Research - (2022) Volume 10, Issue 2
Assessment of Readiness to Quit Smoking Behaviour among Smokers in Chennai, Tamil Nadu
*Correspondence: Pradeep Kumar R, Department of Public Health Dentistry, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and technical sciences, Saveetha University, India, Email:
Abstract
Background: In the stages of the change model for smoking cessation, “willingness to quit” forms the starting point. The impact of the increasing burden of smoking among low and middle‐income countries is well established. To determine the willingness to quit smoking among and quit attempts among smokers in Chennai, Tamil Nadu Methods: A validated pre-tested Questionnaire was used to assess the willingness to quit. Responses were tabulated in Microsoft Excel and statistical analysis was done using SPSS version 27.0 and chi square tests. Results: From the present study, it was found that 42.3% of the smokers belong to the pre contemplation stage, 17.5% of them belong to the contemplation stage, whereas 40.1% of them were ready to quit smoking. The p value for this was 0.049 (<0.05) and hence statistically significant. Conclusion: From this study we can conclude that the majority of the smoker population has a high readiness to quit smoking. Smoking is a major public health problem. Continued effort to control and eliminate this abuse is a medical necessity. Hence, more workshops on the importance of smoking cessation should be conducted.
Keywords
Cessation, Novel questionnaire, Quit, Readiness, Smoking
Introduction
The impact of the increasing burden of smoking among low and middle-income countries is well established. Around 80% of the world’s smokers population live in low- and middle-income countries [1,2]. It is estimated that half of all deaths among individuals with mental illness are attributable to smoking. While significant progress has been made in reducing smoking use within the general population, rates of smoking remain high among individuals with mental illness, including individuals with depression and/or anxiety compared with those without such disorders [3]. Studies done in India reported the quitting rates of tobacco to be varied between 12% and 33%.
The willingness to quit smoking (tobacco) forms an important preliminary step for the behavioral change in an individual. Smoking cessation often requires numerous attempts by people and may be accompanied by anxiety and depression during the quit attempt, due in part to withdrawal symptoms [4]. Identifying these subgroups of smokers who are willing to quit becomes critical in developing effective interventions, beneficial in helping smokers quit their habit. There is paucity of literature regarding willingness to quit and the factors associated with it in India [2]. Available quitting aids are both safe and effective in supporting cessation in smoking users and stopping smoking is associated with an improvement in mental health rather than deterioration [5]. Our team has extensive knowledge and research experience that has translate into high quality publications [6–25].
Hence the aim of the present study focuses on determining the willingness to quit smoking among and quit attempts among smokers in Chennai, Tamil Nadu.
Material and Methods
A cross sectional study was conducted in Chennai among smokers visiting a private dental hospital. Smokers amongst the outpatients were included in the study. Smokers who were not willing to participate in the study were excluded from the study. Prior to the start of the study, ethical clearance was obtained from the Institutional ethics committee. The anonymity of the participants was maintained. The sample size obtained was 158.
Data collection was scheduled in the month of February 2021. Data was collected using a self-administered questionnaire among 158 smokers who visited the dental outpatient department.
A structured and self-administered questionnaire was adopted from questionnaires previously done by [26]. The questionnaire consisted of two parts. The first section consisted of demographic data such as Name, age and level of education. The second section consisted of 25 questions pertaining to assess the readiness to quit smoking among smokers. The questionnaires were distributed to the participants through google forms at the hospital and were collected on the same day.
Statistical Analysis
Data was entered in Microsoft Excel and analysed using SPSS software (version 27.0). Descriptive Statistics and Chi soiree tests were used to assess the association between the educational levels of smokers with respect to the readiness to change behavior amongst smokers.
