Research - (2022) Volume 10, Issue 2
Breast Cancer in Southern Saudi Arabia: Prevalence, Risk Factors and Attitude
*Correspondence: Maha Ahmed Alamodi Alghamdi, Assistant Professor, King Khalid University, Abha, Saudi Arabia, Email:
Abstract
Background: Breast cancer is the most common neoplastic change in women worldwide. The lifetime risk of breast cancer is one in five. Mammography-based screening estimates that 5.8 per 1000 Saudi women aged >40 years have breast cancer. Breast cancer affects Saudi women at an early age compared to developed countries. Most cases are detected at later stages, leading to lower rates of complete, sustained remission. The recovery rate of early detected cases may exceed 90%. This study aims to estimate the prevalence and risk factors of breast cancer among women in Saudi Arabia. Additionally, public knowledge regarding breast cancer is assessed. Materials & Methods: A total sample of 496 female school teachers aged between 22 and 64 years working in primary, intermediate, and secondary schools from the Aseer region was evaluated by a questionnaire after taking their informed consent. School teachers were selected by a multistage random sampling method. Data were collected via a structured questionnaire containing elements on demographics, knowledge regarding the value of self- and clinical breast examination and screening mammography. Approval from the Research Ethical Committee at King Khalid University was obtained and conducted after approval. Collected data were subjected to statistical analysis. Results: A total sample of 496 female school teachers aged between 22 and 64 years were involved in the study. Mean age was 37.6 ± 10.1 (range: 15-64) years, 76% were married, and the median number of children among married participants was 3 (Interquartile range: 2-5) children. Mean age at menarche and birth of first child were 13.1 ± 2.1 and 24.5 ± 4.7 years, respectively. A total of 56% of women reported history of breastfeeding, 38% used oral contraceptive pills, 32% were obese, and 3% were smokers. About two third (73%) of participants reported that they will visit doctor if they notice a lump or anything abnormal during the examination of breast. Majority of the participants (62%) were agreed that clinical examination of the breast must be done before doctor. Additionally, 67% reported knowledge of how to perform breast self-examination. Self-examination was taught by healthcare providers in 82% of cases. Participants said that the age at which BSE should be done at puberty (21%), after 20 years (21%), after 30 years (31%) and 27% said they do not know. Conclusions: Among this sample of middle-aged women, awareness of breast cancer and the value of self- and clinical breast examination is high. Nevertheless, a minority of patients reported never examining their breast for masses. Future studies should focus on improving early detection of breast cancer.
Keywords
Awareness, Knowledge, School teachers, Breast cancer, Breast self-examination, Saudi ArabiaIntroduction
Worldwide, breast malignancy is the 2nd most typical malignancy and the 5th reason behind cancer-related mortality [1]. Breast cancer most common malignancy to affect ladies; in fact, it is 2nd to lung cancer because of the primary reason behind cancer-associated deaths involving females [2,3]. In low- and middle-income nations (LMICs), it continues to be a substantial public health problem as incidence rates have been proven to increase annually by around 5%, with over 1 million expected new cases yearly by 2020 [4,5]. The emergence of breast illness and following the advancement of cancer is apparently more intense in young ladies in comparison to its progression in older women [6]. Worldwide statistics display that the yearly morbidity and mortality of BC are usually growing, where over 1.15 million women globally (addressing ten percent of all identified cancers and 23 % of cancers identified in women) are identified as having BC every year, and much more than 5,02,000 of them die out of this illness [7]. The aetiology of nearly all BCs is unfamiliar, with no more than 25% to 40% of these may be related to well-recognized risk aspects [8].
The higher morbidity and mortality of breast cancer can be decreased if the lesion is recognized in the early stages [2]. In this respect, women have to be "breasts aware" when you are in a position to recognize the risk factors and symptoms of breast malignancy and also risk reduction techniques. Women in the Middle East encounter an essential threat of higher mortality rate from BC because of the delay in the analysis and the sophisticated stages of the condition during medical diagnosis. In the Kingdom of Saudi Arabia, BC is generally diagnosed at an advanced stage and much more regularly in younger pre-menopausal women beneath the age group of 45 years compared to western nations [7].
In the year 2010, breast cancer was the ninth leading reason behind death for women inside the Kingdom of Saudi Arabia (KSA) [9]. Additionally, 1308 new breast cancer situations were documented in 2009, and about 25% of most new cancer cases were documented among Saudi females [10]. The occurrence of breast cancer, it was predicted, increases in the arriving decades in KSA because of the population's development and growing older [11]. In Saudi Arabia, sadly, we don't possess any nationwide screening program; nevertheless, there are many local programs such as for example, the public knowing of BC, through lectures, in a significant hospital in Riyadh [12], a year-round, well-designed general public awareness plan, and the initial structured population-cantered screening mammography plan in Al- Qassim region [13]. In Saudi Arabia, breast cancer generally offers at advanced levels and much more regularly in younger pre-menopausal age women weighed against Western countries [14]. Based on the Ministry of Health in Saudi Arabia, the amount of new cases of malignancy is 2741, which includes about 19% of breast malignancy in women that's ranked first figures [15]. In the USA, 50% of new breast cancer occurs in females over 65 years, whereas in Saudi Arabia, breast cancer generally occurs at age 52 years old. Furthermore, developed nations discover breast cancer mainly in the first stages compared to developing countries, where you can find large quantities diagnosed at advanced phases [15].
