Research - (2022) Volume 10, Issue 1
Association of Chronic Rhinosinusitis with Risk of COVID-19 Infection
Tunjai Namiq Faiq1* and Ozdan Akram Ghareeb2
*Correspondence: Tunjai Namiq Faiq, Department of Otolaryngology, Kirkuk General Hospital, Iraq, Email:
Abstract
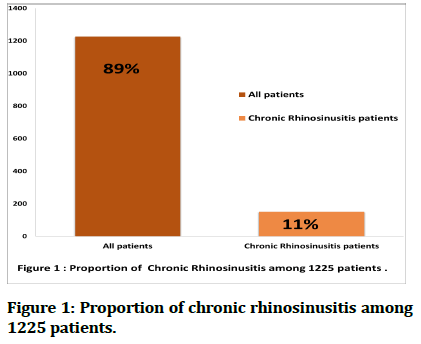
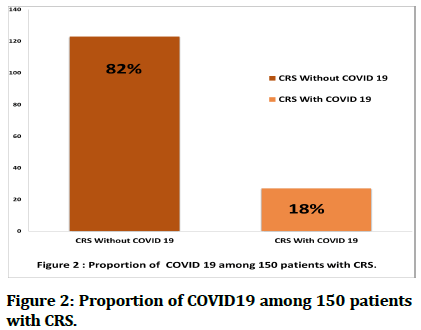
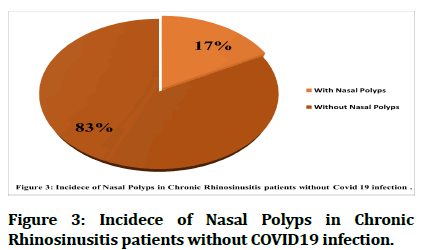
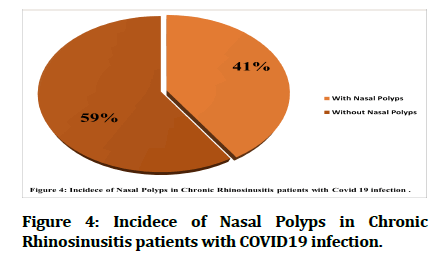
Chronic inflammatory diseases that affect the upper respiratory tract may be a risk factor for COVID19 infection. The current descriptive study is to investigate the existence of a relationship between chronic Rhinosinusitis disease (CRS) and infection with Covid 19. A descriptive study was conducted on 1125 participants who came to the specialized outpatient clinic of otolaryngology in Kirkuk) Iraq (, for the period between August and October of 2021. The results confirmed that the incidence of CRS among the participants was 11%, while the co-infection with COVID-19 was developed in 18 % of CRS patients. The incidence of hyposmia was 24 (18.0%) in CRS with COVID-19 patients versus 9 (6.0%) in non-Covid-19 patients. On the other hand, the proportion of nasal polyps was 41% among CRS patients infected with COVID-19. It was concluded that there is a risk relationship between chronic nasal inflammation and infection with Covid 19, so we recommend paying attention and conducting more accurate studies on this topic.
Keywords
Chronic rhinosinusitis, Otolaryngology, COVID-19
Introduction
Pathological disorders in the nasal cavity may seriously lead to lower airway diseases because it is the gateway to the respiratory system. Chronic Rhinosinusitis (CRS) is a prevalent nasal disorder, affecting up to 12% of the adult population [1,2]. CRS is a long-standing inflammatory condition of the nose and sinuses that is recognized by the existence of the following symptoms, a stuffy nose, nasal discharge with or without facial pain, and disorders of sense of smell [3,4]. Generally CRS is markedly categorized as CRS associated with nasal polyps and unassociated with nasal polyps, depending on the results of nasal endoscopy [5]. In simple terms, COVID-19 is a risky disease that affects the respiratory tract, causing severe pneumonia and potentially life-threatening complications such as multiple organ failure and death [6-9].The nasal cavity has substantial role in the infection of COVID-19 [10,11], and it has been shown that sino-nasal signs are often in the sever phase of an upper respiratory infection like COVID-19 are caused by generalized myxedema [12]. In general, there is a hypothesis that individuals who develop pre-existent upper airway infection are more susceptible to infection with COVID-19 [13,14], so this study was conducted to verify this hypothesis.
