Research - (2021) Volume 9, Issue 1
Awareness on Management of Adenocarcinoma of the Palate
Vishnu Prasanna SG and Dhanraj Ganapathy*
*Correspondence: Dhanraj Ganapathy, Department of Prosthodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, India, Email:
Abstract
Minor salivary gland neoplasms constitute approximately 25% of all the salivary gland tumours. The incidence of these tumors turning into malignancy is slightly greater than half but varies by series. Adenocarcinoma is an uncommon tumour that usually affects the minor salivary glands, particularly in the palate. Adenocarcinomas are distinctive neoplasms which may be sub classified according to their tissue growth patterns or histo-cytomorphology. Polymorphous low-grade adenocarcinoma (PLGA) is a minor salivary gland carcinoma usually arises intraorally, which occurs primarily in the palate. A survey was conducted in January 2020 among dental students. It was an online questionnaire based study, conducted to assess the awareness on the management of adenocarcinoma. 150 dental students (Third years, Final years, Interns) participated in this study. The data collected was entered in an Excel sheet and subjected to statistical analysis using SPSS version 20. Chi square test was done. 25.33% of third years, 29.33% of final years and 32% of interns were aware of the term adenocarcinoma. 32% of third years, 30.67% of final years, 33.33% of interns have come across patients with adenocarcinoma. 16.67% of third years, 25.33% of final years and 30% of interns knew how adenocarcinoma was caused. 14% of third years, 27.33% of final years, 26.67% of interns were aware of diagnostic aids. 16% of third years, 8.67% of final years, 30% of interns have seen a patient with similar lesions. Chi square test shows p<0.000, significant. It was seen that Interns had a good awareness of management of adenocarcinoma when compared to the final and third years.
Keywords
Awareness, Adenocarcinoma, Diagnosis, Malignant tumours
Introduction
Minor salivary gland neoplasms constitute approximately 25% of all the salivary gland tumors [1]. The incidence of these tumours turning into malignancy is slightly greater than half but varies by series. Polymorphous lowgrade adenocarcinomas are low‐grade malignant salivary‐gland neoplasms with a broad variety of architectural patterns [2]. Adenocarcinoma is an uncommon tumour that usually affects the minor salivary glands, particularly in the palate [3]. Adenocarcinoma is a relatively common malignancy of the oral cavity, representing 7% to 11% of all intraoral minor salivary gland tumors, and 19% to 26% of those that are malignant [4]. Adenocarcinomas are distinctive neoplasms which may be sub classified according to their tissue growth patterns or histo-cytomorphology. A clinico-pathologic evaluation of adenocarcinomas of salivary tissues has also been delayed by their inclusion under the generic heading of ‘adenocarcinoma’, wherein all forms of glandular malignancy are included [5]. Polymorphous low-grade adenocarcinoma (PLGA) is a minor salivary gland carcinoma usually arises intraorally, which occurs primarily in the palate. This tumour is characterized by histologic blandness, cytologic uniformity, and a variable, infiltrating growth pattern [6]. Recently, polymorphous low-grade adenocarcinoma is regarded as the second most common salivary gland tumour after mucoepidermoid carcinoma. polymorphous low-grade adenocarcinoma has been a locally invasive carcinoma without distant metastases. Polymorphous low-grade adenocarcinoma is usually treated with local excision [7]. Low-grade papillary adenocarcinoma of minor salivary glands is rare and tends to occur in the palate [8]. Low‐grade papillary adenocarcinoma of the palate is a rare but distinctive neoplasm. Low grade adenocarcinoma is often misdiagnosed and inadequately treated initially and progresses slowly [9] Mucinous adenocarcinoma (MAC) arising in the oral cavity especially in palate is extremely rare.
Previously our department has published extensive research on various aspects of prosthetic dentistry [10-20], this vast research experience has inspired us to research about the awareness on management of squamous cell carcinoma. The aim of this study is to create awareness on diagnosis of adenocarcinoma of palate among dental students.
Materials and Methods
Study design
Awareness based survey.
Data collection
A survey was conducted in January 2020 among dental students (Third years, Final years, Interns). It was an online questionnaire based study, conducted to assess the awareness on the management of adenocarcinoma. 150 dental students (Third years, Final years, Interns) participated in this study. The data collection was done via google forms.
