Research - (2021) Volume 9, Issue 6
Assessment of Left Ventricular Function in Ischaemic Stroke
*Correspondence: E Dhandapani, Department Of General Medicine, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
To study and evaluate left ventricular function in the patients with acute ischaemic stroke. To analyse whether LV dysfunction could be a marker for hospital mortality in patients developing acute ischaemic stroke. Patients with symptomatic heart failure of NYHA class III and IV had a positive correlation with left ventricular systolic dysfunction and clinical morbidity in ischaemic stroke. ECG changes of previous MI had statistically significant correlation with left ventricular systolic dysfunction and clinical morbidity in ischaemic stroke Chest x- ray changes of cardiomegaly were observed among 4 out of 9 patients within hospital stay mortality. LV Diastolic Dysfunction was associated with in patient mortality which was statistically significant.
Keywords
Diabetics, Ischaemic heart disease, Hypertension, Myocardial infarction.
Introduction
Cardiac diseases are the major risk factors for stroke, ranking third after age and hypertension. 1Congestive Cardiac failure ranks the second in cardiogenic related stroke risk [1], with a two-to-three-fold relative risk [1,2]. The prevalence of cardiac failure increases substantially as the population ages. Cardiac failure is associated with high mortality rate, with a 15-year total mortality rate estimated at around 39% for women and 72% for men [3]. Left Ventricular Systolic Dysfunction is common and treatable, accounting for 8% of people aged 25-75 years and 12% of 45-75 years. Of the 8%,4% are asymptomatic [4-8]. The patients who are at high risk of developing LVSD are those with ischaemic heart disease, hypertension, diabetes, and smokers [9-11].
However, echocardiographic screening of all hypertensives, all diabetics, and all smokers for LVSD would be a costly process for screening. A more costeffective approach might be to do it at the first presentation of a vascular episode, and to perform routine echo screening at that time. The first vascular episode could be either an acute myocardial infarction (MI), a transient ischaemic attack (TIA), a cerebrovascular accident or peripheral vascular disease [12].
In normal clinical setting, MI patients are now screened for LVSD during their hospital admission, but patients who have had CVA/TIA/PVD are usually not routinely screened for LVSD. So, the presentation with first vascular episode in the form of stroke could be an opportunity to detect and treat LVSD, and thereby reduce the subsequent incidence of overt heart failure, and perhaps even sudden cardiac death and reduce the incidence of mortality and morbidity further We are aware that LVDD is also a major risk factor contributing towards mortality especially in the hypertensives and elderly.
It is in this context; I have tried to assess the LV function in patients who presented with ischaemic stroke especially atherothrombotic stroke [13-15].
Materials and Methods
Study design
Randomized prospective observational study.
Setting
ICU and Medical wards of Sree Balaji Medical college and Hospital, Chennai.
Study group
142 patients diagnosed as Ischaemic stroke.
Period of study
April 2017 to March 2018.
LV function was assessed by trans thoracic 2-dimensional echo cardiography in patients admitted with Ischaemic stroke in Sree Balaji Medical College and Hospital.
Exclusion criteria
Patients under the age of 40 years were excluded from the study group in this study. Patients with haemorrhagic stroke were excluded from the study group. Patients with Valvular heart diseases were excluded from the study group.
All the study group patients underwent transthoracic Echocardiography as a part of the study. All patients had a thorough clinical, neurological examination with careful evaluation of history. Importance was given to symptoms and signs of cardiac disease in addition to neurological findings.
Results
142 Patients of the study group were divided into various subgroups. Ischaemic stroke was most observed between 51 -60 years of age followed by patients aged 61-70 years. The mean age of the patients was `58 years (Figure 1). Most of the patients were men (66%) as against women (34%).
Figure 1: Age distribution.
Figure 2: Sex distribution.
Smoking
Smoking was one of the most common risk factors observed in 73 patients. All these patients were men. Out of 94 men, 73 patients were chronic smokers (78%). The mean age of the smokers was 54 years. Associated history of chronic alcohol intake was seen in 33 male patients. Associated hypertension was seen in 11 patients which had statistical significance (p value .00). Coexisting diabetes mellitus was observed in 8 patients (Figure 3).
