Case Report - (2020) Volume 8, Issue 2
Asymptomatic Radiopacity of Mandible Causing Delayed Orthodontic Tooth Movement: A Case Report
Noor Sam Ahmad1*, Joann Yong Sook Mei1, Norliwati Ibrahim2, Azizah Ahmad Fauzi3 and Rohaya Megat Abdul Wahab1
*Correspondence: Noor Sam Ahmad, Department of Family Dental Health, Orthodontic Unit, Faculty of Dentistry, Universiti Kebangsaan Malaysia, Malaysia, Email:
Abstract
An incidental finding of a radiopaque lesion on the mandible on a routine orthopantomogram taken before orthodontic treatment had triggered an alarm to the orthodontist. The opacity of lesion showed that it was composed of a dense bone and the lesion presented in the pathway of planned orthodontic tooth movement. We report a case of an asymptomatic radiopaque, non-expansive and localized lesion which occurred as an incidental finding upon routine dental panoramic radiograph assessment prior to orthodontic treatment. The radiopaque lesion which was presented in the pathway of planned orthodontic tooth movement had triggered an alarm to the orthodontist. On the basis of dental panoramic radiograph, the lesion was classified as well defined completely opaque lesion (98mmx70mm), located at the right body of mandible between tooth 44 and tooth 45 and did not attach to these teeth in adjacent to it (with continuous periodontal space separating the roots from the lesion). Nevertheless, the distal part of the lesion demonstrated attachment to the cortical part of the mandibular bone. The lesion was found to cause delayed of orthodontic tooth movement but no root resorption.
Keywords
Radiopacities, Osteosclerosis, Localized lesion, Orthodontics tooth movement
Introduction
It is a difficult task to diagnose idiopathic osteosclerosis (IO) or also known as dense bone island or enostosis, accurately. Radiographically, it can be presented as a round, elliptical or irregular in shape radiopaque area. In term of size, it ranges from 2 or 3mm or 1 or 2cm in diameter or as big as almost the whole height of the body of mandible [1]. This lesion can be mistaken for exostosis, including torus mandibularis and palatinus, residual condensing osteitis, alveolar calcification after exodontia (whether complicated or not), bone architectural change in response to occlusal trauma on an inclined tooth, particularly on mandibular second molars, when the first molars are missing. Jaw lesions are commonly found in the mandible, usually at the molar region and they are associated with root apices [2]. Reported incidence of IO ranging from 2·4 to 7.5% [2-4]. These lesions are usually asymptomatic and often found incidentally on radiographs, in this case during an orthodontic examination. These lesion may even be mistaken for a radiographic projection over bone with a soft tissue calcification. The mere presence of teeth, their carious lesions, occlusal traumas and infectious processes, as well as the primary teeth shedding process, may also cause bone tissue architectural changes, adding to the above mentioned enostoses and dense bone islands. Histologically, the presentation of IO is characterized as dense trabecular bone with scant fibrofatty marrow. A dense bone is known to affect the orthodontic tooth movement within the region that is involved with the lesion. Orthodontic tooth movement in animal models has been shown to be accelerated when alveolar bone density is experimentally reduced [5]. However, to which extent the bone density affects root resorption is not fully understood. Some studies [6-7] have found a relationship between root resorption and movement of teeth through dense bone, while others have not [5,8]. This present case study discussed the presentation of increased alveolar bone density in association with IO in a patient who underwent orthodontic treatment.
Case Report
An 18-year-old female requested for orthodontic treatment at the Orthodontic Postgraduate Clinic, Faculty of Dentistry UKM, Kuala Lumpur. Her chief complaint was uneven teeth with a gap involving her front teeth. She was otherwise fit and healthy. Extraorally, she presented with a Class I skeletal pattern, increased Frankfurt- Mandibular Plane Angle (FMPA) and average Lower Anterior Facial Height (LAFH), symmetrical face, average nasolabial angle and incompetence lips. Intraorally, her oral hygiene was good with no carious teeth and all of her permanent teeth have erupted except the third molars. There was mild crowding in the lower arch (Figure 1). In occlusion, she was presented with Class I incisor relationship with increased overjet (OJ) of 5.0mm, anterior openbite of 2.5mm (measured between 12 and 42). Her upper centerline coincident with facial midline but the lower shifted to the right by 2.0mm. Canine relationship was Class II ¼ unit bilaterally and molar relationship was Class I bilaterally. 27 and 37 were in crossbites. Upon examination on the affected area over the right mandible, there was no bony enlargement, no numbness or tenderness on palpation and the soft tissues appeared normal.