In accordance with ACS suggestions, women ought to know just how their breasts usually experience and report any shifts promptly to their doctors. BSE can be a choice for females beginning from the early 20s [16]. However, the late analysis of BC is principally due to insufficient awareness of the population and barriers to access to health providers (WHO, 2012) [17]. Though nevertheless clouded in conflict, breast self-examination (BSE) still comes with a critical function to play in the first diagnosis of breast malignancy in resourceconstraint settings where regular clinical breast evaluation and mammography might not be achievable. In such environments, BSE is preferred since it is free, personal, pain-free, easy, secure, and requires no special equipment. It has additionally been proven to boost breast health recognition and thus possibly enable early detection of breast anomalies [18]. Breast self-exam, or regularly examining your breasts on your own, can be an important way to find a breast cancer early, when it’s more likely to be treated successfully. While no single test can detect all breast cancers early, Breastcancer.org believes that performing breast self-exam in combination with other screening methods can increase the odds of early detection. Knowledge regarding screening strategies and risk factors and of the condition plays a significant and efficient function in creating and employing screening applications in a community that may effectively improve the likelihood of early recognition of BC in the first stages, which bring about improvement in survival rate and standard of living [19].
Many reports were carried out inside Saudi Arabia concerning the knowledge and practice of breast cancer screening procedures. In a report performed, the Breast Malignancy Screening in Saudi Arabia, it was discovered that among 10,735 individuals of the analysis, 89% of ladies reported devoid of a clinical breast examination, and 92% reported in no way having a mammogram [20]. Other research carried out the patterns, information, and barriers of mammography make use of among ladies in Saudi Arabia, and 3245 ladies were surveyed, with 40% reporting actually having a mammogram [21]. Many reports on BCS efficiency have already been implemented among ladies worldwide. Such research has integrated certain females’ groups such as for example, female university students, women workers, females participating in healthcare centers, or women occupants [14,16-19]. However, few studies have been reported on female teachers in the literature regarding BCS exercise in the world. Therefore, our research aimed to evaluate the knowledge, attitude, and practice of breast cancer screening approaches among female school instructor in the southern region of Saudi Arabia.
Materials and Methods
The current study was a cross-sectional survey, a population-based study that recruited 496 female schoolteachers in the Aseer region of Saudi Arabia. A total sample of 496 female school teachers aged between 22 and 64 years working in primary, intermediate, and secondary schools from the Aseer region was evaluated by a questionnaire after taking their informed consent. School teachers were selected by a multistage random sampling method. Fifty schools in the Aseer region were chosen randomly, and ten teachers were randomly selected from each school. Data were collected via a structured questionnaire containing elements on demographics, personal and family history of breast pathology, marital status and number of children, age at menarche and menopause (as applicable), breastfeeding, use of oral contraceptive pills, obesity, smoking, past mammography, and knowledge regarding the value of self- and clinical breast examination and screening mammography.
The pilot study was conducted on 30 patients to evaluate the content of the questionnaire and the average time it took to complete. Then, corrections were made accordingly. These 30 pilot study cases were not included in the main study. Face validity was also be assessed before the start of the study. Participants were informed about the nature of the study. Approval from the Research Ethical Committee at King Khalid University was obtained and conducted after approval.
Both descriptive and analytical statistical measurements were used to describe the main variables by SPSS 18 (IBM Corporation, Armonk, New York, USA) software. Descriptive statistics, including frequencies and percentage, was used to describe the frequency of each response for the categorical data. The statistical significance of the coefficients in the statistical analyses was tested at 0.05 (<=0.05) level.
Results
A total sample of 496 female school teachers aged between 22 and 64 years working in primary intermediate, and secondary schools from the Aseer region were involved in the study sample. Of the 550 questionnaires distributed, 496 (90.1%) were returned with properly filled, thus subjected to analysis. Mean age was 37.6 ± 10.1 (range: 15-64) years, 76% were married, and the median number of children among married participants was 3 (Interquartile range: 2-5) children. Mean age at menarche and birth of first child were 13.1 ± 2.1 and 24.5 ± 4.7 years, respectively. A total of 56% of women reported history of breastfeeding, 38% used oral contraceptive pills, 32% were obese, and 3% were smokers (Table 1).
