Research - (2020) Volume 8, Issue 6
Association between Ischemic Heart Disease and Dyslipidemia Among Adult Hypertensive Patients- A Case-Control Study in Kingdom of Saudi Arabia
Abo Bakr Omar Hussain1, Mahmoud Hassan EL-Bidawy2,3, Mamdouh Ali Kotb4,5, Mohammed Ahammed Noureddin6*, Ali Hassan A Ali7,8 and Ramadan S Hussein9
*Correspondence: Mohammed Ahammed Noureddin, Department of Internal Medicine, College of Medicine, Prince Sattam Bin Abdul-Aziz University, Saudi Arabia, Email:
Abstract
Background: Hypertension is a major health problem, affecting a large population across the world. Approximately 7.5 million people die of hypertension every year worldwide.
Objective: To determine the association between Ischemic Disease Heart (IHD) and dyslipidemia among hypertensive patients.
Methods: A case-control study was conducted at the cardiology outpatient departments of Prince Sattam-Bin-Abdul-Aziz University hospital between September 2015 and February 2017. The association of ischemic heart disease (dependent variable) was assessed against dyslipidemia (independent variable). Ischemic heart disease (IHD), body mass index (BMI) and dyslipidemia were defined. The data from the patients were collected into the medical notes that were later transferred into an excel spreadsheet. The data was analyzed using SPSS version 23. Pearson's chi-square test was applied and a P-value of ≤ 0.05 was considered significant.
Results: A total of 160 respondents were included in the study and 39.4% (n=63) had a positive history of ischemic heart disease. The average age in our study population was 49.16 ± 11.7 and average BMI was 29.11 ± 5.04. A significant correlation was noted between dyslipidemia and IHD (p=0.000; OR 3.39). It was noted that the chances of IHD with dyslipidemia were higher among individuals in the 31-50 years age group (p=0.001; OR 6.75). In addition, a statistically significant correlation was noted between the risk of IHD and dyslipidemia in overweight and obese patients.
Conclusion: The combination of hypertension and dyslipidemia is a significant risk of IHD for male gender, 31-50 years old, overweight, obese, diabetics or smokers.
Keywords
Dyslipidemias, Myocardial ischemia, Coronary artery disease, Saudi Arabia
Introduction
Hypertension (HTN) or elevated blood pressure is an important non-communicable disease (NCD) which considered as one of the strongest risk factors for cardiovascular diseases (CVDs) including ischemic heart disease (IHD), left ventricular hypertrophy (LVH) and heart failure, cerebrovascular attack, peripheral arterial disease (PAD) and renal failure [1]. Globally, 1.13 billion adults suffer from HTN and 7.5 million people die of it every year [2,3]. Coronary artery disease (CAD) or IHD is one of the major CVDs, contributing to nearly 7.4 million annual deaths worldwide [4]. There are several risk factors involved in the pathogenesis of IHD including modifiable and non-modifiable risk factors. Modifiable risk factors of IHD include unhealthy lifestyle (i.e., poor diet or bad fats, stress, obesity, physical inactivity, sleep deprivation, smoking, alcohol and substance abuse), diabetes, hyperlipidemia, high blood pressure and poor socio-economic status while non-modifiable risk factors include family history of IHD, old age, gender, ethnicity and menopause [5,6].
Dyslipidemia is a highly prevalent but modifiable risk factor for IHD and other cardiovascular events [7]. The global prevalence of raised total cholesterol is 39%, accounting for 2.6 million annual deaths worldwide [8]. More than 50% of patients with IHD have coexistent dyslipidemia while alone hypercholesterolemia accounts for one-third of IHD worldwide [9,10]. Both HTN and dyslipidemia are major and established risk factors for CVDs or IHD. There has been a significant relationship found between dyslipidemia and incidence of IHD among hypertensive patients. It has been reported that hypertensive patients with dyslipidemia develop IHD 18 times greater than those without dyslipidemia [9]. Therefore, coexistence of HTN and hyperlipidemia accelerates atherosclerosis, leading to increased incidence of CAD or IHD [9]. Atherosclerosis plays a main role in the pathogenesis of IHD through the formation of atherosclerotic plaques.