Survey instrument
A pretested, self-administered, closed ended questionnaire comprising the following sections formed the survey instrument. A structured questionnaire containing 10 questions which was adopted from a validated questionnaire developed by the World Health Organisation. The questionnaire was equally distributed among Third years, Final years, Interns. The goal of developing this questionnaire was to know about the awareness the dental students have on the management of adenocarcinoma. The questions had to be answered with a Yes or No response.
Ethical approval
Ethical approval was obtained from the institutional ethical committee.
Data analysis
The data collected was entered in an Excel sheet and subjected to statistical analysis using SPSS version 20. Chi square test was done. The independent variables are age and gender while dependent variables are knowledge, attitude and practice of management of adenocarcinoma. The level of significance was set at p<0.05.
Results
From the results of the study, 25.33% of third years, 29.33% of final years and 32% of interns were aware of the term adenocarcinoma. Chi square test shows p value=0.00, significant (Figure 1). 32% of third years, 30.67% of final years, 33.33% of interns have come across patients with adenocarcinoma. Chi square test shows p value=0.00, significant (Figure 2). 16.67% of third years, 25.33% of final years and 30% of interns knew how adenocarcinoma was caused. Chi square test shows p value=0.00, significant (Figure 3). 14% of third years, 27.33% of final years, 26.67% of interns were aware of diagnostic aids. Chi square test shows p value=0.00, significant (Figure 4). 16% of third years, 8.67% of final years, 30% of interns have seen a patient with similar lesions. Chi square test shows p value=0.00, significant (Figure 5). 32% of third years, 10% of final years and 13.33% of interns have never misdiagnosed a case of adenocarcinoma. Chi square test shows p value = 0.00, significant (Figure 6). 28.67% of third years, 26% of final years and 24% of interns were aware of clinical presentations of adenocarcinoma. Chi square test shows p value=0.00, significant (Figure 7). 26% of third years, 21.33% of final years and 24.67% of interns were aware of histopathological features. Chi square test shows p value=0.00, significant (Figure 8). 10.67% of third years, 27.33% of final years and 20% of interns knew the treatment options for adenocarcinoma. Chi square test shows p value=0.00, significant (Figure 9). 22.67% of third years, 11.33% of final years and 32% of interns recommended incisional biopsy for confirmatory diagnosis. Chi square test shows p value=0.00, significant (Figure 10).
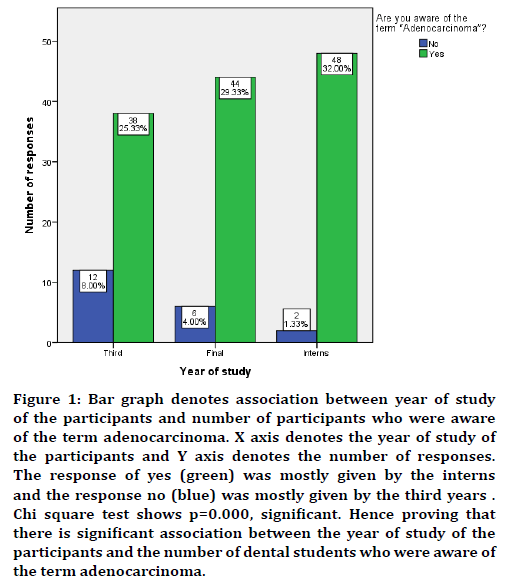
Figure 1. Bar graph denotes association between year of study of the participants and number of participants who were aware of the term adenocarcinoma. X axis denotes the year of study of the participants and Y axis denotes the number of responses. The response of yes (green) was mostly given by the interns and the response no (blue) was mostly given by the third years . Chi square test shows p=0.000, significant. Hence proving that there is significant association between the year of study of the participants and the number of dental students who were aware of the term adenocarcinoma.
