Research - (2019) Volume 7, Issue 5
Assessment of Bioactive Resin-modified Glass Ionomer Restorative as a New CAD/CAM Material Part II: Fracture Strength Study
Huda A Abdulla1* and Manhal A. Majeed2
*Correspondence: Huda A Abdulla, Department of Conservative Dentistry, College of Dentistry, Tikrit University, Iraq, Email:
Abstract
The objective of this in vitro study was to evaluate and compare the fracture strength of monolithic crowns fabricated from a newly-developed bioactive CAD/CAM resin block and reinforced resin CAD/CAM block with two types of resin cement (adhesive and self-adhesive cement). Bioactive CAD/CAM blocks were fabricated from ACTIVA BioACTIVE-RESTORATIVE (PULPDENT Corporation, USA). Thirty-two human maxillary first premolar teeth were prepared to receive full crowns and then divided into two main groups of 16 teeth each according to the block type that used: Group A: crowns fabricated from the bioactive resin block, Group B: crowns fabricated from reinforced composite block (BRILLIANT Crios, COLTENE). Each group was then subdivided into two subgroups according to the type of resin cement used for cementation: Subgroups (A1, B1): RelyX Ultimate cement, Subgroups (A2, B2): ACTIVA BioACTIVE-cement. The prepared teeth were then scanned using CEREC Omnicam digital intra-oral scanner and crowns were designed using Sirona InLab (version 15.1) and milled using InLab MC XL milling unit. Each crown was cemented on its respective tooth according to manufacturer’s instructions of each cement. All cemented crowns were subjected to compressive axial loading in computer-controlled universal testing machine (LARYEE, China) at crosshead speed of 0.5 mm/ min until fracture occurred. The data were statistically analyzed using student’s t-test at a level of significance of 0.05. The results of this study showed no statistically significant differences between the mean values of fracture strength of both block types with each cement type. Meanwhile, blocks cemented with adhesive cement showed higher mean values of fracture strength than those cemented with the self-adhesive cement with statically highly significant differences. From the results of this study, it could be concluded that the newly-developed bioactive CAD/CAM block can be used clinically as monolithic crowns in the premolar area as the mean values of fracture strength of crowns fabricated from these blocks surpassed the maximum biting force in a premolar area irrespective of cement type.
Keywords
Resin block, Activa bio active, Brilliant crios, CAD/CAM, Fracture strength
Introduction
Advances in digital impression technology and manufacturing processes have led to a dramatic paradigm shift in dentistry and to the widespread use of CAD/CAM system in the fabrication of indirect dental restorations. Although ceramic CAD/CAM blocks are still commonly used clinically [1], the interest surrounding resin-composite blocks has recently been increased due to their suitable characteristics [2], including excellent machinability, edge stability and reduced brittleness which palliated some of the disadvantages encountered with ceramic CAD/ CAM blocks [3]. On the other hand, indirect restorations made from resin blocks were not as negatively affected by polymerization contraction, light curing variations and handling/manipulation inconveniences as those made from direct light-cured resin composite restoration [4].
Bioactive materials have been used in almost all fields of dentistry. They are reported to release fluoride and react to pH changes in the mouth by up taking calcium, phosphate, and fluoride ions to maintain the chemical integrity of the tooth structure. However, bioactive materials have not yet been implied in the field of CAD/CAM materials. ACTIVA BioACTIVE-RESTORATIVE is one of such restorative material, which comprises a patented bioactive shock-absorbing rubberized ionic-resin (Embrace resin) matrix that contains a small amount of water that makes them tougher and more resistant to fracture and chipping than composites [5,6]. As claimed by the manufacturer, it chemically bonds to teeth, releases more calcium, phosphate and fluoride and is more bioactive than glass ionomers [7,8]. It contains no Bisphenol A, No Bis-GMA and no BPA derivatives [9].
These positive characteristics of ACTIVA material encouraged the idea of developing a bioactive resin block for CAD/CAM applications that can release favorable ions and stimulate apatite formation in response to pH changes in the oral cavity.