In Saudi Arabia, hypertension is one of the leading causes of death with overall prevalence of 4.9% in the country [11]. Similarly, the prevalence of HTN among the population suffering from CVDs is 31.4% [11]. As far as dyslipidemia is concerned, its prevalence has been reported to be 33% in Saudi population [12]. These statistics reflect that there is substantial risk of IHD existing in Saudi population in the form of hypertension and dyslipidemia. If other risk factors of IHD such as old age, gender, obesity, diabetes and smoking are considered, it will further add to the risk of incidence of IHD or CAD in Saudi population. In other words, the risk of CAD development rises as the number of risk factors increases. In addition, modifiable risk factors are highly prevalent in Saudi Arabia, adding to the risk of IHD. Moreover, studies on the determination of the number of risk factors for IHD and their cumulative effect on the incidence of other CVDs among Saudi individuals is lacking. Unfortunately, lack of awareness about substantial risk factors of CAD or IHD among Saudi individuals is upsetting and requires mass awareness campaigns [13].
The literature on association between dyslipidemia and IHD is scars from Saudi Arabia. Therefore, this case control study was carried out to determine the association between IHD and dyslipidemia among hypertensive patients.
Methodology
This case-control study was conducted at the cardiology outpatient departments of Prince Sattam Bin Abdul-Aziz University hospital between September 2015 and February 2017. Written consent was obtained from the patient and the study was approved by the ethics approval committee of the concerned hospital. The association of ischemic heart disease (dependent variable) was assessed against dyslipidemia (independent variable). Other confounding variables assessed were history of hypertension, sex, age, weight status, diabetes (based on the history of diagnosed diabetes or taking anti-diabetes medication), and history of smoking.
The inclusion criteria included patients with a history of primary hypertension; adults of both genders and aged 18 years or more, patients with varying BMIs (from underweight to obese); both diabetics and non-diabetics; smokers and non-smoker; and patients presenting in the outpatients who consented to participate in the study. Patients without the history of established hypertension or who had secondary hypertension; children and adolescents; inpatients, and outpatients who did not consent to participate were excluded from the study.
The variables included in the study were defined as follows.
Ischemic heart disease: The patients were labeled to have ischemic heart disease if they had a positive history of either myocardial infarction, coronary angioplasty or coronary artery bypass surgery, positive stress electrocardiogram, or angiographic evidence of luminal narrowing of coronary arteries or ischemic changes evident on an electrocardiogram with a positive history of chest pain and raised cardiac enzymes (including troponin) levels.
BMI: It was calculated after assessing patients’ height and weight and patients were classified into underweight, normal, obese, and overweight categories (obesity stages as defined by the Center for Disease Control and Prevention).
Blood pressure: It was assessed on two separate instances during the clinic appointment using a mercury sphygmomanometer. The blood pressure was divided into three stages: (a) Stage 1- Clinic blood pressure 140/90 mmHg to 159/99 mmHg; (b) Stage 2- Clinic blood pressure 160/100 mmHg or higher less than 180/120 mmHg, and (c) Stage 3- Clinic systolic blood pressure greater than 180 mmHg.
Dyslipidemia: It was established following a complete lipid profile from the patients. The levels of LDL, HDL, triglycerides and cholesterol were interpreted based on the American College of Cardiology guidelines.
The sample size was calculated using an Openepi sample calculator where confidence level was set at 95%, power was 80%, frequency of dyslipidemia in cases of IHD was set as 17.3% and in controls it was set as 50%. The computed results gave us a sample size of 160 with 63 cases and 97 controls. The data from the patients was collected into the medical notes that were later transferred retrospectively into an excel spreadsheet. The data was analyzed using SPSS version 23 and descriptive statistics were computed for study variables. Pearson's chi-square test was applied and a P-value of ≤ 0.05 was considered significant. Odds ratios with (95% CI) were calculated to check the association between dyslipidemia and IHD and OR>1 was considered as significant. The results were represented as tables and figures.
Results
Out of the 160 respondents, 39.4% (n=63) had a positive history of ischemic heart disease. The average age in our study population was 49.16 ± 11.7 and average BMI was 29.11 ± 5.04 (Figure 1). Majority of our population were males (n=90; 56.2%), were above 50 years (n=77; 48.1%), were obese (n= 93; 58.1%), had stage one hypertension (n=102; 63.7%), were nondiabetics (n=90; 56.2%), and non-smokers (n= 131; 81.9%). Table 1 describes the demographics and distribution of confounding variables among the study population in detail.