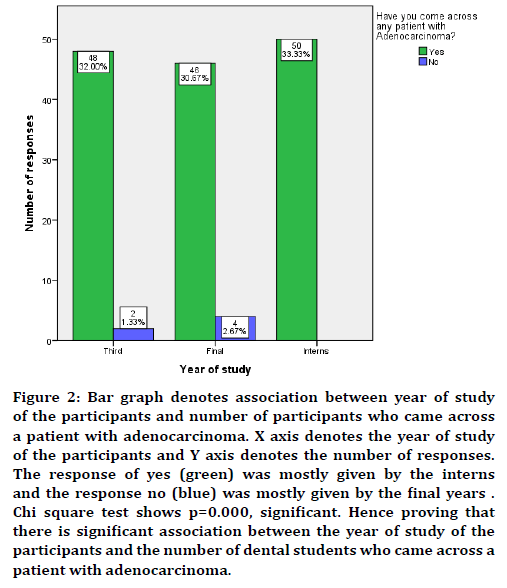
Figure 2. Bar graph denotes association between year of study of the participants and number of participants who came across a patient with adenocarcinoma. X axis denotes the year of study of the participants and Y axis denotes the number of responses. The response of yes (green) was mostly given by the interns and the response no (blue) was mostly given by the final years . Chi square test shows p=0.000, significant. Hence proving that there is significant association between the year of study of the participants and the number of dental students who came across a patient with adenocarcinoma.
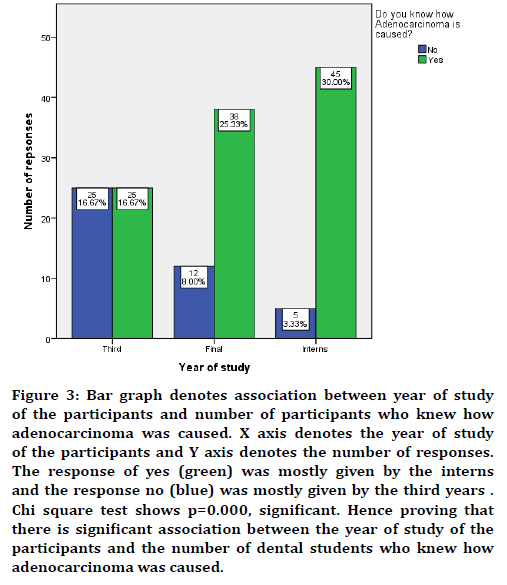
Figure 3. Bar graph denotes association between year of study of the participants and number of participants who knew how adenocarcinoma was caused. X axis denotes the year of study of the participants and Y axis denotes the number of responses. The response of yes (green) was mostly given by the interns and the response no (blue) was mostly given by the third years . Chi square test shows p=0.000, significant. Hence proving that there is significant association between the year of study of the participants and the number of dental students who knew how adenocarcinoma was caused.
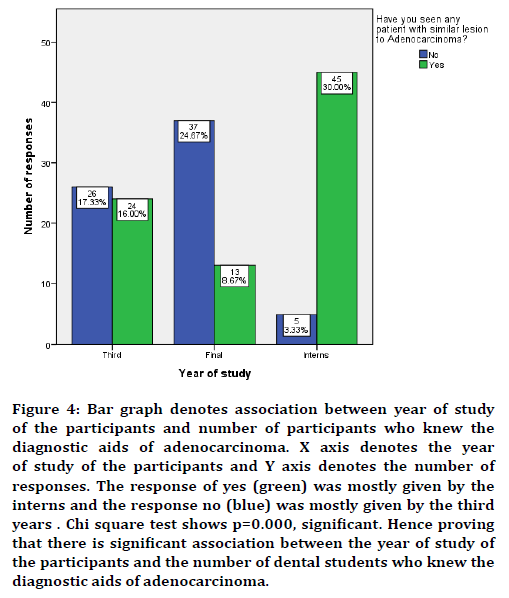
Figure 4. Bar graph denotes association between year of study of the participants and number of participants who knew the diagnostic aids of adenocarcinoma. X axis denotes the year of study of the participants and Y axis denotes the number of responses. The response of yes (green) was mostly given by the interns and the response no (blue) was mostly given by the third years . Chi square test shows p=0.000, significant. Hence proving that there is significant association between the year of study of the participants and the number of dental students who knew the diagnostic aids of adenocarcinoma.