| Variables | Frequency N (496) | Percentage (%) |
|---|---|---|
| Age group | ||
| < 30 | 128 | 26 |
| 30-39 | 120 | 24 |
| >40 | 248 | 50 |
| Social status | ||
| Single | 121 | 24 |
| Married | 375 | 76 |
| Number of children | ||
| 0 | 48 | 10 |
| 1-2 | 104 | 21 |
| 3-4 | 214 | 43 |
| >5 | 130 | 26 |
| Age at first birth | ||
| <20 Years | 78 | 16 |
| 20-29 years | 257 | 52 |
| >30 Years | 40 | 8 |
| Puberty | ||
| 9-11 years | 6 | 1 |
| Â 12-15 years | 390 | 79 |
| Â >15 years | 100 | 20 |
| Breastfeeding | ||
| Yes | 277 | 56 |
| No | 219 | 44 |
| Use of birth control pills | ||
| Yes | 188 | 38 |
| Â No | 308 | 62 |
| Obesity | ||
| Â Yes | 159 | 32 |
| Â No | 337 | 67 |
| Smoking | ||
| Â Yes | 14 | 3 |
| Â No | 482 | 97 |
| n=Number; %=Percentage. | ||
Table 1: Frequency distribution of Socio-demographic characteristics of the included 496 female schoolteachers in Aseer region of Saudi Arabia.
Participants who reported hearing about breast cancer comprised 99% of the sample. Source of knowledge was reported to be social media in 88% of patients. Family history of breast cancer was reported by 19% of women, and 5% had history of breast cancer in first-degree relatives (Table 2). About two third (73%) of participants reported that they will visit doctor if they notice a lump or anything abnormal during the examination of breast.
| VARIABLES | Frequency N (496) | Percentage (%) |
|---|---|---|
| Have you heard about breast cancer | ||
| Â Yes | 490 | 99 |
| No | 6 | 1 |
| What is the source of your information? | ||
| Books | 61 | 12 |
| Social Media (TV, Radio, Internet) | 435 | 88 |
| Is there a family with breast cancer in the family? | ||
| Yes | 94 | 19 |
| No | 402 | 81 |
| If the answer is yes, what is the relationship of kinship? | ||
| Sister | 17 | 18 |
| Mother | 10 | 11 |
| Aunt and maternal uncle | 40 | 43 |
| Cousin | 27 | 28 |
| If you notice a lump or anything abnormal during the examination, what are you doing? | ||
| Visit a doctor | 358 | 72 |
| Make necessary checkup | 128 | 26 |
| Nothing | 10 | 2 |
| Have you ever had a breast examination? | ||
| Yes | 288 | 58 |
| No | 208 | 42 |
| Have you heard about clinical breast examination? | ||
| Yes | 222 | 45 |
| No | 274 | 55 |
| Did you know that a clinical breast examination helps with early detection of breast cancer? | ||
| Yes | 292 | 59 |
| No | 204 | 41 |
| The clinical examination of the breast must be done before | ||
| Doctor | 309 | 62 |
| Patient himself | 12 | 2 |
| Nurse | 12 | 2 |
| I do not know | 163 | 34 |
| The clinical examination of the breast must be done by | ||
| Â Television Acoustic Radiology | 76 | 15 |
| Mammogram | 139 | 28 |
| Hand | 41 | 8 |
| I do not know | 240 | 49 |
| Have you heard of mammograms? | ||
| Â Yes | 278 | 56 |
| Â No | 218 | 44 |
| Do you think mammograms are a means of early detection of breast cancer? | ||
| Â Yes | 370 | 75 |
| Â No | 126 | 25 |
| At what age the mammogram begins to be used | ||
| After menopause | 93 | 19 |
| At the age of 20 years | 25 | 5 |
| At the age of 30 years | 177 | 35 |
| I do not know | 203 | 41 |
| Have you ever done a mammogram? | ||
| Â Yes | 59 | 12 |
| Â No | 437 | 88 |
| If your answer is no, what is the reason? | ||
| Age does not agree to do a mammogram | 104 | 24 |
| A mammogram is not available | 141 | 32 |
| Because of a physical deficiency | 192 | 44 |
| n=Number; %=Percentage. | ||
Table 2: Frequency distribution of knowledge, and attitude towards breast cancer in 496 female schoolteachers in Aseer region of Saudi Arabia.
Moreover, 42% had no breast examination done before and 55% did not heard about clinical breast examination. Majority of the participants (62%) were agreed that clinical examination of the breast must be done before doctor. Unfortunately, nearly half of the participants (49%) said that they do not know how the clinical breast examination must be done. When asked about mammogram done before, 88% of participants said ‘No’.
Overall, 93% of participants reported hearing about breast self-examination, including 84% who were aware that breast self-examination improves early recognition of breast cancer. Additionally, 67% reported knowledge of how to perform breast self-examination. Selfexamination was taught by healthcare providers in 82%of cases (Table 3). Less than half (48%) said that they do not know how often the mammogram done, but 28% said it should be done only with clinical breast examination discovers a lump (Figure 1). Nearly about 34% of participants said that clinical examination of breast should be performed when there is something abnormal in the BSE (Figure 2). More than the half of the participants (54%) said that the best time to do the BSE is weak after menses and as little as 4% agreed to do during breastfeeding (Figure 3). Participants said that the age at which BSE should be done at puberty (21%), after 20 years (21%), after 30 years (31%) and 27% said that they do not know (Figure 4).