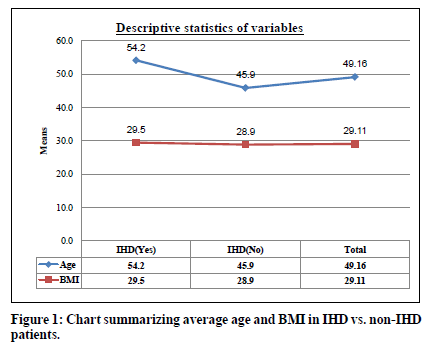
Figure 1. Chart summarizing average age and BMI in IHD vs. non-IHD patients.
| Associated Variables | IHD | Total | P Values | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| Age groups | 30 or less years | 0 | 14 | 14 | 0.002* |
| 0.00% | 14.40% | 8.80% | |||
| 31-50 years | 25 | 44 | 69 | ||
| 39.70% | 45.40% | 43.10% | |||
| More than 50 years | 38 | 39 | 77 | ||
| 60.30% | 40.20% | 48.10% | |||
| Gender | Female | 25 | 45 | 70 | 0.403 |
| 39.70% | 46.40% | 43.80% | |||
| Male | 38 | 52 | 90 | ||
| 60.30% | 53.60% | 56.20% | |||
| BMI | Underweight | 2 | 11 | 13 | 0.3 |
| 3.20% | 11.30% | 8.10% | |||
| Normal | 8 | 9 | 17 | ||
| 12.70% | 9.30% | 10.60% | |||
| Overweight | 15 | 22 | 37 | ||
| 23.80% | 22.70% | 23.10% | |||
| Obese | 38 | 55 | 93 | ||
| 60.30% | 56.70% | 58.10% | |||
| Stage of HTN | Stage 1 | 11 | 91 | 102 | <0.000* |
| 17.50% | 93.80% | 63.70% | |||
| Stage 2 | 44 | 0 | 44 | ||
| 69.80% | 0.00% | 27.50% | |||
| Stage 3 | 8 | 6 | 14 | ||
| 12.70% | 6.20% | 8.80% | |||
| Diabetes Mellitus | Yes | 51 | 19 | 70 | <0.000* |
| 81.00% | 19.60% | 43.80% | |||
| No | 12 | 78 | 90 | ||
| 19.00% | 80.40% | 56.20% | |||
| Smoking | Yes | 18 | 11 | 29 | 0.006* |
| 28.60% | 11.30% | 18.10% | |||
| No | 45 | 86 | 131 | ||
| 71.40% | 88.70% | 81.90% | |||
Table 1: Distribution of study variables according to IHD.
We noted a significant correlation between dyslipidemia and IHD (p= 0.000; OR 3.39 (95% CI: 1.72-6.62)) (Figure 2). When the association between IHD and dyslipidemia was assessed based on the patient’s characteristics, we noted several trends (Table 2 summarizes these trends). We noted that the chances of IHD with dyslipidemia were higher among individuals in the 31-50 years age group (p= 0.001; OR 6.75 (95% CI 2.23-20.44)). There was no statistically significant correlation between these variables in the remaining age groups. Although both genders had an increased risk of IHD with dyslipidemia, this risk was higher among males than females (p= 0.003; OR 3.63 (95% CI 1.51- 8.67) in males vs. p= 0.051; OR 3.05l (95% CI 0.97-9.62) in females).
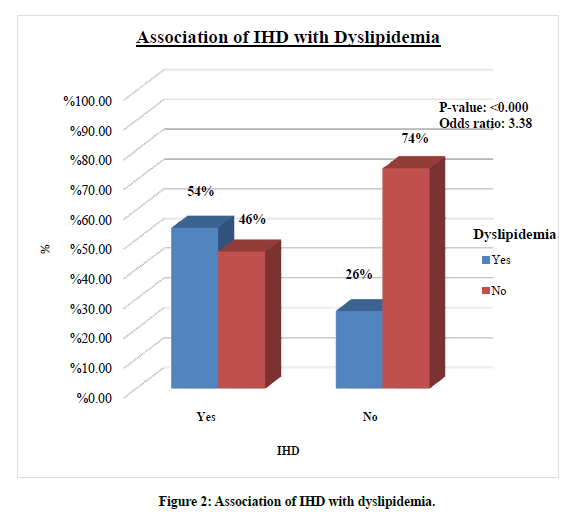
Figure 2. Association of IHD with dyslipidemia.