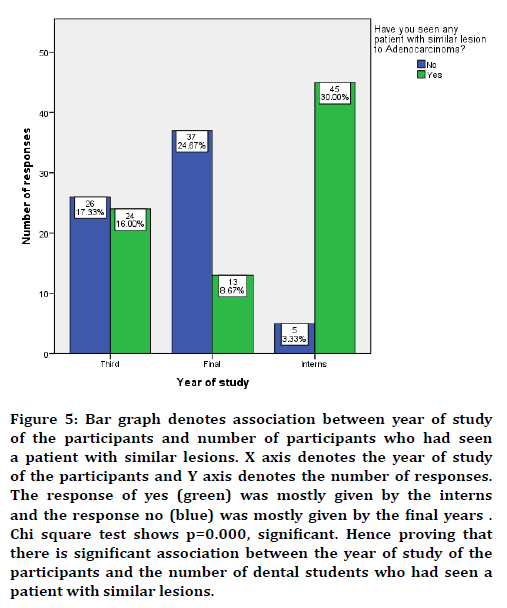
Figure 5. Bar graph denotes association between year of study of the participants and number of participants who had seen a patient with similar lesions. X axis denotes the year of study of the participants and Y axis denotes the number of responses. The response of yes (green) was mostly given by the interns and the response no (blue) was mostly given by the final years . Chi square test shows p=0.000, significant. Hence proving that there is significant association between the year of study of the participants and the number of dental students who had seen a patient with similar lesions.
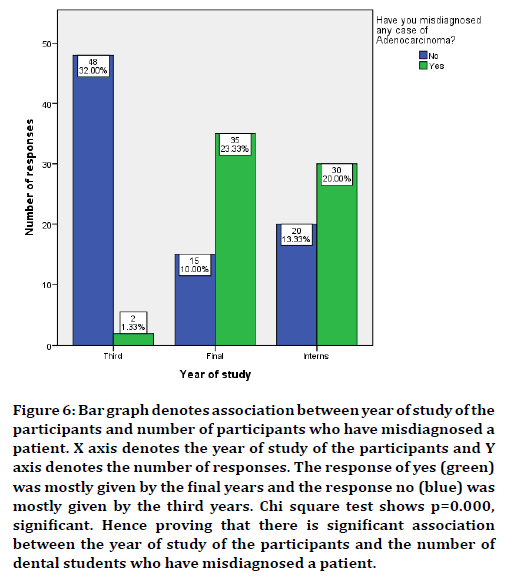
Figure 6. Bar graph denotes association between year of study of the participants and number of participants who have misdiagnosed a patient. X axis denotes the year of study of the participants and Y axis denotes the number of responses. The response of yes (green) was mostly given by the final years and the response no (blue) was mostly given by the third years. Chi square test shows p=0.000, significant. Hence proving that there is significant association between the year of study of the participants and the number of dental students who have misdiagnosed a patient.
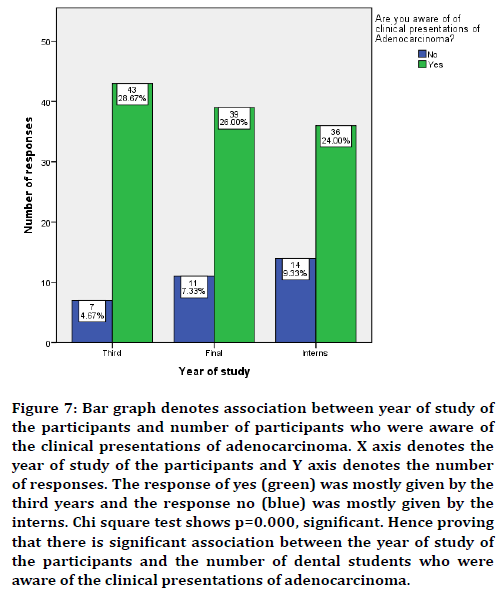
Figure 7. Bar graph denotes association between year of study of the participants and number of participants who were aware of the clinical presentations of adenocarcinoma. X axis denotes the year of study of the participants and Y axis denotes the number of responses. The response of yes (green) was mostly given by the third years and the response no (blue) was mostly given by the interns. Chi square test shows p=0.000, significant. Hence proving that there is significant association between the year of study of the participants and the number of dental students who were aware of the clinical presentations of adenocarcinoma.