| Variables | Frequency N (496) | Percentage (%) |
|---|---|---|
| Have you heard about breast self-examination? | ||
| Yes | 461 | 93 |
| No | 35 | 7 |
| Did you know that breast self-examination helps with early detection of breast cancer? | ||
| Â Yes | 418 | 84 |
| No | 78 | 16 |
| Have an idea of how breast self-examination is applied? | ||
| Yes | 329 | 66 |
| No | 167 | 34 |
| If the answer is yes, you know that by | ||
| Doctor | 219 | 67 |
| Teacher | 45 | 14 |
| Nurse | 23 | 7 |
| Parents | 42 | 12 |
| Breast self-examination must be done before. | ||
| Doctor | 87 | 18 |
| Person himself | 354 | 71 |
| I do not know | 55 | 11 |
| Breast self-examination was done with | ||
| Observation and viewing of a woman's breast | 370 | 76 |
| Breast exam by hand | 446 | 90 |
| Armpit hand examination | 381 | 76 |
| Modern breast TV work | 188 | 38 |
| Mammogram | 168 | 34 |
| What is the benefit of breast self-examination? | ||
| Early detection of breast cancer | 361 | 73 |
| Breast Message | 2 | 0.4 |
| Knowing the types of breast tissues | 133 | 26.6 |
| While doing a breast self-examination, did you notice any change? | ||
| Yes | 105 | 21 |
| No | 391 | 79 |
| Do you think breast self-examination is important? | ||
| Yes | 480 | 96 |
| No | 16 | 4 |
| n = Number; % = Percentage. | ||
Table 3: Frequency distribution of Knowledge, practice and perceived importance of breast self-examination among female schoolteachers.
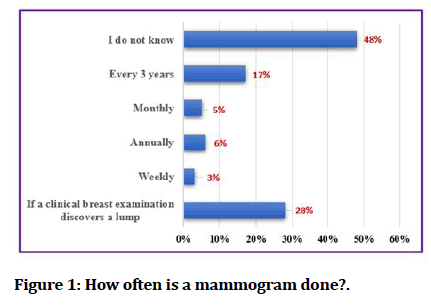
Figure 1: How often is a mammogram done?.
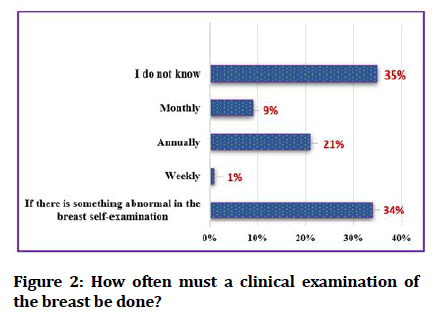
Figure 2:How often must a clinical examination of the breast be done?
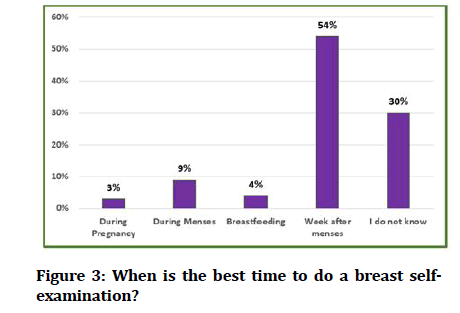
Figure 3:When is the best time to do a breast selfexamination?
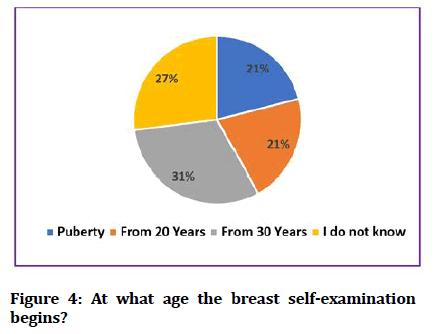
Figure 4:At what age the breast self-examination begins?
Discussion
The knowing of breast cancer plays a significant role in early recognition and prevention of the condition, and primary health care centers will be the first degree of contact among women and families within the health care system. A rise in understanding of breast cancer screening methods will result in early intervention and analysis of breast cancer and also increased survival. A report conducted in Saudi Arabia by Ibrahim et al. approximated that the near future burden of breast cancer in Saudi Arabia is likely to enhance by around 350% by 2025 [22]. Another significant element why we encounter past due presentation of breast cancer is that a lot of women do not perform BSE, and they usually do not also make use of the screening part of mammography. It really is either they have never heard about BSE, or they don't understand how to make it out [23-25]. Additionally, it is possible they can perform BSE; however, the motivation to transport it out is absent. The majority of the participants had been aware of Breast malignancy and BSE but just not even half of the individuals had found out about CBE. Our results can be weighed against earlier research in Najran (Saudi Arabia) that showed over fifty percent of women were alert to breast cancer, but not even half of them had been unacquainted with early detection methods [26]. Furthermore, a report in Abha (Saudi Arabia) demonstrated that not even half (41.5%) and several women (22%) possess heard about breast selfexaminations and mammograms, respectively [27]. Another research of feminine teachers in Buraidah (Saudi Arabia) showed they had a limited understanding of breast cancer [28]. Therefore, this research may lead healthcare providers to motivate women to apply breast cancer screening solutions to reduce the occurrence of breast cancer.
