Review Article - (2023) Volume 11, Issue 1
Assessment of Some Properties of Heat Activated Denture Base Resin Reinforced with Strontium Titanate Nano Powder
Wisam Ahmed Shihab* and Mohammed Moudhaffer Mohammed Ali
*Correspondence: Wisam Ahmed Shihab, Department of Prosthodontics, Ashur University College, Iraq, Email:
Abstract
Introduction: In the current research, evaluation of some properties of heat cured acrylic resin were carried out after adding different concentration of strontium titanate (SrTiO3) nano powder (1% and 1.5% wt.).
Statement of the problem: Polymethyl Methacrylate (PMMA) is the most often utilized material for dentures manufacturing. Insufficient thermal conductivity, poor surface hardness, increase in roughness values and reduced some mechanical qualities make this material far from optimal in terms of justifying mechanical requirements.
Aim of the study: The goal of this research was to investigate the effects of adding SrTiO3 (NPs) nanoparticles in proportion of 1% wt. and 1.5% wt. on some physical and mechanical properties of heat cured denture base material.
Materials and methods: One hundred twenty (120) samples were divided into four groups based on the testing property, each group had 30 specimens, which were then divided into three groups: Control group, reinforced PMMA (1% wt. and 1.5% w SrTiO3 nanoparticles).
Impact strength, transverse strength, vickers hardness test and surface roughness were all tested. Additional tests include Scanning Electron Microscopy (SEM) and Fourier Transform Infrared Spectroscopy (FTIR).
Result: FTIR revealed no chemical interaction between SrTiO3 NPs and acrylic resin. The results of this study showed at 1.5% wt. SrTiO3 highly significant increase in impact strength and vickers hardness, while for transverse strength the 1% wt. showed highly significant increase while there was non-significant decrease in surface roughness.
Conclusion: The addition of SrTiO3 nanoparticles into denture base acrylic material improve impact strength, transverse strength, surface hardness values, while there was non-significant reduction in surface roughness.
Keywords
Acrylic resin, Strontium titanate (SrTiO3), Impact strength, Vickers hardness
Introduction
The fundamental purpose of dentistry is to retrieve or replace tooth structure that has been lost or destroyed, in order to meet the patient's functional and cosmetic needs. Dentures, which are produced from resin based polymeric systems, are still the most prevalent prosthetic appliance [1].
Polymethyl Methacrylate (PMMA) is a widely utilized polymer because of its optical characteristics, biocompatibility and good look, despite this, PMMA's mechanical characteristics against fatigue, impact and bending are poor, these difficulties must be addressed in order to improve the performance of PMMA as a denture base material [2].
Transverse strength is utilized more often than tensile and compressive strength measures because it strictly reflects the kind of loading that the denture is subjected to inside the mouth and is produced when stress is used in the middle of a beam that is supported at both ends [3].
A variety of strategies have been used to improve mechanical qualities, involves chemically correcting polymeric structure by the addition of specific components.
Another method for improving acrylic resin is to add particles and fibers. Fillers of micrometer and nano scale size are commonly added to polymers to increase stiffness and strength, improve solvent resistance, or lower costs [4].
It was found that adding nanoparticles as a reinforcing agent affects the physical properties of acrylic resins [5]. The chemical formula of strontium titanate (SrTiO3) is an oxide of strontium and titanium. It's a popular material for super conductors and thin oxide sheets. Strontium titanate nano powder can be used in making scaffolds for bone regeneration [6].
Materials and Methods
In this study, strontium titanate nano powder (nano shel, USA) (average particle size 80-100 nm) and heat cure acrylic resin (Kulzer, Germany) were used.
Pilot study
Various weight concentrations (0.5%, 1%, 1.5% and 2 %) of SrTiO3 were incorporated into heat cure acrylic resin; impact strength and transverse strength were compared. As a result, the weight percentages of 1% and 1.5% were chosen because they presented the best behavior.
Specimen grouping
In this research, a total of 120 samples were prepared. According to the tests employed, the samples were divided into four different groups, with each test containing 30 samples that were further subdivided into three groups:
• 10 samples of acrylic resin without SrTiO3 nanoparticles as a control group.
• 10 samples of acrylic resin with 1% SrTiO3 nanoparticles.
• 10 samples of acrylic resin with 1.5% SrTiO3 nanoparticles.