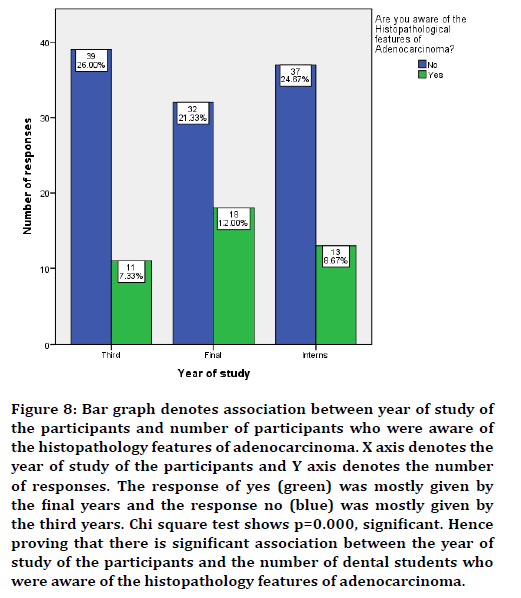
Figure 8. Bar graph denotes association between year of study of the participants and number of participants who were aware of the histopathology features of adenocarcinoma. X axis denotes the year of study of the participants and Y axis denotes the number of responses. The response of yes (green) was mostly given by the final years and the response no (blue) was mostly given by the third years. Chi square test shows p=0.000, significant. Hence proving that there is significant association between the year of study of the participants and the number of dental students who were aware of the histopathology features of adenocarcinoma.
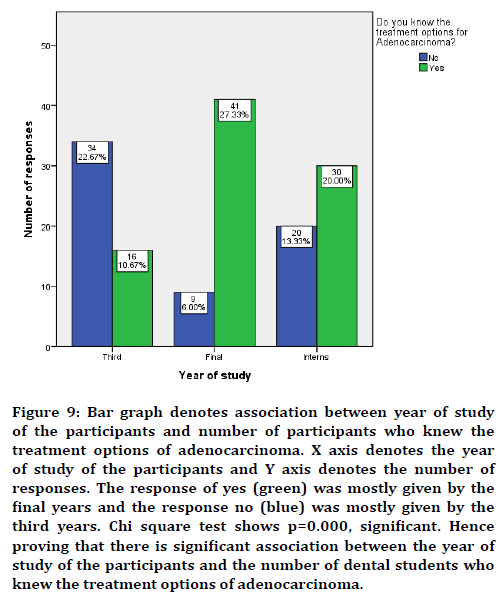
Figure 9. Bar graph denotes association between year of study of the participants and number of participants who knew the treatment options of adenocarcinoma. X axis denotes the year of study of the participants and Y axis denotes the number of responses. The response of yes (green) was mostly given by the final years and the response no (blue) was mostly given by the third years. Chi square test shows p=0.000, significant. Hence proving that there is significant association between the year of study of the participants and the number of dental students who knew the treatment options of adenocarcinoma.
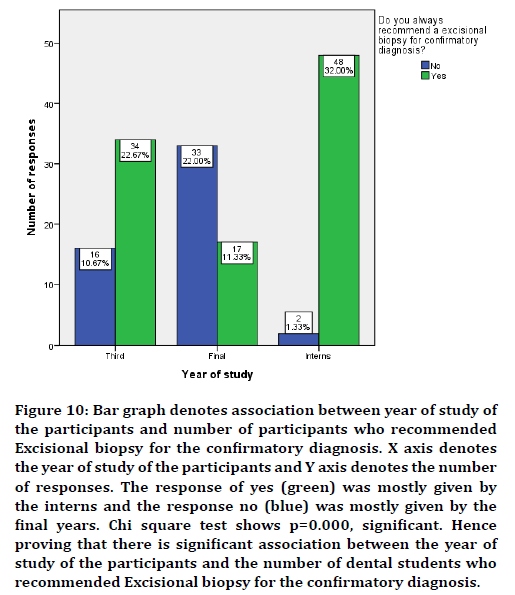
Figure 10. Bar graph denotes association between year of study of the participants and number of participants who recommended Excisional biopsy for the confirmatory diagnosis. X axis denotes the year of study of the participants and Y axis denotes the number of responses. The response of yes (green) was mostly given by the interns and the response no (blue) was mostly given by the final years. Chi square test shows p=0.000, significant. Hence proving that there is significant association between the year of study of the participants and the number of dental students who recommended Excisional biopsy for the confirmatory diagnosis.
