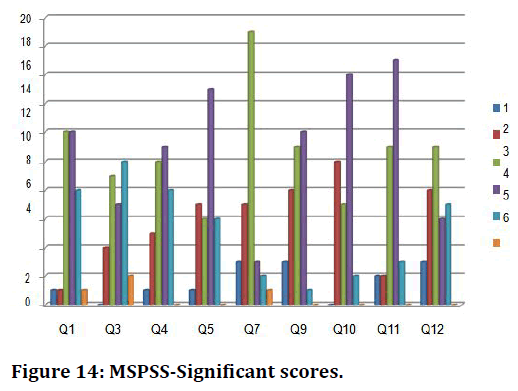
Figure 14. MSPSS-Significant scores.
The responses were recorded with regard to the WHOQOL BREF and the significant scores are explained as follows. Q1–How would you rate your quality of life had the highest score 3 , Q3–To what extent do you feel that physical pain prevents youfrom doing what you need to do had the highest score 3, Q4– How much do you need any medical treatment to function in your daily life had the highest score 4, Q11- Are you able to accept your bodily appearance had the highest score 2, Q12-Have you enough money to meet your needs had the highest score 1, Q16-How satisfied are you with your sleep had the highest score 4, Q18- How satisfied are you with your capacity for work had the highest score 5, Q21-How satisfied are you with your sex life had the highest score 3 (Figure 15).
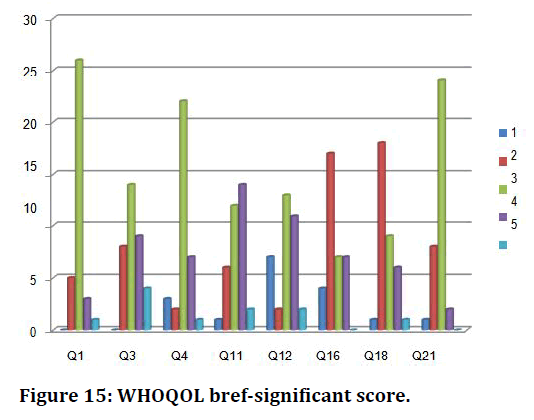
Figure 15. WHOQOL bref-significant score.
Among the total cases, 71% were seen by the medical practitioner, 17% were seen by psychiatric services, 12% were seen by specialist first (Figure 16).
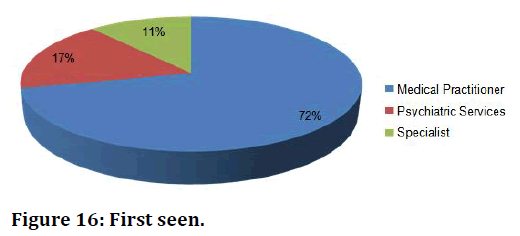
Figure 16. First seen.
We assessed for the presence of a psychiatric disorder in patients that were diagnosed with a chest pain, that’s non cardiac in nature by using a MINI International Neuropsychiatric Interview . The diagnostic criteria were taken from ICD–10.Panic disorder was found to be present in 23% of the patients. MAD, Mild Depressive Disorder & Moderate Depressive Disorder was found to be present in 14% of the patients. GAD was found to be present in 11% of the patients. Dysthymia was found to be present in 9% of the patients & Adjustment Disorder & Somatization Disorder was found to be present in 6% of the patients. Severe Depressive Disorder was found to be present in 3% of the patients
In order to assess for the symptoms of Anxiety and Depression in patients that were diagnosed with a chest pain, that’s non–cardiac in nature we used a Hamilton Depression Rating Scale is a questionnaire that comprises of multiple items that provides an indication on the severity of the depressive symptoms in the patient& a Hamilton Anxiety Rating Scale is a questionnaire that comprises of multiple items that provide an indication on the severity of the anxiety symptoms in the patient.
In the 8 patients that were diagnosed with a Panic Disorder the average HAM–D score was 11 (Mild Severity) & the average HAM–A score was 19 (Mild to Moderate Severity). In the 4 patients that were diagnosed with GAD the average HAM–D score was 10 (Mild Severity) & the average HAM–A score of 20 (Mild to Moderate Severity). In the 5 patients that were diagnosed with MAD the average HAM–D score is 12 (Mild Severity) & the average HAM–A score is 15 (Mild Severity).
In the 5 patients that were diagnosed with Mild Depressive Disorder the average HAM–D score is 12 (Mild Severity) & the average HAM–A score is 8 (Mild Severity). In the 5 patients that were diagnosed with Moderate Depressive Disorder the average HAM–D score is 18 (Moderate Severity) & the average HAM–A scores is 12 (Mild Severity). In the 3 patients that were diagnosed with Dysthymia the average HAM–D score is 11 (Mild Severity) & the average HAM–A score is 7 (Mild Severity). In the 2 patients that were diagnosed with Adjustment Disorder the average HAM–D score is 14 (Moderate Severity) & the average HAM–A score is 14 (Mild Severity)
In the 2 patients that were diagnosed with Somatization Disorder the average HAM–D score is 8 (Mild Severity) & the average HAM–A score is 15 (Mild Severity). In the 1 patient that was diagnosed with Severe Depressive Disorder the HAM–D score is 21 (Severe Severity) & the HAM –A score is 18 (Mild to Moderate Severity).
To assess the perceived stressors; patients that were diagnosed with a chest pain, that’s non–cardiac in nature a Presumptive Stressful Life Events Scale was administered and identified the 3 most common stressors–Marital conflict was scored by 20 patients. Financial loss or problems was scored by 27 patients Change in sleeping habits was scored by 23 patients.