Fracture strength is considered an important mechanical property that influences the clinical success of dental restorations. Therefore, this study was conducted to evaluate the fracture strength of monolithic crowns fabricated from newly-developed bioactive CAD/CAM blocks and compared with crowns fabricated from one of the commercially available resin blocks (Brilliant Crios) cemented with adhesive and self-adhesive resin cements.
Materials and Methods
Bioactive resin blocks were fabricated from ACTIVA BioACTIVE-RESTORATIVE material (PULPDENT Corporation, USA) using a clear rectangular Teflon mold. The internal dimensions of the Teflon mold size are in accordance with size 14 CAD/CAM block. The material was injected directly in the mold using a disposable auto-mixing tips. A celluloid strip was then placed on the top surface of the mold and a glass slab was placed above. A 500 gm weight was placed above the glass slab to release air bubbles and remove excess material. A period of 30-seconds was waited to allow for self-curing reaction to start. The mold was then placed in the chamber of UV light curing box (Vertex Eco Light Box, Netherlands, Holland) for 10 minutes. Block material was then separated from the mold by unscrewing the base of the mold. A metal holder specially fabricated for this study was then fixed to the fabricated block.
Thirty-two sound human maxillary first premolar teeth extracted for orthodontic purposes of comparable size and shape were selected. Each tooth received tooth preparation for full crown in accordance with the guidelines of tooth preparation for full crown made from resin block. The prepared teeth were divided into two main groups of 16 teeth each according to the block type used: Group A (study group): Crowns fabricated from bioactive resin block, Group B (control group): Crowns fabricated from reinforced composite block (BRILLIANT Crios, Coltene/ Whaledent AG, Switzerland). Each group was further subdivided into two subgroups of 8 teeth each according to cement type that used for the cementation: Subgroup 1: crowns cemented with adhesive resin cement (RelyX Ultimate, 3M ESPE, USA).
Subgroup 2: crowns cemented with self-adhesive bioactive resin cement (ACTIVA BioACTIVECement, Pulpdent Corporation, USA).
Digital impression was taken for each tooth using CEREC Omnicam digital intra-oral scanner. Crowns were designed using Sirona inLab CAD SW 15.1 and milled using inLab MC XL milling unit. Prior to cementation, proper surface treatment of the restoration and the teeth was done according to the manufacturer recommendations of each cement. Crowns of both groups were sandblasted with 50 μm aluminum oxide for 10 seconds, under 0.1 pressure, at distance of 10 mm, and at 45°angle [10]. The crowns were then cleaned in an ultrasonic cleaner for 5 minutes to remove any residue from sandblasting. For group A, the internal surface of each crown was etched with phosphoric acid gel for 15-seconds, washed for 15 seconds and air-dried. For group B, ONE COAT 7 UNIVERSAL lightcured dental adhesive (Coltene/Whaledent AG, Switzerland) was applied to the internal surface of each crown for 20 seconds, airdried for 5 seconds, and then light cured for 10-seconds with a light curing unit (Light intensity 800 mW/cm2 Perfection Plus, UK,). Teeth of subgroups A1 and B1 (cemented with RelyX Ultimate adhesive cement) were etched with phosphoric acid gel for 15 seconds, rinsed and air-dried, then Single Bond Universal Adhesive (3M ESPE, USA) was applied according to manufacturer's instructions. On the other hand, teeth of subgroups A2 and B2 (cemented with ACTIVA BioACTIVE selfadhesive cement) didn’t receive any surface treatment prior to cementation. The internal surface of each crown was loaded with either type of cement and seated on its respective tooth using a dental surveyor under a constant static load of 5 Kg, followed by light curing for 20 seconds per surface. The specimens were then removed from the cementation device and kept on bench for one hour and then stored in deionized distilled water for 24 hours [11].