| Associated variables | Dyslipidemia | IHD | P values | Odds ratio (95% CI) | ||
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Age groups | 30 or less years | Yes | 0(0%) | 1(100%) | N/A | N/A |
| No | 0(0%) | 13(100%) | ||||
| 31-50 years | Yes | 15(65.2%) | 8(34.8%) | 0.001* | 6.75 (2.23-20.44) | |
| No | 10(21.7%) | 36(78.3%) | ||||
| More than 50 years | Yes | 19(54.3%) | 16(45.7%) | 0.429 | 1.44 (0.58-3.54) | |
| No | 19(45.2%) | 23(54.8%) | ||||
| Gender | Female | Yes | 9(56.2%) | 7(43.8%) | 0.051* | 3.05 (0.97-9.62) |
| No | 16(29.6%) | 38(70.4%) | ||||
| Male | Yes | 25(58.1%) | 18(41.9%) | 0.003* | 3.63 (1.51-8.67) | |
| No | 13(27.7%) | 34(72.3%) | ||||
| BMI | Underweight | Yes | 0(0%) | 4(100%) | 0.305 | N/A |
| No | 2(22.2%) | 7(77.8%) | ||||
| Normal | Yes | 8(66.7%) | 4(33.3%) | 0.012* | N/A | |
| No | 0(0%) | 5(100%) | ||||
| Overweight | Yes | 8(80%) | 2(20%) | 0.003* | 11.43 | |
| No | 7(25.9%) | 20(74.1%) | (1.94-67.26) | |||
| Obese | Yes | 18(54.5%) | 15(45.5%) | 0.046* | 2.4 (1.0-5.73) | |
| No | 20(33.3%) | 40(66.7%) | ||||
| Stages of Hypertension | Stage 1 | Yes | 7(26.9%) | 19(73.1%) | 0.002* | 6.63 (1.76-25.04) |
| No | 4(5.3%) | 72(94.7%) | ||||
| Stage 2 | Yes | 19(100%) | 0(0%) | N/A | N/A | |
| No | 25(100%) | 0(0%) | ||||
| Stage 3 | Yes | 8(57.1%) | 6(42.9%) | N/A | N/A | |
| No | 0(0%) | 0(0%) | ||||
| Diabetes Mellitus | Yes | Yes | 23(92%) | 2(8%) | 0.007* | 6.98 (1.46-33.41) |
| No | 28(62.2%) | 17(37.8%) | ||||
| No | Yes | 11(32.4%) | 23(67.6%) | 0.000* | 26.3 (3.21-215.7) | |
| No | 1(1.8%) | 55(98.2%) | ||||
| Smoking | Yes | Yes | 13(81.3%) | 3(18.8%) | 0.018* | 6.93 (1.29-37.22) |
| No | 5(38.5%) | 8(64.5%) | ||||
| No | Yes | 21(48.8%) | 22(51.2%) | 0.015* | 2.55 (1.19-5.44) | |
| No | 24(27.3%) | 64(72.7%) | ||||
Table 2: Association of IHD with Dyslipidemia according to patient’s characteristics.
We also noted a statistically significant correlation between the risk of IHD and dyslipidemia in overweight and obese patients. In overweight patients, the OR was 11.45 (95% CI 1.94-67.26) and p-value was 0.003. In the obese population, statistical significance was achieved with a p-value of 0.046 (OR 2.4 (95% CI 1.0-5.73)). A statistically significant correlation was only noted in patients with stage I hypertension (p= 0.002; OR 6.65 (95%CI 1.76- 25.03)). Other stages of hypertension did not reach statistical significance. As for diabetes, we noted a statistically significant risk of IHD with dyslipidemia with both diabetics and nondiabetic patient (p=0.007, OR 6.98 (95% CI 1.46- 33.41)) in diabetics vs. p= 0.000, OR 26.30 (95% CI 3.21-215.7) in non-diabetics). The IHD risk with dyslipidemia was high in both smoker and non-smoker patient populations with p-values 0.018 (OR 6.93 (95% CI 1.29-37.22) and 0.015 (OR2.55 (95% CI 1.19-5.44) in smoking and nonsmoking patients respectively.
Discussion
The present case-control study revealed a significant correlation between dyslipidemia and IHD. Besides this correlation, male gender, age (31-50 years), overweight, obesity, stage one hypertension, diabetics or non-diabetics, smokers or non-smokers had significant correlation with IHD in the presence of dyslipidemia. Interestingly, the study did not reveal statistically significant correlation of stages two and stage three hypertension with IHD in the presence of dyslipidemia.
