Case Report - (2020) Volume 8, Issue 2
Cerebral Infarction Following Intra-Tonsillar Injection of Phenol in a Child
Lawan Musa Tahir1*, Lokman Cam1*, Atilla Emiroglu2, Mehmet Sina3 and Senol Dane4
*Correspondence: Lawan Musa Tahir, Departments of Pediatrics, Faculty of Basic Medical Sciences, College of Health Sciences, Nile University of Nigeria, Abuja, Nigeria, Email: Lokman Cam, Departments of Pediatrics, Faculty of Basic Medical Sciences, College of Health Sciences, Nile University of Nigeria, Abuja, Nigeria, Email:
Abstract
An apparently well early adolescent presented at the emergency unit with history of multiple convulsions and left sided hemiparesis within 2 hours of receiving intra-tonsillar injection of phenol. Brain MRI showed features of acute infarction of right middle cerebral artery-posterior cerebral artery. He was treated with subcutaneous clexane and Nootropil, Omeprazole, Vitamin B complex and diazepam infusions. He was also given oral carbamazepine, Aspirin and Vitamin E. He responded well, there was no seizure while on admission and had started moving both the left upper and lower limbs within 72 hours. There is no information about intra-tonsillar local phenol injection to treat tonsillitis in literature. Therefore, intra-tonsillar, oral or parenteral phenol usage should be evaluated as a medical malpractice.
Keywords
Phenol injection, Tonsillitis, Seizures, Cerebral infarct
Introduction
Phenol is an aromatic organic compound with the molecular formula C6H5OH. Phenols are widely used in household products and as intermediates for industrial synthesis. For example, phenol itself is used (in low concentrations) as a disinfectant in household cleaners and in mouthwash. Phenol is also a surgical antiseptic. It is mildly acidic and can cause chemical burns in the skin. Tonsillitis is a leading disease in otolaryngology, and the admission for tonsillitis was found to rise by 310% between 2003 and 2011 in the United Kingdom [1,2]. Sprays and medicated lozenges containing phenol are no more effective than candy at relieving throat pain and are not recommended because of the risk for methemoglobinemia and allergic reactions [3]. Up to now, there is no information about intra-tonsillar local phenol injection which occurred in our case to treat tonsillitis in literature. Therefore, oral or parenteral phenol usage should be evaluated as a medical malpractice.
Case Report
A 13 years old boy was rushed into our emergency unit at 1.50 am, from another private hospital, on account of multiple convulsions which started after intra-tonsillar injection of phenol. He presented to the referring hospital with complaints of recurrent tonsillitis (3 to 4 times per year). He was said to have been evaluated and offered tonsillectomy, but parents declined. He was then offered the phenol injection therapy. His clinical state before the injection was described as very good. Body temperature was 36.40C, pulse rate was 64 beats per minute and other examination findings were essentially normal. He was giving injection phenol 1 ml into each tonsil and was said to immediately reacted, he could not move his left upper and lower limbs. At about two and a half hours after the injections he started generalized tonic-clonic seizures. He was commenced on diazepam infusion and carbamazepine. He had 4 seizures before referral and another 3 before arrival, each lasted for about 2 minutes.
On examination on admission, he was drowsy (sedated), afebrile (temperature of 36.60C), had pulse rate of 106 beats per minute, respiratory rate of 22 cycles per minute and SPO2 of 98%. He had loss of left nasolabial fold and left hemiparesis. There were no meningeal signs. Results of investigation showed leukocytosis, neutrophilia and thrombocytosis. His hemoglobin genotype was “AA’’ and clotting profile (PT, APTT and INR) were normal. Electrolytes, urea, creatinine and liver function tests were also normal. The ECG and echocardiography were normal. Brain MRI showed features of right middle cerebral artery-posterior cerebral artery acute infarction (Figure 1).