Mold fabrication
Different plastic patterns were created to build molds for study samples. These models were completed by laser cutting a plastic plate into the correct form and dimension based on the test specifications. The mold is then prepared in the same way that complete dentures are processed to manufacture acrylic specimens. The separating medium (cold mold seal) is applied to the plastic patterns and allowed to dry. The dental stone is combined according to the manufacturer's instructions (100 g powder to 20 ml water) and poured into the flask's lower half, which is then vibrated to remove any air bubbles. The patterns were inserted about halfway into the stone, which was then dried. This is followed by covering the lower half was covered with separating material and let to dry, at that moment the upper half has been put and filled with stone and it has been vibrated and finally the flask's lid is placed and left to dry. After the stone has set, the two halves of the flasks are split and the plastic patterns were detached to produce a mold hole for the acrylic specimen. The separating media is then applied and allowed to dry and the flask is ready to pack the acrylic specimen in the traditional fashion.
The tests that were carried out during the research
A-Transverse strength
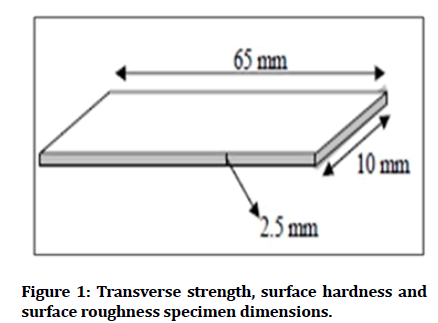
Test specimen: The dimensions of the specimens utilized in this test were (65 mm x 10 mm x 2.5 mm) (Figure 1). Before being tested, all specimens were maintained in distilled water at 37°C for 48 hours [7].
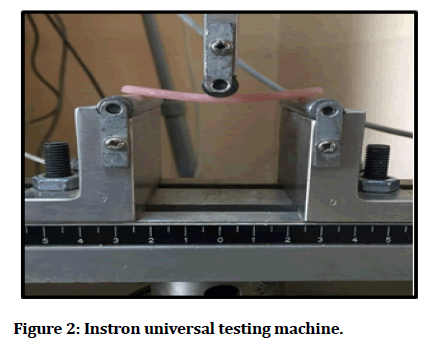
Test procedure: An instron testing machine WDW-200 E (UK) (Figure 2). The specimens were place on bending fixtures made of two parallel supports (50 mm) apart, and the load was applied at a rate of 1 mm/min through a rod that was positioned in the middle of the supports to cause deflection until fracture occurred. The transverse strength was determined using the formula below (1):
T=3PL/2bd2……… (1)
Where,
T: Transverse strength (N/mm2); P: Maximum load applied on sample (N); L: Distance between supports (mm); b: Width of specimens (mm); d: Depth of specimens (mm).
Impact strength
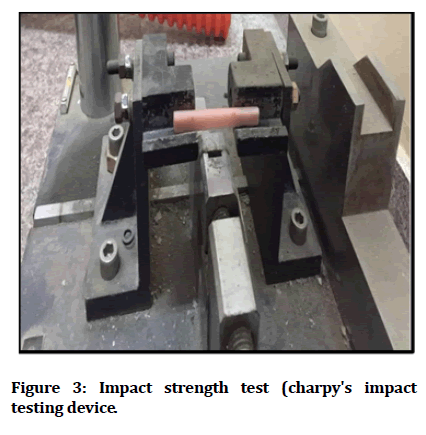
Test specimens: For the impact strength test, acrylic resin specimens with dimensions of (80 mm x 10 mm x 4 mm) were made. The impact strength test was carried by using charpy's impact testing device (testing machines Inc., USA) (Figure 3) and in accordance with the procedure recommended by ISO 179-1: 2000.
Each specimen was held horizontally at both end and stuck with a pendulum of 2 Joules (TMI, testing machine Inc., Amity Vielle, New York, USA). The impact energy was measured in Joules (Figure 3).
The impact strength was calculated in Joules per square meter by the following formula (2):
Impact Strength= (E/bd) × 103…… (2)
Where,
E: The impact energy in Joules; b: The width of specimens in millimeters; d: The depth of specimens in millimeters.
Surface roughness
Test specimen: For the surface roughness test, test specimens of acrylic resin were made with dimensions of (65 mm x 10 mm x 2.5 mm) as shown in Figure 1.
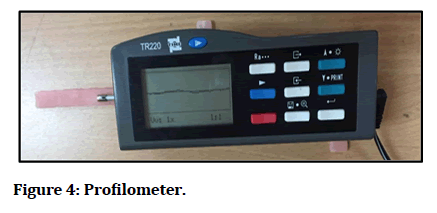
Testing procedure: Profilometer (TEREN, DaLian, China) was used to investigate the micro geometry of test specimens). This apparatus uses a surface contact analyzer (a diamond tipped stylus) to track the progression of surface imperfections (Figure 4). The stylus can capture all peaks and recesses at a maximum distance of 11 mm. The specimens were divided into three regions and the analyzer was moved along the tested area to calculate the average of three readings.