Hypertension and dyslipidemia are leading independent risk factors of CVDs as well as key components of metabolic syndrome which further increase the risk of CV events. Coexistence of hypertension and dyslipidemia poses even more adverse impact on cardiovascular functions through endothelial dysfunction, heightened oxidative stress and accelerated atherosclerosis [14]. A study from China, conducted by Yu et al. [15] has reported high prevalence of dyslipidemia (68.7%). Similarly, Spannella et al. [16] conducted an observational study in Italy including 1219 outdoor patients, reporting the prevalence of dyslipidemia as high as 91.1% among those who were referred for the management of hypertension. Unfortunately, dyslipidemia is often neglected in hypertensive patients. Jani et al. [17] conducted a prospective cross sectional including 600 patients suffering from hypertension and diabetes. They reported insufficiently treated dyslipidemia in patients with controlled and uncontrolled hypertension as 23% and 67%, respectively. It has been reported that effective treatment of hypertension alone and hypertension plus hypercholesterolemia reduces CVD risk by 20- 25% and >50%, respectively [16]. Therefore, proper control of high blood pressure and dyslipidemia significantly reduces the risk of IHD and other CVDs.
Similarly, presence of other risk factors such as male gender, age (31-50 years in the present study), obesity, diabetics and smoking along with dyslipidemia and hypertension adds to the risk of CVDs. For instance, post-MI morbidity, mortality and re-infarction are higher among diabetics as compared to non-diabetics [18]. Like hypertension and dyslipidemia, diabetes is also an independent risk factor of CVD. Therefore, coexistence of these three risk factors intensifies the risk of CV events. The present study has revealed a significant correlation with IHD among those patients with hypertension stage 1 as reported in previous studies [19,20]. Interestingly, Qi et al. [19] and Talaei et al. [20] have reported significant correlation of hypertension stage 1 with CVDs among young and middle-aged patients (<65 years), not in those above 65 years. In the present study, more patients were having dyslipidemia at hypertension stages two and three, posing more risk of developing IHD and its complications. In this context, Wu et al. [21] has reported higher CVD mortality among those patients with hypertension stages two and three as compared to those with hypertension stage one. Proper control of hypertension among young patients at stage one helps reduce cardiovascular risk.
The present study reveals that combination of dyslipidemia and hypertension is a significant risk for the development of IHD even among nondiabetics and non-smokers. Limitations of the study include single-centered study and small sample size. As dyslipidemia and hypertension are common risk factors for IHD, large sample size from multiple centers could have offered more precise results.
Conclusion
The combination of hypertension and dyslipidemia is a significant risk of IHD for male gender, 31-50 years old, overweight, obese, diabetics or smokers. In this context, risk of IHD can be cut down significantly by optimizing the treatment of hypertension and diabetes, reduction of weight and dyslipidemia, and smoking cessation. In fact, large benefits can be gained by addressing multiple risk factors of IHD simultaneously.
Acknowledgments
This publication was supported by the Deanship of scientific research at Prince Sattam bin Abdul Aziz University, Al-Kharj, Saudi Arabia.
References
- Kjeldsen SE. Hypertension and cardiovascular risk: general aspects. Pharmacol Res 2018; 129:95-99.
- Barrera L. High blood pressure prevention and control: From evidence to action. Colomb Med 2018; 49:137–138.
- Singh S, Shankar R, Singh GP. Prevalence and associated risk factors of hypertension: A cross-sectional study in Urban Varanasi. Int J Hypertens 2017; 2017:5491838.
- Shahwan AJ, Abed Y, Desormais I, et al. Epidemiology of coronary artery disease and stroke and associated risk factors in Gaza community–Palestine. PLoS One 2019; 14:e0211131.
- Mirzaeipour F, Seyedmazhari M, Pishgooie AH, et al. Assessment of risk factors for coronary artery disease in military personnel: A study from Iran. J Family Med Prim Care 2019; 8:1347–1351.
- Hajar R. Risk factors for coronary artery disease: Historical perspectives. Heart Views 2017; 18:109–114.
- Narindrarngkura P, Bosl W, Rangsin R, et al. Prevalence of dyslipidemia associated with complications in diabetic patients: A nationwide study in Thailand. Lipids Health Dis 2019; 18:90.
- Noubiap JJN, Nansseu JRN, Bigna JJR, et al. Prevalence and incidence of dyslipidaemia among adults in Africa: A systematic review and meta-analysis protocol. BMJ Open 2015; 5:e007404.
- Ariyanti R, Besral B. Dyslipidemia associated with hypertension increases the risks for coronary heart disease: A case-control study in Harapan Kita Hospital, national cardiovascular center, Jakarta. J Lipids 2019; 2019:2517013.