Figure 3: Risk factor profile.
Alcohol
Alcohol intake was observed in 33 of the 94 men (23%). All of them were men. They had associated history of chronic smoking. 21 patients had associated hypercholesterolemia. 4 patients had diabetes mellitus and 4 patients had coronary artery disease. Shortness of breath on exertion was observed in 7 patients. History of angina, palpitation was present in 6 patients. Chest x ray showed cardiomegaly in 1 patient. Echo finding of L.V.H was evident in 13 patients. L.V. systolic dysfunction was present in 6 patients. Diastolic dysfunction was present in 3 patients. One patient had in hospital mortality (Figure 3).
Hypercholesterolemia
78 of the 142 patients had hypercholesterolemia (54%). Out of which 58 were men and 20 were women. It was the most common risk factor observed among the study group patients. It was most observed in the age group between 51 -60 years followed by 61 -70 years. The mean range of blood cholesterol was between 240 -260 mg/dl. 14 patients had associated diabetes mellitus. 25 patients had associated hypertension (Figure 3).
Hypertension
Hypertension was observed in 56 of the 142 patients studied (39.4%). It was most observed in the age group between 50 - 70 years when compared to those below 50 years and more than 70 years of age group. It was more frequent in women compared to men in the ratio of 36:20 17 patients had history of angina and palpitation. History of shortness of breath was observed in hypertensive patients which had no statistical significance (Figure 3).
Diabetes mellitus
26 of the 142 patients had Diabetes mellitus (18%). It was observed as a risk factor equally in both sexes (p value0.05). Previous history of coronary artery disease was present in 12 patients. Coexisting C.A.D was more commonly seen in men compared to women. History of stroke was present in 8 patients. History suggestive of angina, palpitation and shortness of breath was observed among the diabetic patients which had no statistical significance. ECG changes of previous myocardial infarction was seen in 6 patients (Figure 3).
Coronary artery disease
History of coronary artery disease was present in 12 patients (8.4%) C.A.D was more frequent in men when compared to women in the ratio of 8:4. Most common age group with CAD was between 51 -60 years. History of breathlessness on exertion of NYHA class III was more frequently observed in CAD patients (Figure 3).
Symptoms of CAD and cardiac dysfunction
History suggestive of angina was observed in 29 patients (20%). H/O of palpitation was observed in 29 patients (20%) in the absence of Valvular heart disease. Exertional breathlessness of varying degree was present in 49 patients. 4 out of 49 patients had shortness of breath at rest. Symptoms of angina and palpitation were more frequently observed in 20 patients with hypercholesterolemia (p value .03). 14 out of 49 patients had chest x-ray changes of cardiomegaly. This was associated with shortness of breath N.Y.H.A class III and IV. This association had statistical significance (p value 0.00). E.C.G changes of previous M.I was present in 9 out of 49 patients. All of them had breathlessness at rest (p value 0.00). This association was statistically significant. There was no statistically significant association between symptoms of left heart failure with diabetes mellitus and hypertension. Left ventricular systolic dysfunction was evident in echoamong9 patients with severe heart failure symptoms. This association was statistically significant (p value 0.00). Past H/O stroke was observed in 6 patients. 7 patients had altered mentation (p value 0.00). 11 patients had massive infarct on C.T. There was no statistically significant correlation between symptoms of left heart failure and mortality in the present study.
History of stroke was present in 41 out of 142 patients. Most of them were between 51 - 60 years of age. Men had more incidence of past H/O stroke, in ratio of 3:1. Out of 41 patients 16 had dense hemiplegia, 14 had altered mentation. C.T changes of massive infarct was evident 23 patients. The severity of the stroke and clinical picture had significant statistical correlation with a p value of 0 . 00.
Electrocardiographic changes were observed in 76 out of 142 patients (53%). More men had ECG changes when compared to women in the ratio of 43:33. ECG changes of LVH was more frequently observed in 14 hypertensive patients followed by 10 smokers. 28 patients had changes on chest x-ray. 5 patients had chest x- ray changes of pulmonary venous congestion. 23 patients had cardiomegaly on chest x-ray. Men and women showed chest x-ray changes in proportion of 16:12. 14 out of 23 patients with cardiomegaly on chest x- ray had N.Y.H.A class III and IV symptoms (p value .00). All the above patients had left ventricular systolic dysfunction which had no statistical significance. 3 patients had L.V diastolic dysfunction.