Results
It has been observed that, Majority of the participants have not tried to quit smoking previously. 63.35% of all the participants are married. 60.85% of them have only qualified high school (Table 1). Figure 1 bar depicts the association between Readinesses to quit smoking in relation to gender. It can be observed that 52% of the males have a high readiness to quit smoking compared to 6% of the females. The X axis represents the gender of participants and the Y axis represents the % of responses of the participants. Red color represents high readiness to quit, yellow color represents average readiness to quit and Green color represents low readiness to quit smoking. The p value is 0.049 Hence it is clinically significant.
| Smoking related variables | N | Total sample% |
|---|---|---|
| Age in years | ||
| 18-25 | 43 | 27.83 |
| 26-35 | 38 | 24.28 |
| 35-45 | 32 | 20.33 |
| 46 and above | 45 | 27.56 |
| Marital status | ||
| Unmarried | 58 | 36.65 |
| Married | 100 | 63.35 |
| Educational level | ||
| Less than High School | 35 | 22.39 |
| High School | 95 | 60.85 |
| More than high school | 28 | 16.76 |
| Age at smoking initiation | ||
| <15 years | 28 | 18.29 |
| 16-18 years | 78 | 50.21 |
| >19 years | 52 | 31.5 |
| Duration of smoking | ||
| >21 years | 51 | 36.56 |
| 11-20 years | 33 | 23.81 |
| 6-10 years | 29 | 20.43 |
| 5 years or less | 45 | 19.2 |
| Number of cigarettes per day | ||
| >31 cigarettes | 16 | 11.42 |
| 21-30 cigarettes | 36 | 26.03 |
| 11-20 cigarettes | 55 | 39.73 |
| less than 10 cigarettes | 51 | 22.83 |
Table 1: Sociodemographic characteristics of current smokers (N=158)
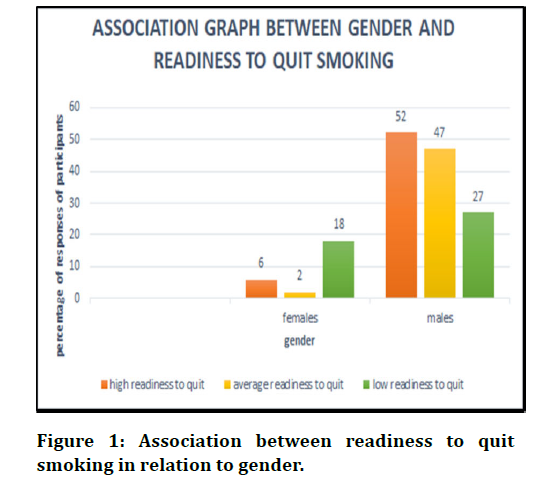
Figure 1. Association between readiness to quit smoking in relation to gender
The X axis represents the parameters for the readiness to quit smoking and the Y axis represents the percentage of study participants based on their quit scores. It was found that 42.3% of the smokers have a low readiness to quit smoking represented by Pink colour,17.5% of them are contemplating ,being represented by the Lemon Green color and 40.1% of the smokers are preparing to quit smoking which is represented by Orange color (Figure 2).
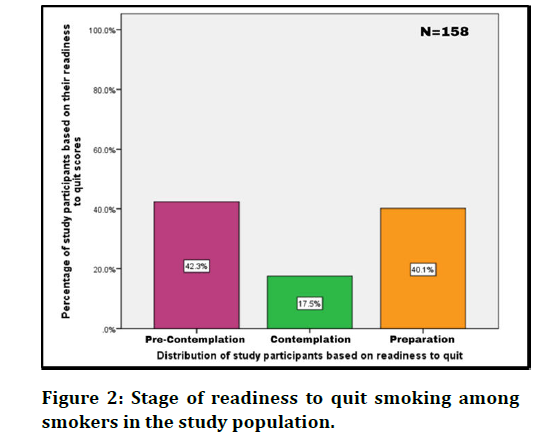
Figure 2. Stage of readiness to quit smoking among smokers in the study population.
Discussions
This study was conducted to assess the willingness to quit smoking amongst smokers in Chennai. Studies done in India and other countries [27,28]. showed that smokers who had ever attempted to quit in the past year were more likely to quit again compared with never attempting, which was concurrent with our study results showing 53.8% of the smokers who attempted to quit previously were more motivated to quit again.
This study also found that willingness to quit was significantly higher by 72.1% among those smokers who had received some form of advice to quit by the dentist (in the preceding 12 months).
This shows that dentists play a vital role in tobacco cessation and should never miss an opportunity to advise their patients who are smokers to quit smoking. Studies show that brief interventions by health practitioners are proven to reduce smoking as shown from studies in other countries [29,30].