Vickers hardness tests
Test specimen: The specimens utilized in this study were tested with the following dimensions (65 mm length x 10 mm width x 2.5 mm thickness) as shown in Figure 1.
Figure 1: Transverse strength, surface hardness and surface roughness specimen dimensions.
Figure 2: Instron universal testing machine.
Figure 3: Impact strength test (charpy's impact testing device.
Figure 4: Profilometer.
Testing procedure: All imperfections were eliminated with a tungsten carbide bur after the specimens were prepared. The samples were polished and placed in distilled water to keep them clean and ready to testing.
The vickers hardness test was performed with laryee hvs-5 (manufacturing limited, beijing, China) (Figure 5). Vickers hardness testing was performed on the specimens with a 25 g load for 30 seconds. Penetration was found in three locations. The average of three readings was determined, with one in the middle and two on either end.
Figure 5: Vickers hardness test.
The statistical analysis: One way ANOVA (Analysis of Variance) and post hoc test (Tukey HSD) software (IBM SPSS Statistics 26 were used in the statistical analysis).
The Probability (P) value of >0.05 were considered statistically Non-Significant (NS), P values of ≤ 0.05 were considered Statistically significant (S) and P values of ≤ 0.01 were considered Highly Significant (HS).
Results
FTIR: The FTIR results of the strontium titanate oxide nano filler powder and the heat cure acrylic resin before and after addition of SrTiO3 Nano fillers are shown respectively in Figures 6 and 7. The FTIR results revealed no structural differences between the specimens before and after the addition of SrTiO3.
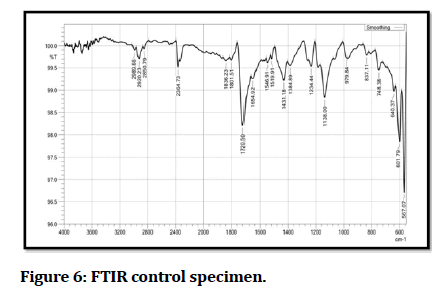
Figure 6: FTIR control specimen.
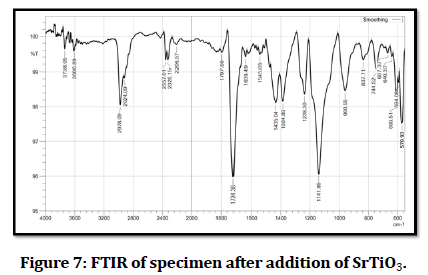
Figure 7: FTIR of specimen after addition of SrTiO3.
However, little changes are found which might be related to alterations in the polymerization process.
Scanning Electron Microscope (SEM test
The surface of control and additive samples of impact strength test specimen was examined by SEM with different magnifications power to evaluate dispersions of nanoparticles in the resin matrix as seen in Figure 8. The SEM images showed well dispersion of SrTiO3 NPs inside the acrylic resin with some aggregation (yellow arrows) as the filler content increases as shown in Figure 8.

Figure 8: Scanning electron microscope, A) PMMA without nanoparticles; B)PMMA with nanoparticle; C) PMMA with nanoparticle.
Mechanical tests results
Impact strength: The highest mean value of impact strength is related to 1.5% wt. group, while the mean value of control group was the lowest value. Tukey test revealed highly significant difference between all tested groups (Table 1).
| Impact strength | ANOVA | Tukey HSD | ||||||
|---|---|---|---|---|---|---|---|---|
| Group | Min | Max | Mean | ± SD | F | P value | Groups | P value |
| Control (A) | 9.32 | 11.50 | 10.555 | 0.6467 | 60.515 | 0.000 | AB | 0.000 |
| 1% (B) | 11.22 | 13.82 | 12.531 | 0.7017 | AC | 0.000 | ||
| 1.5% (C) | 12.96 | 14.33 | 13.554 | 0.4914 | BC | 0.003 | ||
| Levene statistics=0.259, p value=0.774 (NS). | ||||||||
Table 1: Descriptive statistics, one way ANOVA and Tukey’s HSD of impact strength.