Participants’ awareness linked to BSE has also been acceptable; most individuals had been aware of the significance of BSE. This obtaining is much greater than knowledge prices for BSE observed in various other studies [28-30]. The current research showed that nearly half of the participants (58%) of women possess execute breast self-examinations. In an identical study, just a third of ladies had performed breast self-examinations [27] whereas, within an additional study, greater than a 3rd of women performed breast self-examinations [31]. A number of studies about BSE have reported comparable findings [28,31-33]. This can be due to poor health knowledge inside our society. In a report done among secondary college teachers, no more than 25% had an adequate understanding of breast self-exams [33]. The effects, therefore, are that 75% of this type of band of teachers cannot affect their students the significance of BSE [33]. To boost the knowledge of breast cancer inside women, healthcare providers train women the way in which to execute breast self-examinations and tell them of the standard structure of the breasts to improve their capability to recognize abnormalities and how exactly to record the abnormalities to healthcare providers.
Furthermore, just 54 % of the instances knew the optimum time to accomplish BSE, with 9 % stating that it's best during menstrual circulation and 30% having only no idea on the optimum time to accomplish BSE (Figure 3). A report performed amongst females in Al- Ahsa (Saudi Arabia) suggested the critical reason why Saudi women didn't experience breast cancer screening practices. Approximately half of the participants 161 (50.5%), have no idea how the check was performed, 155 (48.6 %) feel pain through the screening, 152 (47.6%) didn't have leisure time to end up being screened, 154 (48.3%) sense humiliated from the screening, and 129 (49.4 %) concern with excellent results. Our findings were much like previous research that indicated a minimal percentage of women experienced a mammogram [22,27,28,34,35]. The United States University of Obstetricians and Gynecologists and the United states Cancer Community offer mammograms at age 40 years old [22]. In Saudi Arabia, the federal government provides mammograms absolve to the populace by means of healthcare providers. Despite the fact that the federal government provides mammograms free of charge, still, nearly all women do not use these services. Regarding the screening options for detecting the condition, the individuals (25%) in this research didn't know about the usage of mammography, and 88% of participants hadn't done a mammogram in the past as a screening device for early recognition of breast cancer.
This finding in addition, has been documented in previous studies [27,35,36]. Health education concerning the great things about mammography screening for recognition of breast cancer ought to be motivated. A study carried out in Al Madinah; the imply age group of the studied 465 ladies was 34.9 ± 12.24 months. Of the women, 27.7% and 38.5% obtained mammography and performed BSE, respectively [37]. Medical breast examinations are usually another way for breast screening. The outcomes from our study could be weighed against earlier studies in Saudi Arabia [31], significantly less than 3rd in Buraidah and Al Hassa [28,35], obtained clinical breast examinations.
In the current study, the primary way to obtain information regarding breast cancer was from social media marketing, which was much like a previous study [27]. These findings have directed us to utilize social media to greatly help increase the understanding of breast cancer screening methods also to motivate the population to execute these procedures. The Ministry of Wellness in Saudi Arabia hosted an annual occasion that is expected to improve the knowledge of breast cancer during International Breast Cancer Awareness Month that has been kept in October [38]. A report in Egypt (2000), showed that the primary source was peer organizations and doctor was the least way to obtain details. This may be credited to the very long time that females spent with one another at the place of work, discussing different issues [39]. Although WHO documented that health groups play a significant role in teaching, guidance, and convincing women to apply BSE. A report performed by Kratzke figured television, radio, and the Web are the second way to obtain information (16.4%). The most typical information sources were Web (75%), magazines (69%), suppliers (76%), and friends (61%). Minimal common resources were radio (44%), papers (34%), and mothers (36%) [40]. Inside a report done among secondary college teachers, no more than 25% had enough understanding of breast self-evaluation [33]. Therefore, the implication is that 75% of this type of band of teachers cannot affect their students the significance of BSE. The data of the usage of mammography as a screening device for early recognition of breast cancer was found to become bad among our participants. Just 14.3% of the participants have found out about screening mammography. An identical finding was documented by Okobia et al. [41]. Health education concerning the great things about mammography screening ought to be encouraged. Freeman et al., also emphasized the necessity for adolescents to end up being appropriately taught the program of BSE as this can significantly impact their exercise because they grow older [42]. Over the years, there has been some debate over just how valuable breast self-examination is in detecting breast cancer early and increasing the likelihood of survival. For example, a 2008 study of nearly 400,000 women in Russia and China reported that breast self-examination does not have a meaningful impact on breast cancer survival rates and may even cause harm by prompting unnecessary biopsies (removal and examination of suspicious tissue). Because of the on-going uncertainty raised by this and other studies, the American Cancer Society no longer recommends breast self-exam as a screening tool for women with an average risk of breast cancer.