Left ventricular hypertrophy was observed in 65 patients in Echo. Most of them were in the age group between60-70 Years followed by 50 -60 years of age. More number of men had LVH when compared to women in the ratio of 41: 24. LVH. was observed commonly in 39 smokers followed by 29 Hypertensives. It was also evident in 13 alcoholics. 15 patients with LVH had history of angina and palpitations.
12 out of 142 patients had diastolic dysfunction in echo. 5 patients were in the age group between 51 -60 years followed by 4 patients in the age group less than 50 years. The number of men with diastolic dysfunction was more when compared to women in the ratio of 7:5.
There is no statistically significant association between diastolic dysfunction and history of angina, palpitations and symptoms of left heart failure.5 hypertensive patients had diastolic dysfunction; 2 diabetic patients had diastolic dysfunction. One patient with history of CAD had diastolic dysfunction. There was no statistically significant association between Diastolic dysfunction and chest X- ray, ECG changes. 9 out of 142 patients had in hospital mortality. The average period of hospital stay was 12 days among this group. 3 were aged between 51 to 60 years and 6 were above 70 years. Mortality was observed more commonly in men (ratio of men: women being 5:4). Among those who expired, hypercholesterolemia was seen in 7 patients. Hypertension was observed in 5 patients. 2 patients had diabetes mellitus. One patient had coronary artery disease. 5 patients had symptoms of cardiac dysfunction on admission. This association between the symptoms of left heart failure and mortality had statistical significance (p value 0.00). Cardiomegaly on chest x ray was observed in 4 out of 9 patients. This association was statistically significant (p value 0.00) (Figure 4).
Figure 4: ECG changes.
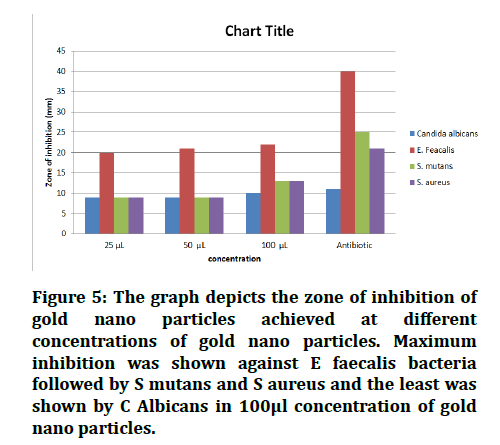
Figure 5: LVSD correlation with age.
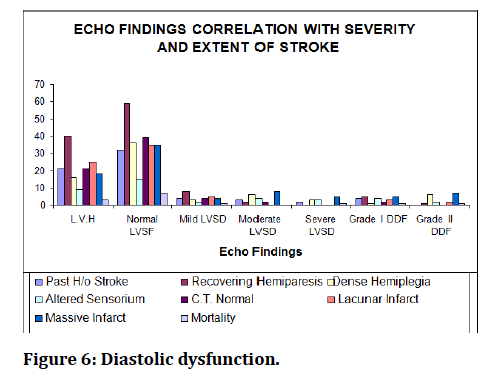
Figure 6: Diastolic dysfunction.
Discussion
The number of patients enrolled in the study was 142. Ventricular function studies in association with ischaemic stroke have been done previously by Allison G. Hays, M.D, Department of Medicine, New York (`1994 -1997) in a subset of patients from the Northern Manhattan study in 2006 (NOMAS) 46. In a study done by them, 270 patients of ischaemic stroke were evaluated for LV function in detail. Framingham study and VH ef trial 51 analysed the various risk factors in association with LV dysfunction in ischaemic stroke patients. Among the patients studied 33% were between 51 -60 years followed by 29% between 61 -70 years. The average age of patients studied was58years. The lesser incidence in people below 50 years of age could be because in our study we excluded patients with valvular heart disease and the cases of young stroke. The number of patients of over 70 years was also less. The age incidence in the current study was like the northern Manhattan study. In the NOMA study also, the age of patients more than 70 and younger than 50 years was less. 66% of patients in the present study were men as against 34% who were women. This is probably because smoking and intake of alcohol was observed in most men in the group. This contrasts with the manhatt and study figures (NOMA study) where 56% were women against 44% men The higher incidence of stroke in women of NOMA study could be due to the associated habits of smoking and alcohol intake in western women [16,17].