After cementation, single load failure test was used to measure the fracture strength of the cemented crowns fabricated from the two CAD/ CAM materials. All cemented crowns were subjected to compressive axial loading in a computer-controlled universal testing machine (LARYEE, China) at a crosshead speed of 0.5 mm/min until fracture occurred. The maximum breaking load of each sample was recorded automatically in Newton (N) by a computer connected to the loading machine.
Fracture Mode Assessment
After completion of the fracture strength test, each sample was examined visually using a magnifying loupes (2.5x) to determine fracture mode according to Burke’s classification as shown in Table 1.
| Description | Mode of fracture |
|---|---|
| Minimal fracture or crack in crown | Code I |
| Less than half of crown lost | Code II |
| Crown fracture through midline (half of crown displaced or lost) | Code III |
| More than half of crown lost | Code IV |
| Severe fracture of crown and /or tooth | Code V |
Table 1: Burke's classification for fracture mode [12].
Results
Descriptive statistics of the fracture strength in Newton (N) of the different groups altogether with the comparison of significance between the different subgroups by student’s t-test are shown in Table 2 and Figure 1.
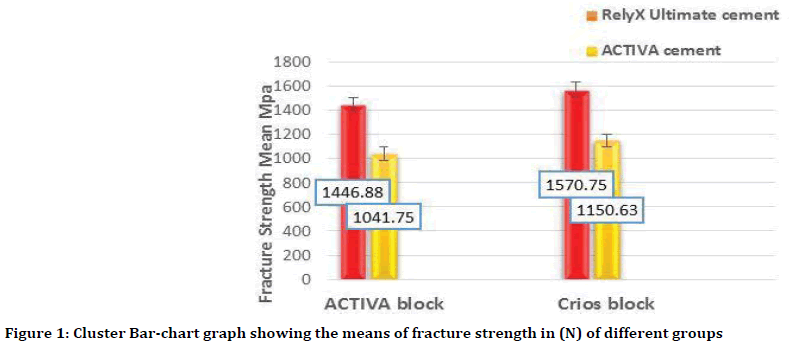
Figure 1. Cluster Bar-chart graph showing the means of fracture strength in (N) of different groups
The results of this study showed no statistically significant differences (p˃0.05) between the mean values of fracture strength of both block types within each cement type.
Further comparison between groups by student’s t-test to find out the effect of cement type on the fracture strength of crowns fabricated from the same block type was done as shown in Table 3.
| Block | Cement | Mini. | Maxi. | Mean | ±SD | t | df | p-value |
|---|---|---|---|---|---|---|---|---|
| ACTIVA Block | A1 | 1296 | 1678 | 1446.88 | 130.54 | 6.123 | 14 | 0.000 HS |
| A2 | 869 | 1240 | 1041.75 | 134.08 | ||||
| Crios Block | B1 | 1286 | 2076 | 1570.75 | 235.86 | 3.609 | 14 | 0.003 HS |
| B2 | 808 | 1532 | 1150.62 | 229.72 | ||||
| Total | Rely X Ultimate | 1286 | 2076 | 1508.81 | 194.95 | 6.06 | 30 | 0.000 S |
| ACTIVA | 808 | 1532 | 1096.19 | 190.2 |
Table 3: Descriptive statistics and comparison of significance for the effect of cement type on the fracture strength of crowns.
Blocks that cemented with adhesive cement showed higher mean values of fracture strength than those cemented with the self-adhesive cement with statistically highly significant differences.
The modes of fracture of the crowns fabricated from both block types and cemented with both cements expressed in (%) are listed in Table 4.
| Subgroups (n=8) | Code I | Code II | Code III | Code IV | Code V |
|---|---|---|---|---|---|
| A1 | - | 1 (12.5%) | 1 (12.5%) | 2 (25 %) | 4 (50%) |
| A2 | - | 1 (12.5) | 1 (12.5%) | 5 (62.5%) | 1 (12.5%) |
| B1 | - | 2 (25%) | 1 (12.5%) | - | 5 (62.5%) |
| B2 | - | 3 (37.5%) | - | 4 (50%) | 1 (12.5%) |
Table 4: Modes of fracture.