Early detection remains the primary way to prevent the development of life-threatening breast cancer. Breast cancers that are detected when smaller or no palpable are more treatable and thus are associated with a more favourable prognosis.
Imaging studies used in breast cancer screening include the following [43]
Mammography.
Ultrasonography.
Magnetic resonance imaging (MRI).
The survival benefit of first detection with mammography screening has been confirmed. However, improvements in imaging technology and disagreements over suggested schedules have difficult the issue of screening. As with any cancer screening program, very careful consideration should be directed at the risks of establishing breast malignancy along with the advantages and causes harm to of the screening intervention, together with the expense involved.
Early detection is widely endorsed by organizations that issue clinical recommendations for breast cancer care. Many expert groups have offered their recommendations for breast cancer screening, and much of the controversy lies in the fact that there is not a consensus about when to begin and end screening, how often to screen, and by what technique? These groups include the following [43]:
American Cancer Society (ACS).
American College of Obstetricians and Gynecologists (ACOG).
American College of Physicians (ACP).
American College of Radiology (ACR).
American Medical Association (AMA).
National Cancer Institute (NCI).
National Comprehensive Cancer Network (NCCN).
United States Preventive Services Task Force (USPSTF).
Guidelines [43]
For women younger than 40 years at average risk for breast cancer, there have no been randomized scientific studies carried out to recommend an advantage to screening. The numerous professional teams haven't reached a consensus among them, but several recommend a clinical breast exam (CBE) every three years and a conversation about the advantages and limitations of breast self-exam (BSE). For women older than 40 years at average risk for breast cancer, numerous expert groups suggest CBE annually. In terms of imaging, probably the most broadly suggested screening method in the United States for this group has been yearly mammography. Controversially, however, current guidelines vary with regards to the suggested age to start regular mammography (eg, 40, 45, or 50 years) and whether to perform mammography yearly or biennially. Recommendations concerning interruption of mammography also differ, with both age group-typically, 75 years and life span as criteria. For testple, the American College of Radiology advises annual mammography screening before life expectations is significantly less than 5 to 7 yrs., dependent on comorbidities.
Even though mammography guidelines have been in place for over 30 years, 20-30% of women still usually do not undergo screening as indicated. The two most important aspects in determining whether a woman undergoes mammographies are physician suggestion and access to health insurance.
Non-white women and the ones of lower socioeconomic status remain less inclined to acquire mammography services, and these women will provide with life-threatening, advanced-stage disease.
National comprehensive cancer network guidelines [43]
The NCCN on screening in average-risk women includes the following recommendations:
Clinical breast examinations every 1-years from age 25-39, then annually from age 40 on Begin annual screening mammography at age 40 years. Consider tomosynthesis (three-dimensional mammography)
NCCN guidelines provide four separate sets of recommendations for women at increased risk on the basis of personal or family history; These include earlier initiation of mammography, in some cases, and consideration or recommendation of annual MRI. Additional considerations include the following: [43]
An upper age limit for screening is not yet established. Consider severe comorbid conditions limiting life expectancy (eg, ≤10 years) and whether therapeutic interventions are planned.
For women with heterogeneously dense breasts and dense breast tissue, we recommend counselling on the risks and benefits of supplemental screening.
Dense breasts limit the sensitivity of mammography and are associated with an increased risk for breast cancer.
Full-field digital mammography appears to benefit young women and women with dense breasts.
Multiple studies show that tomosynthesis can decrease call-back rates and appears to improve cancer detection. Most studies used double the dose of radiation, but the radiation dose can be minimized by using synthesized 2- D reconstruction.
Hand-held or automated ultrasound can increase cancer detection but may increase recall and benign breast biopsies.
Current evidence does not support the routine use of thermography or ductal lavage as screening procedures.
Self-examination and clinical examination [43]
Breast self-examination (BSE) and clinical breast exam (CBE) is affordable and non-invasive methods for the standard assessment of breasts (ie, monthly BSE and yearly CBE). Evidence assisting the effectiveness of these 2 screening methods is debatable and primarily inferred. Despite having suitable training, BSE has not been observed to decrease breast cancer mortality. The majority of the professional groups have revised their recommendations to add discussions about the advantages and limitations of this technique or a more standard education about breast self-awareness. For instance, ACOG distinguishes between BSE, which it will not suggest, from breast self-awareness, which it encourages. Unlike BSE, breasts self-awareness does not involve routine or systematic breast self-examination for the purpose of finding breast cancer. Alternatively, this is a woman's attunement to the standard appearance and feel of her breasts in order that she can inform her doctor if she encounters breast changes such as pain, a mass, new onset of nipple discharge, or redness. With increasing improvements in treatment regimens for earlier, localized disease, CBE, especially among women younger than 40 years, is still recommended by many organizations, which includes ACOG and ACS. Randomized clinical trial results support combining CBE with mammography to improve screening sensitivity, particularly in more youthful ladies in whom mammography could be less effective and in women who receive mammograms almost every other year instead of annually.