- Moor VJA, Amougou SN, Ombotto S, et al. Dyslipidemia in patients with a cardiovascular risk and disease at the university teaching hospital of Yaounde, Cameroon. Int J Vasc Med 2017; 2017:6061306.
- Aldiab A, Shubair MM, Al-Zahrani JM, et al. Prevalence of hypertension and prehypertension and its associated cardioembolic risk factors: A population based cross-sectional study in Alkharj, Saudi Arabia. BMC Public Health 2018; 18:1327.
- Alzahrani GS, Aljehani SM, Al-Johani JJ. Risk Factors of dyslipidemia among Saudi population 2017. Egypt J Hosp Med 2018; 71:2262-2265.
- Almalki MA, AlJishi MN, Khayat MA, et al. Population awareness of coronary artery disease risk factors in Jeddah, Saudi Arabia: A cross-sectional study. Int J Gen Med 2019; 12:63–70.
- Dalal JJ, Padmanabhan TNC, Jain P, et al. Lipitension: Interplay between dyslipidemia and hypertension. Indian J Endocrinol Metab 2012; 16:240–245.
- Yu S, Yang H, Guo X, et al. Prevalence of dyslipidemia and associated factors among the hypertensive population from rural Northeast China. BMC Public Health 2015; 15:1152.
- Spannella F, Giulietti F, Pentima CD, et al. Prevalence and control of dyslipidemia in patients referred for high blood pressure: The disregarded “double-trouble” lipid profile in overweight/obese. Adv Ther 2019; 36:1426–1437.
- Jani Y, Kamberi A, Ferati F, et al. Influence of dyslipidemia in control of arterial hypertension among type-2 diabetics in the western region of the Republic of Macedonia. Am J Cardiovasc Dis 2014; 4:58–69.
- Leon BM, Maddox TM. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes 2015; 6:1246–1258.
- Qi Y, Han X, Zhao D, et al. Long-term cardiovascular risk associated with stage 1 hypertension defined by the 2017 ACC/AHA hypertension guideline. J Am Coll Cardiol 2018; 72:1201-1210.
- Talaei M, Hosseini N, Koh AK, et al. Association of "elevated blood pressure" and "stage 1 hypertension" with cardiovascular mortality among an Asian population. J Am Heart Assoc 2018; 7:e008911.
- Wu CY, Hu HY, Chou YJ, et al. High blood pressure and all-cause and cardiovascular disease mortalities in community-dwelling older adults. Medicine (Baltimore) 2015; 94:e2160.
Author Info
Abo Bakr Omar Hussain1, Mahmoud Hassan EL-Bidawy2,3, Mamdouh Ali Kotb4,5, Mohammed Ahammed Noureddin6*, Ali Hassan A Ali7,8 and Ramadan S Hussein9
1Department of Cardiology, College of Medicine, Prince Sattam Bin Abdul-Aziz University, Al-Kharj, 11942, Saudi Arabia2DBMS (Physiology division), College of Medicine, Prince Sattam Ibn Abdul-Aziz University, Al-Kharj, 11942, Saudi Arabia
3Department of Physiology, Faculty of Medicine, Cairo University, Cairo, Egypt
4Department of Neurology, College of Medicine, Prince Sattam Bin Abdul-Aziz University, Al-Kharj, 11942, Saudi Arabia
5Department of Neurology, Faculty of Medicine, AlMinia University, Egypt
6Department of Internal Medicine, College of Medicine, Prince Sattam Bin Abdul-Aziz University, Al-Kharj, 11942, Saudi Arabia
7Department of Anatomy, College of Medicine, Prince Sattam Bin Abdul-Aziz University, Al-Kharj, 11942, Saudi Arabia
8Department of Anatomy, College of Medicine, Al-Azhar University, Cairo, Egypt
9Department of Dermatology, College of Medicine, Prince Sattam Bin Abdul-Aziz University, Al-Kharj, 11942, Saudi Arabia
Citation: Mohammed A Noureddin, Alhumaidi M Alsubaie, Abdullah S Al-Dosarry, Fahad M Al-Ghamdi, Ziyad M Ali Alshehri, Tariq F Aldaej, Vitamin-D Deficiency and its Effect on Bone Profile: An Observational Study, J Res Med Dent Sci, 2020, 8 (6): 251-257.
Received: 05-Sep-2020 Accepted: 28-Sep-2020