Transverse strength test: The highest mean value is present in 1% wt. SrTiO3, while the lowest mean value is for control group (Table 2). There was highly significant difference between groups (A) and (B), groups (B) and (C). While non-significant difference was found between groups (A) and group (B).
| Transverse strength | ANOVA | Tukey HSD | ||||||
|---|---|---|---|---|---|---|---|---|
| Group | Min | Max | Mean | ± SD | F | P value | Groups | P value |
| Control (A) | 77.43 | 87.14 | 81.133 | 2.8541 | 12.756 | 0.000 | AB | 0.000 |
| 1% (B) | 81.79 | 92.74 | 86.886 | 3.3720 | AC | 0.694 | ||
| 1.5% (C) | 79.31 | 84.90 | 82.131 | 1.6459 | BC | 0.002 | ||
| Levene statistics=2.164, p value=0.134 (NS). | ||||||||
Table 2: Descriptive statistics, one way ANOVA and Tukey’s HSD of transverse strength.
Vickers hardness test: The highest mean value is 1.5% wt. SrTiO3 group, while the lowest value for control group. There was highly significant difference between all of the groups (Table 3).
| Vickers micro hardness | ANOVA | Tukey HSD | ||||||
|---|---|---|---|---|---|---|---|---|
| Group | Min | Max | Mean | ± SD | F | P value | Groups | P value |
| Control (A) | 15.02 | 17.70 | 16.365 | 0.7721 | 47.117 | 0.000 | A B | 0.000 |
| 1% (B) | 18.23 | 20.60 | 19.171 | 0.7961 | A C | 0.000 | ||
| 1.5% (C) | 18.87 | 22.46 | 20.565 | 1.2975 | B C | 0.010 | ||
| Levene statistics=2.307, p value=0.119 (NS) | ||||||||
Table 3: Descriptive statistics, one way ANOVA and Tukey’s HSD of Vickers hardness.
Surface roughness test: The control group showed the highest mean value, while 1.5% wt. Nano SrTiO3 showed the lowest mean value (Table 4).
| Surface roughness test | ANOVA | |||||
|---|---|---|---|---|---|---|
| Group | Min | Max | Mean | ± SD | F | P value |
| Control (A) | 0.97 | 1.82 | 1.4344 | 0.24105 | 0.781 | 0.468 |
| 1% (B) | 1.16 | 1.71 | 1.3862 | 0.1575 | ||
| 1.5% (C) | 1.05 | 1.76 | 1.3232 | 0.19107 | ||
| Levene statistics=2.307, p value=0.119 (NS) | ||||||
Table 4: Descriptive statistics, one way ANOVA and Tukey’s HSD of surface roughness.
Discussion
The study's findings revealed that the 1.5% wt. group had the highest impact strength value when compared to the 1% wt. and control groups. This is because the new combination (SrTiO3+PMMA), enhance the internal resistance due to force exchange between matrix and filler. The applied pressures re also transferred to the nanoparticles, increasing the impact strength [8]. Furthermore, the compound stress strain behavior is influenced by particle size and bonding interaction [9]. The addition of SrTiO3 nano fillers to the acrylic resin may cause limitation the mobility and deformation of the matrix by introducing a mechanical restriction. This result was in agreement with Safi who incorporated ZrO2 nano fillers into heat cured (PMMA) [10].
In the transverse strength, it was found that (1% and 1.5% group higher than control group) because of the use of nanoparticles reduces the free space distance between polymer chains during the curing process, resulting in more complex network chain [11,12]. The increase in transverse strength with SrTiO3 Nano filler could be attributable to stress transference from the more flexible polymers to the high modulus (more rigid and stiffer) filler particles [13].
For the hardness test, the polymer is strengthened with SrTiO3 showed higher surface hardness may be due to good distribution in the resin matrix, the distance between the particles inside the matrix will be decreased [14]. The bonding strength between the particles rises as the inter particle distance decreases, causing hard material particles SrTiO3 to accumulate on the surface of the acrylic matrix spaces, resulting in better hardness behavior [15]. The improved hardness could be attributed to better nano filler dispersion in the resin matrix and the buildup of SrTiO3 nano particles, a hard material, in the polymer matrix. The 1.5% wt. Nano SrTiO3 increased in hardness more than the 1% wt. nano SrTiO3 due to higher nano filler accumulation in the resin matrix [16].
Finally, for surface roughness test, non-significant change with different percentages of added SrTiO3 nanoparticles and this may be due to that the SrTiO3 nanoparticles have very small size, also, because the surface roughness test is concerned with the outer surface of the nano composite rather than the inner surface, just a few particles were implicated on the surface of the specimens when a tiny fraction of nanoparticles was added to the acrylic resin [17,18].