Early detection of breast cancer plays a pivotal role in reducing related mortalities. Until conditions are usually favorable for regular mammographic screening in resource-limited settings, the focus ought to be oriented towards encouraging ladies to exercise BSE regularly. Our results suggest the necessity to increase knowing of BSE as a screening device since it renders women even more “breast aware” and, therefore, potentially enable early detection of breast cancer. By doing this, numerous breast-conserving procedures which include lumpectomy, segmentectomy, and quadrantectomy could be warranted in individuals with early-phase cancers as opposed to the usually feared mastectomy. Increasing consciousness on the options of breast reconstruction surgical treatment can be warranted as this might enhance medical assist seeking attitudes of victims. The conclusions of the study suggested the number of avenues for long term study and may be used to donate to the advancement of preventative and screening applications for breast cancer over the population. This research emphasizes the necessity to raise breast cancer awareness also to teach individuals concerning the need for practices for early recognition methods, such as for example, BSE, that may enable breast cancer to end up being recognized at a youthful phase. We recommend that schoolteachers be looked at as a particular group that should receive home elevators for breast cancer.
Conclusion
Among this sample of middle-aged women, awareness of breast cancer and the value of self- and clinical breast examination is high. Nevertheless, a minority of patients reported never examining their breasts for masses. Future research should concentrate on enhancing the first detection of breast cancer. In the first recognition of breast cancer, breast self-examination is really a safe, efficient, and economical screening approach. Practicing BSE could offer an possibility for women to understand how their breasts usually feel and capable to discern changes within their breast tissue. Women who practice BSE have an increased chance of earlier detection, and by this way, survival rates can increase, and treatment plans can be end up beingtter. Breastcancer.org still feels that breast self-examination is a helpful and essential screening tool, specifically when used in combination with regular physical exams by method of a medical doctor, mammography, and in some cases ultrasound and/or MRI. Each of these screening equipment works in a various way and has strengths and weaknesses. Breasts self-exam is a hassle-free, no-cost tool which you can use {on a normal basis and at any given age.
Conflicts of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: Globocan 2008. Int J Cancer 2010; 127:2893-917. Indexed at, Google Scholar, Cross Ref
- https://www.who.int/health-topics/cancer
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in Globocan 2012. Int J Cancer 2015; 136:E359-86.
- Anderson B, Shyyan R, Eniu A, et al. Breast cancer in limited-resource countries: An overview of the breast health global initiative 2005 guidelines. Breast J 2006; 12:3-15.
- https://www.uicc.org/news/iarc-release-latest-world-cancer-statistics#:~:text=According%20to%20GLOBOCAN%202012%2C%20an,million%2C%20respectively%2C%20in%202008.
- Anders C, Hsu D, Broadwater G, et al. Young age at diagnosis correlates with worse prognosis and defines a subset of breast cancers with shared patterns of gene expression. J Clin Oncol 2008; 26:3324-3330.
- https://gco.iarc.fr/
- https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2009/cancer-facts-and-figures-2009.pdf
- Mokdad AH, Jaber S, Aziz MI, et al. The state of health in the Arab world, 1990–2010: An analysis of the burden of diseases, injuries, and risk factors. Lancet 2014; 383:309-20.
- http://www.scr.org.sa/?module= publications&page=list&id=46&page_num=1. Accessed 7 Nov 2014
- Ibrahim EM, Zeeneldin AA, Sadiq BB, et al. The present and the future of breast cancer burden in the Kingdom of Saudi Arabia. Med Oncol 2008; 25:387-93.
- Abulkhair OA, Al Tahan FM, Young SE, et al. The first national public breast cancer screening program in Saudi Arabia. Annals Saudi Med 2010; 30:350-357.
- Ravichandran K, Al-Hamdan NA, Mohamed G. Knowledge, attitude, and behavior among Saudis toward cancer preventive practice. J Family Comm Med 2011; 18:135.
- Abolfotouh MA, Ala’a AB, Mahfouz AA, et al. Using the health belief model to predict breast self-examination among Saudi women. BMC Public Health 2015; 15:1-2.
- http://www.moh.gov.sa/en/HealthAwareness/Campaigns/Breastcancer/Pages/default.aspx
- Salaudeen AG, Akande TM, Musa OI. Knowledge and attitudes to breast cancer and breast self-examination among female undergraduates in a state in Nigeria. Eur J Soc Sci 2009; 7:157-64.
- Abulkhair OA, Al Tahan FM, Young SE, et al. The first national public breast cancer screening program in Saudi Arabia. Annals Saudi Med 2010; 30:350-7.
- Nde FP, Assob JC, Kwenti TE, et al. Knowledge, attitude and practice of breast self-examination among female undergraduate students in the University of Buea. BMC Rese Notes 2015; 8:1-6.
- Elmore JG, Armstrong K, Lehman CD, et al. Screening for breast cancer. JAMA 2005; 293:1245-56.
- El Bcheraoui C, Basulaiman M, Wilson S, et al. Breast cancer screening in Saudi Arabia: Free but almost no takers. Plos One 2015; 10:e0119051.