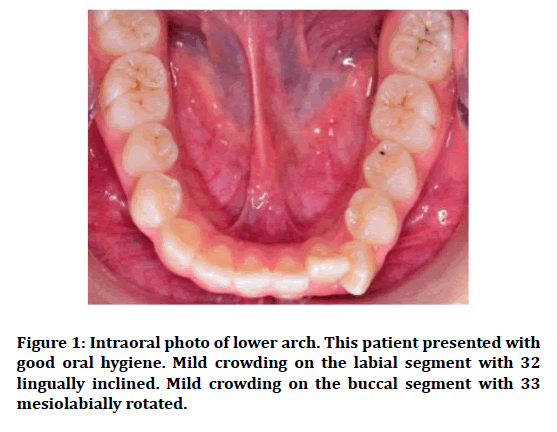
Figure 1: Intraoral photo of lower arch. This patient presented with good oral hygiene. Mild crowding on the labial segment with 32 lingually inclined. Mild crowding on the buccal segment with 33 mesiolabially rotated.
Radiographic findings
A 10 mm diameter mass with well demarcated border was observed at the right body of mandible. The lesion demonstrated as a homogenous radiopaque content and lie near the root apices of teeth 44 and 45. Nevertheless, both root apices did not demonstrate attachment to the lesion (Figure 2a). The incidental lesion detected in the dental panoramic radiograph prompted a re-evaluation of patient clinically. Cone-beam-computed-tomography (CBCT) was acquired for detail evaluation of the lesion and structures adjacent to it. Detail evaluation of the lesion with CBCT image, revealed fusion of the lesion with lamina dura lining the root apices of teeth 44 and 45 and its further attachment to the adjacent mandibular canal wall, as well as buccal and lingual mandibular body cortices (Figure 2b). A primary diagnosis of idiopathic osteosclerosis was made for the radiopaque lesion based on its clinical and classic radiological presentations.
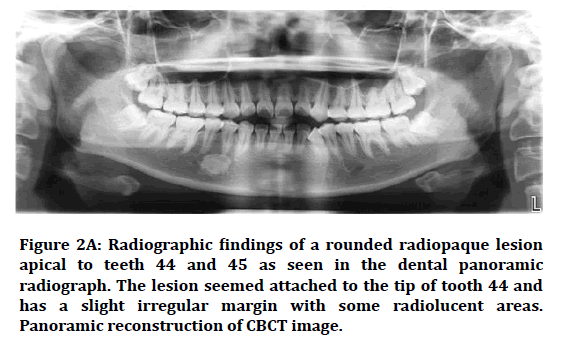
Figure 2A: Radiographic findings of a rounded radiopaque lesion apical to teeth 44 and 45 as seen in the dental panoramic radiograph. The lesion seemed attached to the tip of tooth 44 and has a slight irregular margin with some radiolucent areas. Panoramic reconstruction of CBCT image.
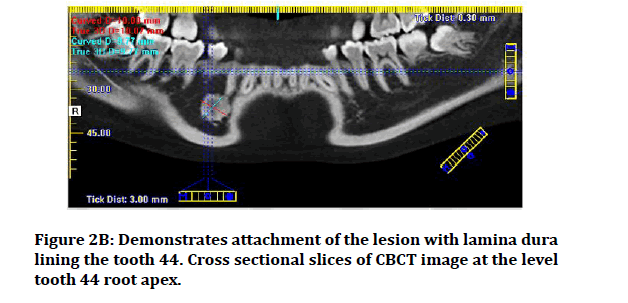
Figure 2B: Demonstrates attachment of the lesion with lamina dura lining the tooth 44. Cross sectional slices of CBCT image at the level tooth 44 root apex.
At the highest resolution of the CBCT image (0.3 mm panoramic slice thickness), the bone density at the alveolar process of the extracted teeth 44 and 34 regions were compared (Figure 2c). The mean density of alveolar process at the site of the extracted tooth 44 ranges from 808–879 HU. This is slightly higher in comparison to the mean density of alveolar process at the site of the extracted tooth 34 which ranges from 696–753 HU. A second cbct was requested as part of a 6-monthly radiographic review to assess any bony expansion of the lesion. At the same time, the tooth 43 and surrounding bone were evaluated for any abnormalities that could have delayed the orthodontic treatment.
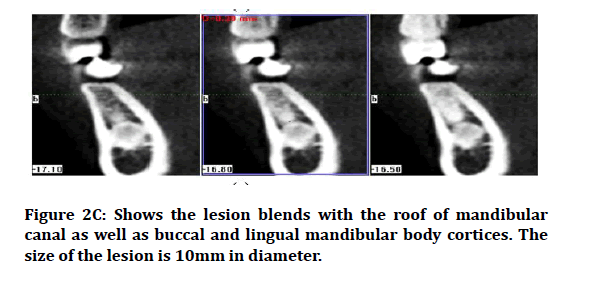
Figure 2C: Shows the lesion blends with the roof of mandibular canal as well as buccal and lingual mandibular body cortices. The size of the lesion is 10mm in diameter.