Although some studies reported that education level was associated with increased willingness to quit smoking [31].
The facility-based cross-sectional study done in India showed that those who were less than 25 years of age were more willing to quit tobacco [30]. Another study from the United States analyzing data from the 2011 U.S.
National Health and Wellness Survey showed that those in the age group of 18–44 years were more willing to quit compared with older individuals [32,33]. These study results were concurrent with our findings.Our team has extensive knowledge and research experience that has translate into high quality publications [13,20].
Conclusion
Smoking is a major public health problem. Continued effort to control and eliminate this abuse is a medical necessity. From this study we can conclude that the majority of the smoker population have high readiness to quit smoking. Hence, more workshops on the importance of smoking cessation should be conducted.
Author Contribution
• Hooriyah: Literature search, data collection, manuscript writing.
• Pradeep Kumar: Study design, data verification, manuscript drafting.
Acknowledgement
I thank Saveetha Dental College for helping and providing support for completion of my research and the participants for their cooperation throughout the study.
Conflict of Interest
There is no conflict of interest.
Source of Funding
The Present project is supported and funded by:
• Saveetha Institute of Medical and Technical Sciences, Saveetha Dental College and Hospitals, Saveetha University.
• Maple Leaf Construction and Project’s Co. Wll.
References
- https://www.atsjournals.org/doi/book/10.1164/ajrccm-conference.2010.C054
- Humair JP. Smoking cessation in patients with mental disorders. Revue Med 2009; 5:1472-1475.
- West R, Shiffman S. Fast facts: Smoking cessation. Karger Med and Sci Publishers 2016.
- Vangeli E, Stapleton J, West R. Smoking Relapse Questionnaire [Internet]. PsycTESTS Dataset. 2013.
- Kim HJ, Kwon JH. The effects of graphic messages embedded in an anti-smoking videogame: Analyzing Singaporean University students’ knowledge improvement and attitudes toward smoking. Asian Communication Res 2017; 14:63-83.
- Mathew MG, Samuel SR, Soni AJ, et al. Evaluation of adhesion of Streptococcus mutans, plaque accumulation on zirconia and stainless steel crowns, and surrounding gingival inflammation in primary molars: Randomized controlled trial. Clin Oral Invest 2020; 24:3275-3280.
- Samuel SR. Can 5-year-olds sensibly self-report the impact of developmental enamel defects on their quality of life. Int J Paediatr Dent 2002; 285-286.
- Samuel SR, Kuduruthullah S, Al Shayeb M, et al. Impact of pain, psychological distress, Sars-cov2 fear on adults’ ohrqol during Covid-19 pandemic. Saudi J Biol Sci 2021; 28:492-494.
- Samuel SR, Kuduruthullah S, Khair AM et al. Dental pain, parental sars-cov-2 fear and distress on quality of life of 2 to 6 year-old children during covid-19. Int J Paediatr Dent 2021; 31:436-441.
- Samuel SR, Acharya S, Rao JC. School Interventionsâ??based prevention of early-childhood caries among 3â??5-year-old children from very low socioeconomic status: Two-year randomized trial. J Public Health Dent 2020; 80:51-60.
- Vikneshan M, Saravanakumar R, Mangaiyarkarasi R, et al. Algal biomass as a source for novel oral nano-antimicrobial agent. Saudi J Biol Sci 2020; 27:3753-3758.
- Chellapa LR, Rajeshkumar S, Arumugham MI, et al. Biogenic nanoselenium synthesis and evaluation of its antimicrobial, antioxidant activity and toxicity. Bioinspired Biomim Nanobiomaterials 2020; 1-6.
- Samuel SR, Mathew MG, Suresh SG, et al. Pediatric dental emergency management and parental treatment preferences during covid-19 pandemic as compared to 2019. Saudi J Biol Sci 2021; 28:2591-2597.
- Barma MD, Muthupandiyan I, Samuel SR, et al. Inhibition of Streptococcus mutans, antioxidant property and cytotoxicity of novel nano-zinc oxide varnish. Arch of Oral Biol 2021; 126:105132.
- Muthukrishnan L. Nanotechnology for cleaner leather production: A review. Environ Chem Lett 2021;1-23.