51% of patients in current study were chronic smokers whereas in NOMA study 23% were smokers. This difference could be due to the higher incidence of smoking in Indian men when compared to people of Western country where the habit of smoking was comparatively less than alcohol intake. The present study showed statistically significant association between smoking, hypertension, and diabetes. The association between smoking and clinical severity and morbidity of the stroke was also statistically significant in the present study. The incidence of alcohol intake was more in the NOMA study when compared to the present study. It was 40% in the NOMA study as comparedto the 23% of present study [18]. This difference could be attributed to the higher incidence of alcohol intake in Western countries when compared toour country [19].
The incidence of hypercholesterolemia was more in the present study (54%) whereas it was less in the NOMA study (38%). The above difference could be due to the changes in the lifestyle pattern of the people in India with associated alcohol intake and smoking and due to the increase in associated co morbid conditions like atherosclerosis, diabetes, hypertension and CAD. The incidence of hypertension was 39% in present study which was less when compared to NOMA study (78%). This could be due to the difference in the incidence of comorbid conditions like diabetes, CAD, dyslipidemaia. The association of hypertension and CAD was statistically significant in the present study. The ECG changes of LVH and hypertension was statistically significant in the present study.
The incidence of diabetes in the present study was 18.3% as compared to the NOMA study of 43%. The above difference may be due to the sedentary lifestyle of the western people and also due to the higher incidence of obesity among the people of western countries. There was a statistically significant correlation between diabetes and LVSD. Hospital stay mortality was statistically significant among diabetic patients in this study [20].
12 patients had diastolic dysfunction in the present study. Most of them were between 51 -60 years followed by less than 50 years. The number of men was more than women in the ratio of 7:5. Diastolic dysfunction was more frequent in hypertensives than diabetics in the ratio of 5:2.One patient with CAD had diastolic dysfunction. There is no statistically significant association between history of angina, palpitations, and symptoms of left heart failure and diastolic dysfunction. The association between Diastolic Dysfunction and chest x- ray, E.C.G changes is also statistically not significant. There is no significant association between diabetes, CAD and diastolic dysfunction in the present study. However, association between mortality and diastolic dysfunction was statistically 9 patients had In hospital mortality in the present study. Mortality was more in men than women in the ratio of 5:4. 7 out of 9 patients had hypercholesterolemia. 5 patients had hypertension. Two patients had diabetes mellitus. One patient had coronary artery disease [21-23]. NYHA class I symptoms was observed in two patients on admission (p-value 0.00). Cardiomagely on chest x- ray was observed in four patients. This association was statistically significant (p value 0.00). The clinical picture and extent of stroke was also severe among the patients with diastolic dysfunction. Four patients had altered sensorium, 5 patients had massive infarct on C.T one patient had dense hemiplegia (p value 0.04).
Conclusion
LVSD was observed in 30 patients of the present study (21.13%). LV Diastolic dysfunction was observed among 12 patients (3.4%). Association of LVSD with clinical severity and extent of the stroke had of positive correlation statistically. Association of LVSD with in hospital stay mortality was not significant. Hypercholesterolemia was observed as the most common risk factor among the ischaemic stroke patients. Coexisting coronary artery disease and diabetes mellitus had positive correlation with left ventricular systolic dysfunction. Patients with symptomatic heart failure of NYHA class III and IV had a positive correlation with left ventricular systolic dysfunction and clinical morbidity in ischaemic stroke. ECG changes of previous MI had statistically significant correlation with left ventricular systolic dysfunction and clinical morbidity in ischaemic stroke Chest x-ray changes of cardiomegaly were observed among 4 out of 9 patients within hospital stay mortality. LV Diastolic Dysfunction was associated with in patient mortality which was statistically significant.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledegements
The encouragement and support from Bharath University, Chennai, is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation, a major contributor to stroke to stroke in the elderly: The framingham study. Arch Intern Med 1987; 147:1561-1564.