From Table 4, it can be seen that half of the crowns of subgroup A1 and more than half of subgroups B1 showed Code V (severe fracture of tooth and crown) Figures 2A and 2B. On the other hand, more than half of the crowns of subgroup A2 and half of subgroup B2 showed code IV (more than half of the crown lost) (Figures 2C and 2D).
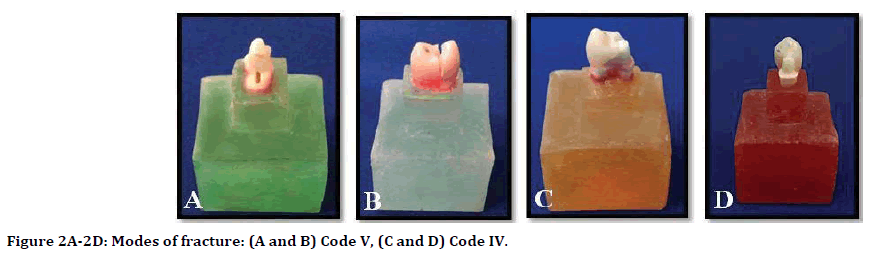
Figure 2. Modes of fracture: (A and B) Code V, (C and D) Code IV.
Discussion
Fracture strength tests of ceramic materials are important to predict their expected life and acceptable low probability of failure [13]. Single load to failure test was used in this study to test the fracture strength of crowns as it provides helpful data for comparing between the tested materials without the contribution of confounding variables brought from fatigue testing [14].
Although dynamic testing could give information about the resistance to fatigue loads, static axial load tests still represent the first step to investigate the resistance to fracture of dental materials [15]. Nonetheless, such an approach would give information about the ultimate strength of the materials that is useful to optimize the geometry of restorations, but it is worth remembering that clinical failures mainly occur because of fatigue.
The results of this study showed that the mean values of fracture strength of the different groups ranged from (1041.75 -1570.75 N). This range is far higher than the average maximum biting force of premolar region which ranges between 390-450 N [16,17] and even higher than that of molar region which ranges between 600-900 N [18,19].
This finding could be attributed, from one hand, to the adequate tooth preparation that fulfilled the preparation requirements of resin blocks which provided enough bulk of material to resist the applied load. On the other hand, this could be due to the use of adhesive and self-adhesive cementation protocols with appropriate surface treatment of the restoration and its bonded substrate according to manufacturer’s instructions.
Jassim et al. evaluated and compared the fracture strength of monolithic crowns fabricated from five different CAD/CAM materials (lithium disilicate, zirconia, reinforced composite, hybrid dental ceramic, and zirconia-reinforced lithium silicate) and found that the highest fracture strength mean value next to zirconia was recorded by crowns fabricated from BRILLIANT Crios block (1880.59 N) [20].
Despite that Crios blocks are fabricated under controlled conditions offering the highest attainable quality of polymerization under standardized parameters at high temperature and pressure, there is no statistically significant differences in the mean values of fracture strength of crowns fabricated from these blocks and those fabricated from the developed bioactive resin block regardless of the cement type (p>0.05).
This may be due to the similarity in their basic structural component that both materials are categorized as resin composite blocks composed of resin and fillers. The chemical composition and microstructure of the CAD/CAM material has a significant effect on the fracture strength of monolithic crowns [20].
In addition, ACTIVA contains a resilient resin matrix with energy-absorbing elastomeric components (blend of diurethane and methacrylates with modified polyacrylic acid), which could explained the high fracture strength value [21]. The rubberized molecules in ACTIVA matrix provide high toughness and impact strength to the matrix. This toughness helps the resin absorb mastication and other forces and provides good strength and durability to dental restorations [9].
Korkut et al. found that ACTIVA Bioactive- Restorative showed the highest values of mechanical and physical properties compared to conventional RMGIs [22]. On the other hand, Taha et al. found that RMGICs had compatible mechanical properties with either microhybrid or nanohybrid composites [23].