- Muthukrishnan L. Multidrug resistant tuberculosisâ??diagnostic challenges and its conquering by nanotechnology approachâ??An overview. Chem-Biol Interact 2021; 109-397.
- Sekar D, Auxzilia PK. H19 Promotes HCC bone metastasis by reducing osteoprotegerin expression in a PPP1CA/p38MAPK-Dependent Manner and Sponging miR-200b-3p. Hepatology 2021.
- Shabgah AG, Amir A, Gardanova ZR, et al. Interleukin-25: New perspective and state-of-the-art in cancer prognosis and treatment approaches. Cancer Med 2021; 10:5191.
- Kamala K, Sivaperumal P, Paray BA, et al. Identification of haloarchaea during fermentation of Sardinella longiceps for being the starter culture to accelerate fish sauce production. Int J Food Sci Technol 2021; 56:5717-5725.
- Ezhilarasan D, Lakshmi T, Subha M, et al. The ambiguous role of sirtuins in head and neck squamous cell carcinoma. Oral Dis 2021.
- Sridharan G, Ramani P, Patankar S, et al. Evaluation of salivary metabolomics in oral leukoplakia and oral squamous cell carcinoma. J Oral Pathol Med 2019; 48:299-306.
- Hannah R, Ramani P, Ramanathan A, et al. CYP2 C9 polymorphism among patients with oral squamous cell carcinoma and its role in altering the metabolism of benzo [a] pyrene. Oral Surg Oral Med Oral Pathol Oral Radiol 2020; 130:306-12.
- Pc J, Marimuthu T, Devadoss P, et al. Prevalence and measurement of anterior loop of the mandibular canal using CBCT. A cross sectional study. Clin Implant Dent Related Res 2018; 20:531-534.
- Mudigonda SK, Murugan S, Velavan K, et al. Non-suturing microvascular anastomosis in maxillofacial reconstruction: A comparative study. J Cranio Maxillofac Surg 2020; 48:599â??606.
- Wahab PA, Madhulaxmi M, Senthilnathan P, et al. Scalpel versus diathermy in wound healing after mucosal incisions: A split-mouth study. J Oral and Maxillofac Surg 2018; 76:1160-1164.
- Kiran Mudigonda S, Murugan S, Velavan K, et al. Non suturing microvascular anastomosis in maxillofacial reconstruction: A comparative study. J Cranio Maxillofac Surg 2020; 48:599-660.
- Daoud N, Hayek S, Muhammad AS, et al. Stages of change of the readiness to quit smoking among a random sample of minority Arab-male smokers in Israel. BMC public Health 2015; 15:1-3.
- Panda R, Venkatesan S, Persai D, et al. Factors determining intention to quit tobacco: Exploring patient responses visiting public health facilities in India. Tob Induc Dis 2014; 12:1-10.
- https://www.who.int/publications-detail-redirect/9789241516204
- Anczak JD, Nogler RA. Tobacco cessation in primary care: maximizing intervention strategies. Clin Med Res 2003; 1:201-216.
- McIvor A, Kayser J, Assaad JM, et al. Best practices for smoking cessation interventions in primary care. Can Respir J 2009; 129-134.
- United States. Public Health Service. Office of the Surgeon General, National Center for Chronic Disease Prevention, Health Promotion (US). Office on Smoking. Preventing tobacco use among youth and young adults: a report of the surgeon general. US Government Printing Office 2012.
- Schwartz JL. Review and evaluation of smoking cessation methods: The United States and Canada, 1978-1985. Division of Cancer Prevention and Control, National Cancer Institute, US Department of Health and Human Services, Public Health Service, National Institutes of Health; 1987.
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Indexed at, Google Scholar, Cross Ref,
Author Info
Department of Public Health Dentistry, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and technical sciences, Saveetha University, IndiaDepartment of Public Health Dentistry, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and technical sciences, Saveetha University, India
Received: 10-Jan-2022, Manuscript No. JRMDS-22-51458; , Pre QC No. JRMDS-22-51458 (PQ); Editor assigned: 12-Jan-2022, Pre QC No. JRMDS-22-51458 (PQ); Reviewed: 26-Jan-2022, QC No. JRMDS-22-51458; Revised: 31-Jan-2022 Published: 07-Feb-2022