Discussion
Our results depicted that the majority of the participants were aware of the term adenocarcinoma. Most of them had come across patients with adenocarcinoma and had knowledge on the etiology of adenocarcinoma. Most of them knew the diagnostic aids of adenocarcinoma. The majority of the participants had seen cases with similar lesions. Most of the participants did not misdiagnose a case with adenocarcinoma because they were aware of the clinical presentation however they were not aware of the histopathological features. Most of the participants knew the treatment options available for adenocarcinoma and recommended an excisional biopsy for confirmatory diagnosis.
In our study, it was reported that most of the participants were not aware of the histopathological features of adenocarcinoma. Batsakis et al reported that a histologic feature, present in varying degrees, in all of the tumors, was an elongation or spindling of the neoplastic cells [5]. Adenocarcinoma generally has a slow rate of growth, absence of symptoms, less aggressiveness, minimal metastatic potential and good prognosis [21]. It basically can occur mostly on the palate, followed by either the upper lip or buccal mucosa and rarely could involve floor of mouth, lower lip, alveolar ridge and tongue [22].
Our study shows that the majority of the participants had knowledge on the etiology of adenocarcinoma. Batsakis et al. reported that the majority of the adenocarcinomas of salivary tissues are presumed to arise from the reserve cells of the metabolically active or conduit parts of the salivary duct unit, i.e., intra-, inter-, and excretory ducts.
In our study, it was reported that the majority of the participants knew the treatment options for adenocarcinoma and recommended excisional biopsy for confirmatory diagnosis. Sathyanarayanan et al. reported that wide local excision should be the ideal treatment of choice. If positive or close surgical margins is there, post-operative radiotherapy is recommended but it has not shown to alter outcome in patients without neck node metastasis [23]. Batsakis et al. reported that surgical excision was the primary treatment in all patients. The extent of the excision ranged from 'excisional biopsy' to a block resection, including hemimandibulectomy, radical neck dissection and post-operative irradiation. Wide local excision should be the treatment of choice. If positive or close surgical margins are present, post-operative radiotherapy is done but it has not shown to alter outcome in patients without neck node metastasis. Radiotherapy is indicated if there is cervical lymph node metastasis. The recurrence rate for adenocarcinoma is minimal following wide excision and if present radical excision is done [24].
There are no comparative studies since not much attention is given towards training the students at an undergraduate level to encounter and manage patients with adenocarcinoma. Thus the curriculum should emphasize the need to know about the management of adenocarcinoma. The limitation was the study is that the study was conducted only in one city (Chennai) and may not be generalized to other regions.
Conclusion
Within the limitation of the study it was seen that Interns had a good awareness on management of adenocarcinoma when compared to the final and third years. This is because of the clinical expertise that the interns have acquired through clinical experience and clinical practice.
Acknowledgment
The authors acknowledge all the parents who provided consent and spent their time on completing this survey.
Conflict of Interest
The authors of the study declare that there were no conflicts of interest.
References
- Ellis GL, Auclair PL. Armed forces institute of pathology. Tumors of the salivary glands. atlas of tumor pathology, 3rd Edn, Washington DC. 1996; 17: 257–267.
- Slootweg PJ. Low-grade adenocarcinoma of the oral cavity: Polymorphous or papillary? J Oral Pathol Med 1993; 22:327–330.
- Kumar M, Stivaros N, Barrett AW, et al. Polymorphous low-grade adenocarcinoma: A rare and aggressive entity in adolescence. Br J Oral Maxillofac Surg 2004; 42:195-199.
- Pittman CB, Zitsch RP. Polymorphous low-grade adenocarcinoma of the tonsil: report of a case and review of the literature. Am J Otolaryngol 2002; 23:297–299.
- Batsakis JG, Pinkston GR, Luna MA, et al. Adenocarcinomas of the oral cavity: A clinicopathologic study of terminal duct carcinomas. J Laryngol Otol 1983; 97:825-835.