Orthodontic management
This patient was treated with orthodontic fixed appliance with extraction of all first permanent premolars. She was bonded with conventional orthodontic brackets and with 0.014NiTi as initial archwire for upper and lower arch. Both the lower canines were ligated with ligation wire and retraction was done 4 months after the bracket’s placement with 0.018 stainless steel archwire using 3 links power chain, attached to the hook of the lower 1st molars. No movement of lower right canine was seen during the first review after 1 month. On the contralateral side, the tooth 33 had moved distally approximately 1.5mm. Reviewed on the following month showed that there was still no movement of tooth 43 while tooth 33 had proximated with tooth 35. Following 3 months of orthodontic management, no movement of tooth 43 was observed despite movement of the contralateral lower canine. There was no occlusal interference prior or during the canine retraction. The operator decided to use NiTi closed coil spring to retract tooth 43. A month later, tooth 43 moved. The operator kept on retracting the tooth 43 until it finally proximated with the tooth 45 as observed on the 6-month interval (Table 1). Evaluation of the second CBCT image showed no evidence of socket sclerosis, no changes in the appearance of the radiopaque lesion which can address the delayed tooth movement and no root resorption.
| Tooth | Duration | |||||
|---|---|---|---|---|---|---|
| Traction using power chain | Traction using NiTi coil spring | |||||
| 1 month | 2 Months | 3 Months | 4 Months | 5 Months | 6 Months | |
| 33 | 1.5 mm | Proximated | - | - | - | - |
| 43 | 0 mm | 0 mm | 0 mm | 2.5mm | 2.0 mm | Proximated |
Table 1: Duration taken for tooth 33 and 43 to proximate with adjacent tooth.
Discussion
Among the differential diagnoses for radiopaque lesions encountered in orthodontics patients, idiopathic osteosclerosis (IO) fits into the current case presentation. of a single lesion of any age, non-expansive bone and no resorption nor deviation of teeth. The sclerotic areas persisted indefinitely, and some may even disappear with constant and normal bone remodelling [9]. Similarly, osteosclerosis related to Gardner’s syndrome may also affecting young patients but unlike the current case, the lesion may present as multiple lesions and usually occurs at sites of previous extractions.
Benign fibro osseous lesions such as fibrous dysplasia, ossifying fibroma, and osseous dysplasia are difficult to distinguish by radiological findings. They may exhibit radiolucency or mixed radiolucent-radiopacity, and even radiopacity depending on the spectrum of maturity. Like this case, ossifying fibroma is commonly seen at premolar and molar region of mandible. It often exhibits round or oval shaped single lesion but with a welldefined margin with corticated lines. In addition, it often shows cystic or mixed-density appearances which is dissimilar to the current case [10-11]. Meanwhile, late stage osseous dysplasia may present as uniformly radiopaque mass at root apex of a vital too [10]. Unless when the radiopacity surrounded by a radiolucent rim, the lesion is difficult to be differentiated with IO. In the current case, the irregular border of the lesion which blends with buccal and lingual mandibular body cortices identified with CBCT imaging provided a more definitive appearance of idiopathic osteosclerosis.
The compound type of odontomes radiographically exhibits a well-organized multiple malformed tooth or denticles of varying size and shape surrounded by a narrow radiolucent band while the complex type presents with a large, irregular calcified mass surrounded by a narrow and even radiolucent periphery [12]. However, the current lesion is a single radiopacity with no appearance of denticles resembling the compound odontomes, nor as irregular as the complex type.
Juvenile mandibular chronic osteomyelitis and pseudocysts may also present with radiopacity, nonetheless, these lesions may have discharges like pus. The border of lesions are not well-defined especially the osteomyelitis and the patients may complained of pain.
Tooth movement at sclerotic region
Idiopathic osteosclerosis has normal bone structure except that it has higher trabecular density thus longer bone remodelling required. Researchers claimed that teeth can be moved in this region and procedures like Osseo integrating implants and mini implants can be placed without further consequences, provided that the region has no evidence of infection [9]. In this study, tooth movement was evident but at a much slower rate than usual. As tooth 43 did not move during the first 3 month as compared to the contralateral side, the operator decided to use NiTi closed coil spring in order to move the tooth distally. It took about 3 months for tooth 43 to initially start moving and another 3 months to completely approximate with tooth 45. While on the contralateral part, it only took 1 month to start moving and 2 months to completely approximate with the 35.