Methods and Patients
This study was conducted on 1225 individuals who attended the specialized outpatient clinic of the ear, nose and throat for the specialist consultant, Dr. Tunjai Namiq Faiq, in the center of Kirkuk governorate in northern Iraq. The study period extended from the first day of August to the end of October 2021. The diagnosis of chronic rhinosinusitis was confirmed by a specialist physician, and patient data were recorded after obtaining their consent to participate in the study. The diagnosis of chronic rhinosinusitis was confirmed by a specialist physician, as for the diagnosis of Covid 19 infection, it was through a polymerase chain reaction (PCR) procedure for a throat swab that was conducted in the public health laboratory in the governorate center. Data of patients were recorded after they agreed to participate in the study. Inclusion criteria for individuals were as follows: the youngest age 10 and the oldest 70 years old, males and females. As for the exclusion criteria for individuals, they were as follows: Those with serious diseases that made it difficult for them to answer. CRS patients were divided into two groups: a group of CRS patients with covid 19 infections and the other group of CRS patients without covid 19. A comparison was made between the two groups in terms of demographic factors such as gender, age, and dwelling places. In addition to the following symptoms: runny nose, rhinal obstruction, sneezing, olfactory disorders, and nasal polyps (NPs). A descriptive statistics method was used to display the results with the use of SPSS program version 25. Chi-square test was conducted, and the values were considered statistically significant at P < 0.05.
Results and Discussion
In this study, we found that 150 (11%) of the participants had chronic rhinosinusitis (Figure 1), and 27 (18 %) of the total patients, had a positive COVID-19 test, as illustrative in Figure 2.
The characteristics and symptoms of patients with CRS are shown in Table 1. The percentage of chronic rhinitis symptoms in patients with COVID-19 was as follows: 26 (17.3%) runny nose, 24 (18.0 %) hyposmia, 24 (16.0%) sneezing, and 14 (9.3%) rhinal obstruction.
While figures 3 and 4 represent the occurrence of nasal polyps in both CRS subgroups, as those who suffer from nasal polyps with Covid 19 co-infection amounted to about 11(41%) compared to 16 (59%) of them without polyps.
Figure 1: Proportion of chronic rhinosinusitis among 1225 patients.
Figure 2: Proportion of COVID19 among 150 patients with CRS.
Figure 3:Incidece of Nasal Polyps in Chronic Rhinosinusitis patients without COVID19 infection.
Figure 4:Incidece of Nasal Polyps in Chronic Rhinosinusitis patients with COVID19 infection.
| Characteristics | All CRS | CRS without Covid19 | CRS with Covid19 | P-value | |
|---|---|---|---|---|---|
| 150 (100 %) | 123 (82 %) | 27 (18 %) | |||
| Gender | Male | 71 | 56 | 15 | 0.345 |
| 47.30% | 37.30% | 10.00% | |||
| Female | 79 | 67 | 12 | ||
| 52.70% | 44.70% | 8.00% | |||
| Ages | 10-30 | 77 | 64 | 13 | 0.907 |
| 51.30% | 42.70% | 8.70% | |||
| 31-50 | 61 | 49 | 12 | ||
| 40.70% | 32.70% | 8.00% | |||
| 51-70 | 12 | 10 | 2 | ||
| 8.00% | 6.70% | 1.30% | |||
| Dwelling places | Urbanized | 128 | 105 | 23 | 0.981 |
| 85.30% | 70.00% | 15.30% | |||
| Ruralized | 22 | 18 | 4 | ||
| 14.70% | 12.00% | 2.70% | 0.089 | ||
| Runny nose | Yes | 129 | 103 | 26 | |
| 86.00% | 68.70% | 17.30% | |||
| No | 21 | 20 | 1 | ||
| 14.00% | 13.30% | 0.70% | 0 | ||
| Hyposmia | Yes | 41 | 23 | 18 | |
| 27.30% | 15.30% | 12.00% | |||
| No | 109 | 100 | 9 | ||
| 72.70% | 66.70% | 6.00% | 0.708 | ||
| Sneezing | Yes | 130 | 106 | 24 | |
| 86.70% | 70.70% | 16.00% | |||
| No | 20 | 17 | 3 | ||
| 13.30% | 11.30% | 2.00% | 0.006 | ||
| Rhinal Obstruction | Yes | 45 | 31 | 14 | |
| 30.00% | 20.70% | 9.30% | |||
| No | 105 | 92 | 13 | ||
| 70.00% | 61.30% | 8.70% | |||
Table 1: Distribution of characteristics and symptoms among the subgroups of CRS patients.