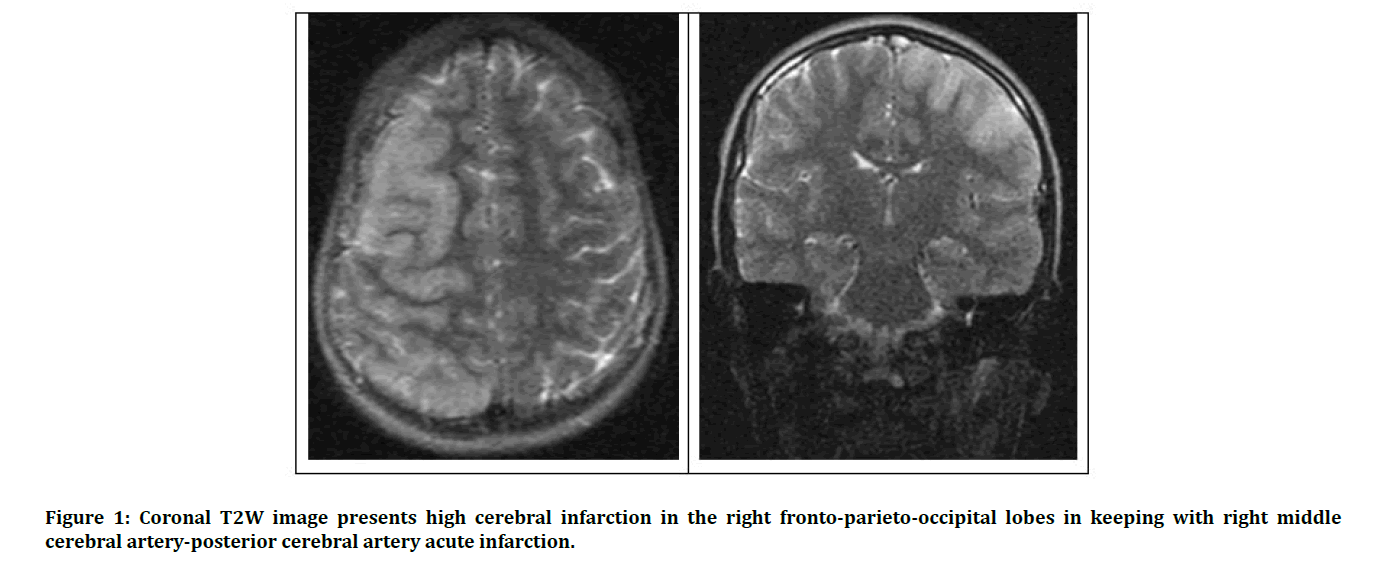
Figure 1: Coronal T2W image presents high cerebral infarction in the right fronto-parieto-occipital lobes in keeping with right middle cerebral artery-posterior cerebral artery acute infarction.
He was treated with subcutaneous clexane 0.4 unit daily, IV Nootropil (Piracetam) 1g by infusion daily, IV Omeprazole 40 mg daily, Vitamin B complex infusion and diazepam infusion. He was also given oral carbamazepine 100 mg bd, tabs Aspirin 75 mg daily and caps Vitamin E 1000 iu daily. He responded well, there was no seizure while on admission and had started moving both the left upper and lower limbs within 72 hours.
Discussion
Sore throat (tonsillitis/pharyngitis) is a common problem in childhood and adolescence. Most etiological agents are viral and thus self-limited; such patients require only symptomatic and supportive treatments [4]. Group A beta-hemolytic Streptococcus is the commonest bacterial agent that causes pharyngitis and the only agent linked to acute rheumatic fever and rheumatic heart disease [4,5]. Appropriate antibiotic therapy reduces the duration of symptoms, diminishes transmission, decreases the likelihood of suppurative complications such as retropharyngeal and peritonsillar abscesses, and prevents the development of acute rheumatic fever [4,6]. According to the guidelines, clinicians may recommend tonsillectomy for recurrent throat infection with a frequency of at least 7 episodes in the past year, at least 5 episodes per year for 2 years, or at least 3 episodes per year for 3 years with documentation in the medical record for each episode of sore throat and at least 1 of the following: temperature of at least 38.50 C, cervical adenopathy, tonsillar exudate, or positive test for group A beta hemolytic streptococcus.