Propose of management
In cases needing tooth movement through denser areas such as idiopathic osteosclerosis bone type, the ideal would be to use continuous and lighter forces than those normally employed, compensating part of the force that would be dissipated by the adjacent bone deflection [9]. By analogy, reducing the force corresponds to a discount, or compensation, because the bone deflection does not happen due to the higher density on site. Under these circumstances, surprisingly a normal and even faster movement will occur, even in a denser area. Furthermore, the use of conventional forces in these cases can induce hyalinization areas and death of cementoblasts followed by root resorption besides preventing an efficient tooth movement. In this case, the operator decided to change from power chain to NiTi closed coil spring which provided a continuous retraction force on the 43 since the was no evidence of movement of the tooth [13]. It took approximately 6 months to get tooth-to tooth contact of the affected side. In view of the lesion, an excision of this mass will only leave an empty intraosseous space that may weaken the bone structure. In this case, a decision was made to leave the radiopaque lesion in situ because there was no bony expansion and pain as suggested by other researchers [10,14].
Conclusion
Delayed orthodontic tooth movement may occur due to the high trabecular bone density area. A continuous force using Niti closed coil spring may help in moving tooth in this high bone density area. In the presence of radiopaque lesion in the tooth movement pathway, orthodontic tooth movement should be planned with caution to avoid any unwanted effect such as root resorption.
References
- MacDonald-Jankowski DS. Idiopathic osteosclerosis in the jaws of Britons and of the Hong Kong Chinese: Radiology and systematic review. Dentomaxillofac Radiol 1999; 28: 357-363.
- Sisman Y, Ertas ET, Ertas H, et al. The frequency and distribution of idiopathic osteosclerosis of the jaw. Eur J Dent 2011; 5:409-414.
- Farhadi F, Ruhani MR, Zarandi A. Frequency and pattern of idiopathic osteosclerosis and condensing osteitis lesions in panoramic radiography of Iranian patients. Dent Res J 2016; 13:322–326.
- Miloglu O, Yalcin E, Buyukkurt MC, et al. The frequency and characteristics of idiopathic osteosclerosis and condensing osteitis lesions in a Turkish patient population. Med Oral Patol Oral Cir Bucal 2009; 14:640-645.
- Kapila S, King GK. Biological mechanisms in orthodontic tooth movement in esthetics and biomechanics in orthodontics. WB Saunders. 2015; 90-107.
- Kaley J, Phillips C. Factors related to root resorption in edgewise practice. Angle Orthodont 1991; 61:125-132.
- Horiuchi A, Hotokezaka H, Kobayashi K. Correlation between cortical plate proximity and apical root resorption. Ame J Orthodont Dent Orthop1998; 114:311–318.
- Scheibel PC, Ramos AL, Iwaki LCV, et al. Analysis of correlation between initial alveolar bone density and apical root resorption after 12 months of orthodontic treatment without extraction. Dental Press J Orthod 2014; 19:97-102.
- Consolaro A, Consolaro RB. Advancements in the knowledge of induced tooth movement: Idiopathic osteosclerosis, cortical bone and orthodontic movement. Dental Press J Orthod 2012; 17:12-16.
- Koenig LJ, Tamimi D, Petrikowski GC, et al. Diagnostic imaging: Oral and maxillofacial 2nd Edn Canada.
- Akashi M, Matsuo K, Shigeoka M, et al. A case series of fibro-osseous lesions of the jaws. Kobe J Med Sci 2017; 63:73-79.
- Satish V, Prabhadevi MC, Sharma R. Odontome: A brief overview. Int J Clin Pediat Dent 2011; 4:177-185.
- Cox C, Nguyen T, Koroluk L, et al. In Vivo force decay of niti closed coil springs. Am J Orthod Dentofacial Orthop 2014; 145: 505–513.
- Silva BSF, Bueno MR, Yamamoto-Silva FP. et al. Differential diagnosis and clinical management of periapical radiopaque/hyperdense jaw lesions. Braz Oral Res 2017; 31:e52.
Author Info
Noor Sam Ahmad1*, Joann Yong Sook Mei1, Norliwati Ibrahim2, Azizah Ahmad Fauzi3 and Rohaya Megat Abdul Wahab1
1Department of Family Dental Health, Orthodontic Unit, Faculty of Dentistry, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia2Department of Orofacial Diagnostics and Biosciences, Oral Pathology and Oral Medicine Unit, Faculty of Dentistry, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
3Department of Orofacial Diagnostics and Biosciences, Clinical Oral Biology Unit, Faculty of Dentistry, Universiti Kebangsaan Malaysia, Kuala Lumpur, Malaysia
Citation: Noor Sam Ahmad, Joann Yong Sook Mei, Norliwati Ibrahim, Azizah Ahmad Fauzi, Rohaya Megat Abdul Wahab, Asymptomatic Radiopacity of Mandible Causing Delayed Orthodontic Tooth Movement: A Case Report, J Res Med Dent Sci, 2020, 8(2): 72-75
Received: 17-Mar-2020 Accepted: 10-Apr-2020