The corona virus that causes COVID-19, enters the body's cells via the angiotensin-converting enzyme 2 (ACE2) receptor [15,16].This enzyme is extremely expressed in nasal epithelium, particularly in non-acidic tissues, and is down regulated by IFN-γ, indicating that pro- existent type one inflammation may rise vulnerability to COVID-19 [17]. Previous studies confirmed a relationship between acute form of asthma and an augmentation risk of dying from COVID-19 [18-20]. Although a contrarian hypothesis asserts that altering ACE2 expression in recurrent inflammatory airway illnesses might modulate the risk of COVID-19 [21,22].To date, there are few studies evaluating COVID-19 infection in patients who have CRS, so we conducted this current study. Findings of this study suggested that infection with COVID-19 in chronic rhinosinusitis patients was 18%. This is consistent with Lee and colleagues' findings that 21% of CRS patients have serious COVID-19 comparison to the 13.3% non-CRS patients [23]. In addition, our findings are consistent with another previous study which confirmed that 67 (57.3%) suffer from decreased sense of smell (hyposmia) out of 117 patients infected with COVID-19 [24-26].
Conclusion
We concluded that the co-morbidity of COVID-19 in chronic rhinosinusitis patients was 18%, which is a high rate of concern. Therefore, chronic rhinosinusitis can be considered to be related with the promotion of COVID-19 infection. This requires more studies on this topic.
References
- Faiq TN, Ghareeb OA. Endoscopic management of orbital diseases of sinus origin: A case series. Ann Romanian Soc Cell Biol 2021; 25:8755-61.
- Takabayashi T, Schleimer RP. Formation of nasal polyps: The roles of innate type 2 inflammation and deposition of fibrin. J Allergy Clin Immunol 2020; 145:740-50.
- Poluan FH, Marlina L. Prevalence and risk factor of chronic rhinosinusitis and the impact on quality of life in students of the medical faculty christian university of Indonesia in 2018. J Drug Delivery Therapeut 2021; 11:154-62.
- Ranford D, Hopkins C. Safety review of current systemic treatments for severe chronic rhinosinusitis with nasal polyps and future directions. Expert Opinion Drug Safety 2021; 19:1-3.
- Laidlaw TM, Mullol J, Woessner KM, et al. Chronic rhinosinusitis with nasal polyps and asthma. J Allergy Clini Immunol 2021; 9:1133-41.
- Sultan AI, Ibrahim JM, Ghareeb OA. The prevalence of emergency surgical conditions among Covid-19 patients in Kirkuk province, Iraq. Pakistan J Med Health Sci 2021; 15:1087-1090.
- Dziedzic A, Wojtyczka R. The impact of coronavirus infectious disease 19 (COVIDâ?19) on oral health. Oral Dis 2021; 27:703-6.
- Al-Haidari KA, Faiq TN, Ghareeb OA. Preventive value of black seed in people at risk of infection with COVIDâ??19. Pakistan J Med Health Sci 2021; 15.
- Al-Haidari KA, Faiq T, Ghareeb O. Clinical trial of black seeds against covidâ??19 in Kirkuk city/Iraq. Indian J Forensic Med Toxicol 2021; 3393-9.
- Gengler I, Wang JC, Speth MM, et al. Sinonasal pathophysiology of SARSâ?CoVâ?2 and COVIDâ?19: A systematic review of the current evidence. Laryngoscope Investigative Otolaryngol 2020; 5:354-9.