To assess the social support systems among patients that were diagnosed with a chest pain, that’s non–cardiac in nature a Multidimensional Scale of Perceived Social Support was administered and identified that patients who presented with higher levels of Anxiety and Depression incidentally scored less. This was interpreted as those patients having decreased levels of social support. MSPSS also correlated with scores on the PSLES. The quality of life among patients that were diagnosed with a chest pain, that’s non–cardiac in nature using a WHO Quality of Life Questionnaire was administered and identified that patients with Anxiety and Depressive symptoms scored less in the Psychological Domain & in the Social Relationships Domain as the most common stressor was–Not having enough money to meet the patient’s financial needs.
The patient feeling that physical pain prevented them from performing their daily activates to their full potential. The pathways of care was used among patients that were diagnosed with a chest pain, that’s non–cardiac in nature using a WHO Encounter Form in order to identify that 71% of the cases were seen by the Medical Practitioner. About 17% of the cases had come to Psychiatric Services for the first time. About 12% of the cases were seen by Specialist before they arrived at Psychiatric Services. A study in a tertiary mental health facility in Jaipur using a WHO Encounter form to assess 76 patients that had attended the Out Patient Department found that the median duration for the untreated illness was around 6 months; the patients had already visited 2 centres for primary care, before they had visited a mental health professional. The median monetary cost of the care pathway was rounded to be about Rs. 3,565. In my study the patients were charged anywhere between Rs. 400–1,500 before they were referred to the Dept. of Psychiatry.
Conclusion
Among the patients that were diagnosed with a chest pain, that’s non–cardiac in nature had an average Hamilton Depression Rating Scale score that indicated Mild depressive symptoms & an average Hamilton Anxiety Rating Scale score that indicated Moderate anxiety symptoms.
In patients that were diagnosed with a chest pain, that’s non–cardiac in nature the majority of them were referred from the Dept. of General Medicine for a Psychiatric evaluation. Panic disorder was the most common diagnosis followed by Mild Depressive Disorder, Moderate Depressive Disorder & Mixed Anxiety– Depressive Disorder in patients that were diagnosed with a chest pain, that’s non–cardiac in nature.
The 3 most common stressors in patients that were diagnosed with a chest pain, that’s non–cardiac in nature using a Presumptive Stressful Life Events Scale were identified as marital conflict, Financial loss or problems & Change in sleeping habits. Not having enough money to meet the patient’s financial needs & the patient feeling that physical pain prevented them from performing their daily activates to their full potential made patients that were diagnosed with a chest pain, that’s non–cardiac in nature scoreless in a WHO Quality of Life Scale.
Funding
No funding sources.Ethical Approval
The study was approved by the Institutional Ethics Committee.Conflict of Interest
The authors declare no conflict of interest.Acknowledgement
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.References
- www.bhf.org.uk
- Eslick GD, Talley NJ. Non‐cardiac chest pain: squeezing the life out of the Australian healthcare system?. J Neurogastroenterol Motility 2011; 17:110-123.
- Eslick GD, Coulshed DS, Talley NJ. the burden of illness of non‐cardiac chest pain. Alimentary Pharmacol Therapeu 2002; 16:1217-23.
- Fruergaard P, Launbjerg J, Hesse B, et al. The diagnoses of patients admitted with acute chest pain but without myocardial infarction. European Heart J 1996; 17:1028-34.
- Ros E, Armengol X, Grande L, et al. Chest pain at rest in patients with coronary artery disease (myocardial ischemia, esophageal dysfunction, or panic disorder?). Digestive Diseas Sci 1997; 42:1344-53.
- Burt CW, McCaig LF. National hospital ambulatory medical care survey: 2003 emergency department summary. Adv Data Solutions 2004; :1-34.
- Solinas L, Raucci R, Terrazzino S, et al. Prevalence, clinical characteristics, resource utilization and outcome of patients with acute chest pain in the emergency department. A multicenter, prospective, observational study in north-eastern Italy. Italian Heart J 2003; 4:318-24.
- Kuijpers PM, Honig A, Griez EJ, et al. Panic disorder in patients with chest pain and palpitations: an often unrecognized relationship. Nederlands Tijdschrift Voor Geneeskunde 2000; 144:732-736.
- Beitman BD, Basha I, Flaker G, et al. Major depression in cardiology chest pain patients without coronary artery disease and with panic disorder. J Affective Disorders 1987; 13:51-9.
- Yinclinc KW, Wulsin LR, Arnold LM, et al. Estimated prevalences of panic disorder and depression among consecutive patients seen in an emergency department with acute chest pain. J General Internal Med 1993; 8:231-5.
- Demiryoguran NS, Karcioglu O, Topacoglu H, et al. Anxiety disorder in patients with non-specific chest pain in the emergency setting. Emergency Med J 2006; 23:99-102.
- Wulsin LR, Hillard JR, Geier P, et al. Screening emergency room patients with atypical chest pain for depression and panic disorder. Int J Psychiatr Med 1989; 18:315-23.
- Wulsin LR, Arnold LM, Hillard JR. Axis I disorders in ER patients with atypical chest pain. Int J Psychiatr Med 1991; 21:37-46.
Author Info
Department of Psychiatry, Sree Balaji Medical College, India1Department of Psychiatry, Sree Balaji Medical College, India
Citation: Anshul Ramesh, Nambi S, Assessing the Major Life Events, Anxiety and Depression among Patients with Non-Cardiac Chest Pain, J Res Med Dent Sci, 2021, 9(6): 325-330
Received: 02-Apr-2021 Accepted: 23-Jun-2021 Published: 30-Jun-2021