- Kannel WB, Wolf PA, Verter J. Manifestations of coronary disease prodisposing to stroke : The framingham study. JAMA 1983; 250: 2942-2946.
- Schocken DD, ARrieta MI, Leaverton PE, et al. Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol 1992; 20:301-306.
- https://accessmedicine.mhmedical.com/book.aspx?bookID=1477
- McDonagh TA, Morrison CE, Lawrence A, et al. Symptomatic and asymptomatic left ventricular systolic dysfunction in an urban population. Lancet 1997; 350:829-32.
- Brockell. Prevalence of left ventricular dysfunction in the general population. J Am CollCardiol 1996; 27:25.
- Ward R, Jones D, Haponik EF. Paradoxical embolism, an under diagnosed problem. Chest 1995; 108:549-558.
- Wilson PW. An epidemiologic perspective of systemic hypertension, ischaemic heart disease and heart failure. Am J Cardiol 1997; 80: 3J-8J.
- Solvd investigators. Effect of enalapril on mortality and development of heart failure in asympotmatic patients with reduced left ventricular ejection fractions. N Engl J Med 1992; 327:685-91.
- Pfeffer MA, Braunwald E, Moye La, et al. Effect of captopril on mortality in patients with left ventricular dysfunction after myocardial infarction: Results of the survival and Ventricular Enlargement study. N Engl J Med 1992; 327:669-77.
- Gorelick RB. Stroke prevention. Arch Neurol 1995; 52:347-355.
- Rosamond WD, Folsom AR, Chambless L, et al. Stroke incidence and survival among middle aged adults. Stroke 1990; 30:736-743.
- Fabris F, Zanocchi M, Bo M, et al. Prevalence and determinants of carotid atherosclerosis in a general population . Stroke 1994; 25: 1133 -1140 .
- Wilson PW, HoegJm, D’ Agostino RB, et al. Cumulative effects of high cholesterol levels, high blood pressure, and cigarette smoking on carotid stenosis. N Engl J Med 1997; 337:516-522.
- Vaitkus PT, Berlin JA, Schwartz JS, et al. Stroke complicating acute myocardial infarction. A meta-analysis of risk modification by anticoagulation and thrombolytic therapy. Arch Intern Med 1992; 152:352-357.
- Serena J, Segura T, Perez- Ayuso MJ, et al. The need to quantify right - to-left shunt in acute ischemic stroke: A case- control study. Stroke 1998; 29:1322-1328 .
- Jones EF, Calafiore P, Donnan GA, et al. Evidence that patent foramen ovale is not a risk factor for cerebral ischemia in the elderly. Am J Cardiol 1994; 74:596-599.
- Hanna JP, Sun JP, Furlan AJ, et al. Patent foramen ovale and brain infarct. Echocardiographic predictors, recurrence and prevention. Stroke 1994; 25:782-786.
- Nishimura RA, McGoon MD, Shub C, et al. Echocardiographically documented mitral valve prolapse. Long- term follow- up of 237 patients. N England J Med 1985; 313:1305-1309.
- Longstreth WT, Litwin PE, Weaver WD. Myocardial intarction, thrombolytic therapy and stroke. A community- based study. The MITI Project Group. Stroke 1993; 24:587-590.
- Bautista RE. Embolic stroke following thrombolytic therapy for myocardial infarction in a patient with preexisting ventricular thrombi. Stroke 1995; 26:324-325.
- De Simone G, Devereux RB, Daniels SR, et al. Effect of growth on variability of left ventricular mass: Assessment of allometric signals in adults and children and their capacity to predict cardiovascular risk. J Am CollCardiol 1995; 25:1056-1062.
- Goldstein S. The electrocardiogram in stroke: Relationship to pathophysiological type and comparison with prior tracings. Stroke 1979; 10:253-259.
Author Info
Department Of General Medicine, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Y Bhargav, E Dhandapani, Assessment of Left Ventricular Function in Ischaemic Stroke, J Res Med Dent Sci, 2021, 9(6): 263-268
Received: 27-Mar-2021 Accepted: 21-Jun-2021