Concerning the effect of cement, crowns fabricated from both block types and cemented with the adhesive cement (RelyX Ultimate) showed higher mean of fracture strength than those cemented with the self-adhesive cement (ACTIVA BioACTIVE) and the differences was statistically highly significant. This results suggest that resin cement relying on the use of etch-and-rinse adhesives achieved higher fracture resistance values. Vaz et al. concluded that the bond strength corresponded to the quality of the hybrid layer. Their results showed a significant decrease in bond strength values for the self-adhesive system compared with the etch-and-rinse system [24]. Based on the results of this study, better bond strength between resin cement and tooth substrate resulted in greater fracture resistance of ceramics. This is in agreement with Rojpaibool et al. who concluded that etch-and-rinse resin cements are recommended for cementing on either enamel or dentin, compared with self-adhesive resin cements, for improved fracture resistance [25]. Moreover, Bindl et al. concluded that strong adhesive bonding with luting resin can noticeably strengthen weaker ceramic restorations and balance the inherent strength variations among different materials [26].
Furthermore, the adhesive bonding of the restoration to the tooth would create a mono block due to the similarity in the chemical composition between the resin block, resin cement, and the adhesive bonding agent which created a high bond capacity among them.
Tay et al. revealed the formation of an adhesive “monoblock” probably contributed to increase fracture strength, letting the cement act as an elastic stress absorber and compensating for the core stiffness. This could strengthen the restoration, allowing to dissipate the occlusal loads on the entire intaglio surface of the crowns [27].
Another possible attributing factor may be the higher compressive strength of RelyX Ultimate adhesive cement (262 MPa) than ACTIVA selfadhesive cement (210 MPa).
About half of the crowns fabricated from both types and cemented with the adhesive cement showed severe fracture of the crown and tooth (code V), which suggests a strong bond between the cemented crowns and their respective teeth owing to the adhesive cementation protocol used. It has been shown that adhesive cementation reduces the risk of debonding of all-ceramic restorations due to its high bond strength to the tooth structure and ceramic restorative materials [28]. Moreover, it has been found that adhesive cements used with multiple steps yielded higher bond strength than selfadhesive cements [24].
Conclusion
Fracture strength of the crowns fabricated from both CAD/CAM materials surpassed the maximum biting force in the premolar region with no statistically significant differences between both block types, suggesting that the fabricated bioactive resin block could be successfully used clinically as monolithic crown restoration in the premolar region. Crowns cemented with the adhesive cement showed higher fracture strength mean values than those cemented with self-adhesive cement with statistically highly significant differences, irrespective of the type of block material.
References
- Lauvahutanon S, Takahashi H, Shiozawa M, et al. Mechanical properties of composite resin blocks for CAD/CAM. Dent Mater J 2014; 33:705-710.
- Spitznagel FA, Horvath SD, Guess PC, et al. Resin bond to indirect composite and new ceramic/polymer materials: A review of the literature. J Esthet Restor Dent 2014; 26:382-393.
- Ruse N, Sadoun MJ. Resin-composite blocks for dental CAD/CAM applications. J Dent Res 2014; 93:1232-1234.
- Mainjot A, Dupont N, Oudkerk J, et al. From artisanal to CAD-CAM blocks: State of the art of indirect composites. J Dent Res 2016; 95:487-495.
- Garcia-Godoy F, Morrow BR, Pameijer CH. Flexural strength and fatigue of new activa RMGICS. J Dent Res 2014; 93:254.
- Chao W. Deflection at break of restorative materials. J Dent Res 2015; 94:2375.
- Slowikowski L, John S, Finkleman M, et al. Fluoride ion release and recharge over time in three restoratives. AADR Annual Meeting & Exhibition 2014; 93:268.
- Zmener O, Pameijer CH, Hernandez S. Resistance against bacterial leakage of four luting agents used for cementation of complete cast crowns. Am J Dent 2014; 27:51-55.