- Pilicheva B, Boyuklieva R. Can the nasal cavity help tackle COVID-19?. Pharm 2021; 13:1612.
- Akhlaghi A, Darabi A, Mahmoodi M, et al. The frequency and clinical assessment of COVID-19 in patients with chronic rhinosinusitis. Ear Nose Throat J 2021.
- Furci F, Caminati M, Senna G, et al. The potential protective role of corticosteroid therapy in patients with asthma and COPD against COVID-19. Clin Molecular Allergy 2021; 19:1-5.
- Gallo O. Risk for COVID-19 infection in patients with tobacco smoke-associated cancers of the upper and lower airway. Eur Arch Otorhinolaryngol 2021; 278:2695-702.
- Ghareeb OA, Ramadhan SA. COVID 19-a novel zoonotic disease: Origin, prevention and control. Pakistan J Med Health Sci 2021; 221-3.
- Faiq TN, Ghareeb OA, Fadhel MF. Characteristics and outcomes of COVID 19 patients in Kirkuk City, Iraq. Annals Romanian Society Cell Biol 2021; 12432-8.
- Wang M, Bu X, Fang G, et al. Distinct expression of SARSâ?CoVâ?2 receptor ACE2 correlates with endotypes of chronic rhinosinusitis with nasal polyps. Allergy 2021; 76:789-803.
- Robinson LB, Fu X, Bassett IV, et al. COVID-19 severity in hospitalized patients with asthma: a matched cohort study. J Allergy Clin Immunol 2021; 9:497-500.
- Hamed IA, Shady NW, Ait-Allah AS. The role of diagnostic laparoscopy in the unexplained infertility cases. J Scientific Res Med Biol Sci 2021; 2:57-63.
- Bloom CI, Drake TM, Docherty AB, et al. Risk of adverse outcomes in patients with underlying respiratory conditions admitted to hospital with COVID-19: a national, multicentre prospective cohort study using the ISARIC WHO clinical characterisation protocol UK. Lancet Respir Med 2021.
- Terry PD, Heidel RE, Dhand R. Asthma in adult patients with COVID-19. prevalence and risk of severe disease. Am J Respir Critical Care Med 2021; 203:893-905.
- Yao Y, Wang H, Liu Z. Expression of ACE2 in airways: Implication for COVIDâ?19 risk and disease management in patients with chronic inflammatory respiratory diseases. Clin Exp All 2020; 50:1313-24.
- Xu X, Reitsma S, Wang DY, et al. Highlights in the advances of chronic rhinosinusitis. Allergy 2021.
- Alhusam S. Clinical conditions and risk factors of acinetobacter baumannii producing metallo beta-lactamases among hospitalized patients. J Scient Res Med Biol Sci 2021; 2:11-7.
- Lee SW, Kim SY, Moon SY, et al. Estimating COVID-19 infection and severity risks in patients with chronic rhinosinusitis: A Korean nationwide cohort study. J All Clin Immunol 2021.
- Faiq TN, Ghareeb OA, Ghaleb AA, et al. Incidence of hyposmia and hypoguesia in COVID-19 patients in Kirkuk. J Res Med Dent Sci 2021; 9:204-8.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Tunjai Namiq Faiq1* and Ozdan Akram Ghareeb2
1Department of Otolaryngology, Kirkuk General Hospital, Iraq2Department of Community Health, Northern Technical University, Iraq
Citation: Tunjai Namiq Faiq, Ozdan Akram Ghareeb,Association of Chronic Rhinosinusitis with Risk of COVID-19 Infection, J Res Med Dent Sci, 2022, 10(1): 382-385
Received: 22-Dec-2021, Manuscript No. Jrmds-21-47989; , Pre QC No. Jrmds-21-47989 (PQ); Editor assigned: 24-Dec-2021, Pre QC No. Jrmds-21-47989 (PQ); Reviewed: 07-Jan-2021, QC No. Jrmds-21-47989; Revised: 12-Jan-2022, Manuscript No. Jrmds-21-47989 (R); Published: 19-Jan-2022