Our patient did not meet the criteria for tonsillectomy [7-9] and conservative management and antibiotic therapy could have been adequate. There was paucity of data on recommendation for the use of intra-tonsillar injection of phenol. Phenol in small concentration (1.4%) is used, cautiously, in mouth wash and sprays for pharyngitis and to numb the pain of mouth and lip ulcers [9]. Phenol injection is given intramuscularly to treat severe muscle spasticity that results from cerebral palsy, Parkinson’s disease or brain trauma. It’s used on more severe ingrown toenails that don ’ t respond to other treatments (matrixectomy) [8]. Phenol was used as surgical antiseptic; its use was limited by its toxicity and ability to cause severe but painless burns of the skin and mucous membrane. Phenol and its vapours are corrosive to the eyes, the skin, and the respiratory tract. The substance may cause harmful effects on the central nervous system and heart, resulting in dysrhythmia, seizures, and coma [10,11]. Our patient had multiple convulsions which could be one of the side effects of phenol. The MRI finding could suggest that the phenol injection may have entered the cerebral circulation through the ascending pharyngeal branch of the external carotid, one of the arterial supplies to the palatine tonsils (Figure 1).
Phenol injection for treatment of tonsillitis is not an established practice and could be dangerous; it should therefore be avoided, especially when there are standard guidelines for management of the condition.
Conclusion
Up to now, there is no information about intra-tonsillar local phenol injection which occurred in our case to treat tonsillitis in literature. Therefore, intra-tonsillar, oral or parenteral phenol usage should be evaluated as a medical malpractice.
References
- Millington AJ, Phillips JS. Current trends in tonsillitis and tonsillectomy. Ann R Coll Surg Engl 2014; 96:586-589.
- Lau AS, Upile NS, Wilkie MD, et al. The rising rate of admissions for tonsillitis and neck space abscesses in England, 1991–2011. Ann R Coll Surg Engl 2014; 96:307-310.
- Bochner RE, Gangar M, Belamarich PF. A clinical approach to tonsillitis, tonsillar hypertrophy, and peritonsillar and retropharyngeal abscesses. Pediatr Review 2017; 38:81-92.
- Gereige R, Cunnill-De Sautu B. Throat infections. Peadiatr Review 2011; 32:459-469.
- Uzodimma CC, Dedeke FI, Nwadike V, et al. A study of group a streptococcal pharyngitis among 3–15-year-old children attending clinics for an acute sore throat. Nig J Cardiol 2017; 14:97-102.
- Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group a streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis 2012; 55:1279-1282.
- Baugh RF, Archer SM, Mitchell, RB, et al. Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg. 2011; 144:1-30.
- Chiappini E, Regoli M, Bonsignori F, et al. Analysis of different recommendations from international guidelines for the management of acute pharyngitis in adults and children. Clin Ther 2011; 33:48-58.
- Kavanagh KT, Beckford NS. Adenotonsillectomy in children: Indications and contraindications. South Med J 1988; 81:507-514.
- https://www.healthline.com/health/what-is-phenol
- https://en.wikipedia.org/wiki/Phenol
Author Info
Lawan Musa Tahir1*, Lokman Cam1*, Atilla Emiroglu2, Mehmet Sina3 and Senol Dane4
1Departments of Pediatrics, Faculty of Basic Medical Sciences, College of Health Sciences, Nile University of Nigeria, Abuja, Nigeria2Department of ENT, Faculty of Basic Medical Sciences, College of Health Sciences, Nile University of Nigeria, Abuja, Nigeria
3Department of Radiology of Nizamiye Hospital, Faculty of Basic Medical Sciences, College of Health Sciences, Nile University of Nigeria, Abuja, Nigeria
4Department of Physiology, Faculty of Basic Medical Sciences, College of Health Sciences, Nile University of Nigeria, Abuja, Nigeria
Citation: Lawan Musa Tahir, Lokman Cam, Atilla Emiroglu, Mehmet Sina, Senol Dane, Cerebral Infarction Following Intra-Tonsillar Injection of Phenol in a Child, J Res Med Dent Sci, 2020, 8(2): 39-41
Received: 13-Mar-2020 Accepted: 02-Apr-2020