- https://www.pulpdent.com/activa-bioactive-white-paper
- Reymus M, Roos M, Eichberger M, et al. Bonding to new CAD/CAM resin composites: influence of air abrasion and conditioning agents as pretreatment strategy. Clin Oral Investig 2019; 23:529-538.
- Kassem AS, Atta O, El‐Mowafy O. Fatigue resistance and microleakage of CAD/CAM ceramic and composite molar crowns. J Prosthodont 2012; 21:28-32.
- Burke F. Maximising the fracture resistance of dentine-bonded all-ceramic crowns. J Dent 1999; 27:169-173.
- Ritter JE. Predicting lifetimes of materials and material structures. Dent Mater 1995; 11:142-146.
- Shahrbaf S, Van Noort R, Mirzakouchaki B, et al. Fracture strength of machined ceramic crowns as a function of tooth preparation design and the elastic modulus of the cement. Dent Mater 2014; 30:234-241.
- Sun T, Zhou S, Lai R, et al. Load-bearing capacity and the recommended thickness of dental monolithic zirconia single crowns. J Mech Behav Biomed Mater 2014; 35:93-101.
- Powers JM, Sakaguchi RL, Craig RG. Craig's restorative dental materials. Powers: Philadelphia, Elsevier/Mosby 2012.
- Sathyanarayana HP, Premkumar S, Manjula WS. Assessment of maximum voluntary bite force in adults with normal occlusion and different types of malocclusions. J Contemp Dent Pract 2012; 13:534-538.
- Braun S, Bantleon HP, Hnat WP, et al. A study of bite force, part 1: Relationship to various physical characteristics. Angle Orthod 1995; 65:367-72.
- Waltimo A, Nysträm M, Känänen M. Bite force and dentofacial morphology in men with severe dental attrition. Scand J Dent Res 1994; 102:92-96.
- Jassim ZM, Majeed MA. Comparative evaluation of the fracture strength of monolithic crowns fabricated from different all-ceramic CAD/CAM materials (an in vitro study). Biomed Pharmacol J 2018; 11:1689-1697.
- Garoushi S, Vallittu PK, Lassila L. Characterization of fluoride releasing restorative dental materials. Dent Mater J 2018; 37:293-300.
- Korkut E, Gezgin O, Tulumbacı F, et al. Comparative evaluation of mechanical properties of a bioactive resin modified glass ionomer cement. Conference Proceedings 2017.
- Taha N, Ghanim A, Tavangar MS. Comparison of mechanical properties of resin composites with resin modified glass ionomers. J Dent Biomat 2015; 2:47-53.
- Vaz RR, Hipólito VD, D'Alpino PH, et al. Bond strength and interfacial micromorphology of etch‐and‐rinse and self‐adhesive resin cements to dentin. J Prosthodont 2012; 21:101-111.
- Rojpaibool T, Leevailoj C. Fracture resistance of lithium disilicate ceramics bonded to enamel or dentin using different resin cement types and film thicknesses. J Prosthodont 2017; 26:141-149.
- Bindl A, Lüthy H, Mörmann WH. Strength and fracture pattern of monolithic CAD/CAM-Generated posterior crowns. Dent Mater 2006; 22:29-36.
- Tay FR, Pashley DH. Monoblocks in root canals: a hypothetical or a tangible goal. J Endod 2007; 33:391-398.
- Lafuente JD, Chaves A, Carmiol R, et al. Bond Strength of Dual‐Cured Resin Cements to Human Teeth. J Esthet Dent 2000; 12:105-110.
Author Info
Huda A Abdulla1* and Manhal A. Majeed2
1Department of Conservative Dentistry, College of Dentistry, Tikrit University, Iraq2Department of Conservative Dentistry, College of Dentistry, University of Baghdad, Iraq
Citation: LHuda A Abdulla, Manhal A Majeed, Assessment of Bioactive Resin-modified Glass Ionomer Restorative as a New CAD/CAM Material Part II: Fracture Strength Study, J Res Med Dent Sci, 2019, 7(5):74-79.
Received: 13-Sep-2019 Accepted: 30-Sep-2019