- Al-Wassia RK, Farsi NJ, Merdad LA, et al. Patterns, knowledge, and barriers of mammography use among women in Saudi Arabia. Saudi Med J 2017; 38:913.
- Yousuf SA. Breast cancer awareness among Saudi nursing students. JKAU Med Sci 2010 ; 17:67-78.
- Osime OC, Okojie O, Aigbekaen ET, et al. Knowledge attitude and practice about breast cancer among civil servants in Benin City, Nigeria. Ann Afr Med 2008; 7:192–7.
- Rutledge DN, Barseric KA, Knobf MT, et al. Breast cancer detection: Knowledge, attitude and behaviour of women from Pennsylvania. Oncol Nurs Forum 2001; 28:1032–40.
- Abdel-Fattah M, Zaki A, Bassili A, et al. Breast self-examination practice and its impact on breast cancer diagnosis in Alexandria, Egypt. East Mediterr Health J 2000; 6:34–40.
- Alshahrani M, Alhammam SYM, Al Munyif HAS, et al. Knowledge, attitudes, and practices of breast cancer screening methods among female patients in primary healthcare centers in Najran, Saudi Arabia. J Cancer Edu 2018; 34:1167–1172.
- Mahfouz AA, Hassanein MH, Nahar S, et al. Breast cancer knowledge and related behaviors among women in Abha city, southwestern Saudi Arabia. J Cancer Educ 2013; 28:516-520.
- Dandash KF, Al-Mohaimeed A. Knowledge, attitudes, and practices surrounding breast cancer and screening in female teachers of Buraidah, Saudi Arabia. Int J Health Sci 2007; 1:61.
- Renganathan L, Ramasubramaniam S, Al-Touby S, et al. What do Omani women know about breast cancer symptoms?. Oman Med J 2014; 29:408.
- Rakkapao N, Promthet S, Moore MA, et al. Development of a breast cancer awareness scale for Thai women: Moving towards a validated measure. Asian Pac J Cancer Prev 2016; 17:851–6.
- Alam AA. Knowledge of breast cancer and its risk and protective factors among women in Riyadh. Annals Saudi Med 2006; 26:272-7.
- Hassan I, Onakek EE, Mabogunje AO. Breast cancer in Nigeria. J R Coll Surg Edinb 1992; 37:159-61.
- Odusanya OO, Tayo OO. Breast cancer knowledge, attitudes and practice among nurses in Lagos, Nigeria. Acta Oncol 2001; 40:844-8.
- Alshahrani M, Alhammam SY, Al Munyif HA, et al. Knowledge, attitudes, and practices of breast cancer screening methods among female patients in primary healthcare centers in Najran, Saudi Arabia. J Cancer Educ 2019; 34:1167-72.
- Al-Suroj HR, Al Ali FB, Al-Saleh KH, et al. Awareness and Attitude among Saudi Females toward Breast Cancer Screening in Al-Ahsa, KSA. Egyptian J Hospital Med 2018; 71:2516-2522.
- Alharbi N, Alshammari M, Almutairi B, et al. Knowledge, awareness, and practices concerning breast cancer among Kuwaiti female school teachers. Alexandria J Med 2012; 48:75-82.
- Al‑Zalabani AH, Alharbi KD, Fallatah NI, et al. Breast cancer knowledge and screening practice and barriers among women in Madinah, Saudi Arabia. J Cancer Educ 2018; 33:201‑7.
- https://www.moh.gov.sa/en/
- Seif NY, Aziz MA. Effect of breast self-examination training program on knowledge, attitude and practice of a group of working women. J Egyptian Nat Cancer Inst 2000; 12:105-115.
- Almutairi KM, Ahmad M, Vinluan JM, et al. Random cross‑sectional determination of the level of awareness among female Saudi patients about breast cancer. J Cancer Educ 2016; 31:131‑5.
- Okobia MN, Bunker CH, Okonofua F, et al. Knowledge, attitude and practice of Nigerian women towards breast cancer: A cross-sectional study. World J Surg Oncol 2006; 4:11–6.
- Freeman AG, Scott C, Waxman A, et al. What do adolescent females know about breast cancer and prevention? Pediatr Adolesc Gynecol 2002; 13:96–8.
- https://emedicine.medscape.com/article/1945498-overview
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Assistant Professor, King Khalid University, Abha, Saudi ArabiaCitation: Maha Ahmed Alamodi Alghamdi, Breast Cancer in Southern Saudi Arabia: Prevalence, Risk Factors and Attitude, J Res Med Dent Sci, 2022, 10(2): 794-804
Received: 29-Jan-2022, Manuscript No. Jrmds-22-55016; , Pre QC No. JRMDS-22-55061 (PQ); Editor assigned: 31-Jan-2022, Pre QC No. JRMDS-22-55061 (PQ); Reviewed: 14-Feb-2022, QC No. JRMDS-22-55061; Revised: 18-Feb-2022, Manuscript No. JRMDS-22-55061 (R); Published: 25-Feb-2022