- Gnepp DR, Chen JC, Warren C. Polymorphous low-grade adenocarcinoma of minor salivary gland: An immunohistochemical and clinicopathologic study. Am J Surg Pathol 1988; 12:461-468.
- Crean SJ, Bryant C, Bennett J, et al. Four cases of polymorphous low-grade adenocarcinoma. Int J Oral Maxillofac Surg 1996; 25:40-44.
- Mostofi R, Wood RS, Christison W, et al. Low-grade papillary adenocarcinoma of minor salivary glands: Case report and literature review. Oral Surg Oral Med Oral Pathol 1992; 73:591-595.
- Allen Jr MS, Fitz‐Hugh GS, Marsh WL. Low‐grade papillary adenocarcinoma of the palate. Cancer 1974; 33:153-158.
- Begum R, Ariga P, Jain AR. Evaluation of corrosive behavior of four nickel–chromium alloys in artificial saliva by cyclic polarization test: An in vitro Study. World J Dent 2017; 8:477–482.
- Ganapathy DM, Kannan A, Venugopalan S. Effect of coated surfaces influencing screw loosening in implants: A systematic review and meta-analysis. World J Dent 2017; 8:496–502.
- Jain AR. Clinical and functional outcomes of implant prostheses in fibula free flaps. World J Dent 2017; 8:171–176.
- Jain AR. Prevalence of partial edentulousness and treatment needs in rural population of South India. World J Dent 2017; 8:213–217.
- Ranganathan H, Ganapathy DM, Jain AR. Cervical and incisal marginal discrepancy in ceramic laminate veneering materials: A SEM analysis. Contemporary Clin Dent 2017; 8:272–278.
- Jain AR, Nallaswamy D, Ariga P, et al. Determination of correlation of width of maxillary anterior teeth using extraoral and intraoral factors in Indian population: A systematic review. World J Dent 2018; 9:68-75.
- Gupta P, Ariga P, Deogade SC. Effect of monopoly-coating agent on the surface roughness of a tissue conditioner subjected to cleansing and disinfection: A contact profilometric study. Contemporary Clin Dent 2018; 9:S122–S126.
- Anbu RT, Suresh V, Gounder R, et al. Comparison of the efficacy of three different bone regeneration materials: An animal study. Eur J Dent 2019; 13:22.
- Ashok V, Ganapathy D. A geometrical method to classify face forms. J Oral Biol Craniofac Res 2019; 9:232–235.
- Duraisamy R, Krishnan CS, Ramasubramanian H, et al. Compatibility of nonoriginal abutments with implants: evaluation of microgap at the implant–Abutment interface, with original and nonoriginal abutments. Implant Dent 2019; 28:289-295.
- Varghese SS, Ramesh A, Veeraiyan DN. Blended module-based teaching in biostatistics and research methodology: A retrospective study with postgraduate dental students. J Dent Educ 2019; 83:445–450.
- Yih WY, Kratochvil FJ, Stewart JC. Intraoral minor salivary gland neoplasms: review of 213 cases. J Oral Maxillofac Surg 2005; 63:805-10.
- Buchner A, Merrell PW, Carpenter WM. Relative frequency of intra‐oral minor salivary gland tumors: A study of 380 cases from northern California and comparison to reports from other parts of the world. J Oral Pathol Med 2007; 36:207-214.
- Sathyanarayanan R, Suresh V, Thomas BA. Polymorphous low-grade adenocarcinoma of the palate: a rare case report. Iranian J Cancer Prevention 2016; 9.
- El-Naaj IA, Leiser Y, Wolff A, et al. Polymorphous low grade adenocarcinoma: case series and review of surgical management. J Oral Maxillofac Surg 2011; 69:1967-1972.
Author Info
Vishnu Prasanna SG and Dhanraj Ganapathy*
Department of Prosthodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, IndiaCitation: Vishnu Prasanna SG, Dhanraj Ganapathy, Awareness on Management of Adenocarcinoma of the Palate, J Res Med Dent Sci, 2021, 9 (1): 371-376.
Received: 23-Sep-2020 Accepted: 13-Jan-2021