Conclusion
Within the limitation of this study, it can be concluded that, the impact strength, transverse strength and surface hardness were significantly increase in the reinforced SrTiO3 group while surface roughness of acrylic denture base reinforced by SrTiO3 nanoparticles showed nonsignificant decrease among the study groups.
References
- Ismail IJ, Muklif OR. Studying the effect of addition a composite of silanized nano-Al2O3 and plasma treated polypropylene fibers on some physical and mechanical properties of heat cured PMMA denture base material. J Baghdad Coll Dent 2015; 27:22-27. [Googlescholar][Indexed]
- Bettencourt AF, Neves CB, de Almeida MS, et al. Biodegradation of acrylic based resins: A review. Dent Mater 2010; 26:e171-80. [Crossref][Googlescholar][Indexed]
- Sakaguchi RL, Powers JM. Craig's restorative dental materials e-book. Elsevier Health Sciences 2012. [Crossref][Googlescholar][Indexed]
- Nejatian T, Johnson A, Van Noort R. Reinforcement of denture base resin. Adv Sci Technol Trans Tech Pub 2006; 49:124-129. [Crossref][Googlescholar][Indexed]
- Sodagar A, Bahador A, Khalil S, et al. The effect of TiO2 and SiO2 nanoparticles on flexural strength of poly (methyl methacrylate) acrylic resins. J Prosth Res 2013; 57:15–19. [Crossref][Googlescholar][Indexed]
- Nanoshel. Strontium titanate nanoparticles. Nanopowder compounds, Nanoshel UK limited, 2021.
- Studying the effect of addition a composite of silanized nano-Al2O3 and plasma treated polypropylene fibers on some physical and mechanical properties of heat cured PMMA denture base material
- Sun L, Ronald FG, Suhr J, et al. Energy absorption capability of nano composites: A review. Composites Sci Technol 2009; 69:2392-2409. [Crossref][Googlescholar][Indexed]
- Tanasa F, Zanoaga M, Darie R. Evaluation of stress strain properties of some new polymer clay nano composites for aerospace and defense applications. Int Sci Committee 2014; 241. [Googlescholar][Indexed]
- Ihab NS, Moudhaffar M. Evaluation of the effect of modified nano fillers addition on some properties of heat cured acrylic denture base material. J Bagh Coll Dent 2011; 23:23-29. [Googlescholar][Indexed]
- Ke YC, Stroeve P. Polymer layered silicate and silica nano composites. Elsevier, St. Louis, 2005; 120–201. [Googlescholar]
- Katsikis N, Franz Z, Anne H, et al. Thermal stability of PMMA/silica nano and micro composites as investigated by dynamic mechanical experiments. Polym Degrad Stab 2007; 22:1966-1976. [Crossref][Googlescholar][Indexed]
- Anusavice KJ. Philips science of dental material. 11th edition, Middle east and African edition, 2008; 7:143-166,721-756. [Crossref][Googlescholar][Indexed]
- Zakaria ZK, Nezhad KS. The effects of interphase and interface characteristics on the tensile behavior of POM/CaCO3 nano composites. Nanomater Nanotechnol 2014; 4:17. [Crossref][Googlescholar][Indexed]
- Antil P, Singh S, Manna A. Effect of reinforcing silicon carbide particulates on mechanical properties of polymer matrix composite. National conference on recent advances in mechanical engineering India, 2017.
- Hudson LK, Misra C, Perrotta AJ, et al. Aluminum oxide. Ullmann's encyclopedia of industrial chemistry 2000. [Crossref]
- Al-Momen MM. Effect of reinforcement on strength and radiopacity of acrylic denture base material. A master thesis, Department of Prosthodontics, University of Baghdad 2000.
- Plastics-determination of charpy impact properties-part 1: Non-instrumented impact test. ISO 179-1, 2010.
Author Info
Wisam Ahmed Shihab* and Mohammed Moudhaffer Mohammed Ali
Department of Prosthodontics, Ashur University College, IraqCitation: Wisam Ahmed Shihab, Mohammed Moudhaffer Mohammed Ali, Assessment of Some Properties of Heat Activated Denture Base Resin Reinforced with Strontium Titanate Nano Powder, J Res Med Dent Sci, 2023, 11 (01): 132-137.
Received: 03-Nov-2022, Manuscript No. JRMDS-22-71567; , Pre QC No. JRMDS-22-71567; Editor assigned: 08-Nov-2022, Pre QC No. JRMDS-22-71567; Reviewed: 22-Nov-2022, QC No. JRMDS-22-71567; Revised: 02-Jan-2023, Manuscript No. JRMDS-22-71567; Published: 09-Jan-2023