Research - (2022) Volume 10, Issue 12
Cervical epidural anesthesia for large goiter with tracheal deviation
*Correspondence: Ali M Hasan Altaiey, Department of Anesthesiologist, Alazizya General Hospital, Wasit Health Director, Iraq, Email:
Abstract
Background: Cervical epidural anesthesia is a regional anesthesia technique which has been used for upper limb surgery, upper thoracic wall surgery, carotid artery surgery and neck dissections. Anesthesia for thyroid surgery can be complicated due to the altered functional status of the thyroid or its large size. Objective: This prospective study was designed to assess the effectiveness and safety of cervical epidural anesthesia for thyroid surgery. Materials and methods: Cervical epidural anesthesia was attempted in 75 years old female patient with long past history of smoking. The epidural catheter was placed in the C7 – T1 vertebral interspace and 10 – 15 ml of 1% Lignocaine and 0.25 Bupivacaine with adrenaline was injected. Results: The technique of cervical epidural anesthesia was successfully used in our patient in whom it was attempted. Patient was maintained in a state of conscious – sedation and effective analgesia was obtained our patient. There were no significant complications especially those related to diaphragmatic function and cardiovascular stability. In contrast patients undergoing surgery under conventional general anesthesia had complications related to endotracheal intubation, cardiac arrhythmias and hypotension Conclusion: The technique of cervical epidural anesthesia should be considered in thyroid patients where difficult endotracheal intubation is anticipated and in those in whom alterations in thyroid functional state make them vulnerable to cardiovascular complications under conventional general anesthesia.
Keywords
Thyroid surgery, Large goiter, Tracheal deviation, Cervical epidural anesthesia
Introduction
Providing safe and effective anesthesia for thyroid surgery can sometimes become a problem for the anesthetists. This becomes especially relevant in large goiters which might compress or deviate the trachea. Endotracheal intubation is difficult in such cases and in large goiters can be hazardous. Also, the goiter might be associated with thyroid functional disorders. Patients with both hypo and hyperthyroidism are prone to cardiac rhythm disorders which might get aggravated under the influence of general anesthetic agents. Regional anesthetic techniques are safer than general anesthesia (GA) in high-risk patients where endotracheal intubation is difficult or cardiac arrhythmias are anticipated. For thyroid surgery regional anesthesia is not a conventionally described option. Cervical epidural anesthesia (CEA) has been used for shoulder, upper extremity, and thoracic wall surgery with good results. Here we describe our experiences of using this technique for thyroid surgery.
Materials and Methods
The technique of cervical epidural anesthesia was used in one patient who underwent thyroid surgery.
Selection criteria
Cervical epidural anesthesia technique used in one case who underwent thyroid surgery for patient with 73 years old 68 kg.
Technique of CEA
The patient was placed in a sitting position with flexion at the neck and forehead supported on a table. Skin at the nape of neck was disinfected with cetrimide and spirit. The spine of the C7 vertebra was identified as the 1st prominent spine while palpating in the midline from the occiput downwards. The space between the C7 and T1 vertebral spines was infiltrated with 2% Lignocaine. An 18-gauge Tuohy needle was inserted in the C7 – T1 interspace perpendicularly so that the needle would be parallel to the vertebral spine. The bevel of the needle was kept facing upwards. The needle was advanced carefully to get a feel of piercing the ligamentum flavum. It should be kept in mind that the resistance offered by the ligament in the neck is lesser than in the lumbar area. Epidural placement of the needle tip was ascertained by loss of resistance or the hanging drop technique. An epidural catheter was guided through the Tuohy needle and advanced 3 – 4 cm in to the epidural space followed by removal of the needle. After reconfirming by aspiration that subarachnoid entry had not occurred 10 – 15 ml of 1% Lignocaine and 0.25 Bupivacaine with 1: 200,000 Adrenaline was injected through the catheter. The patient was placed in supine position and after a 35 minutes observation of the pulse rate, respiratory effort and blood pressure, ‘thyroid position’ with extension of the neck was permitted (Figures 1 and Figure 2).
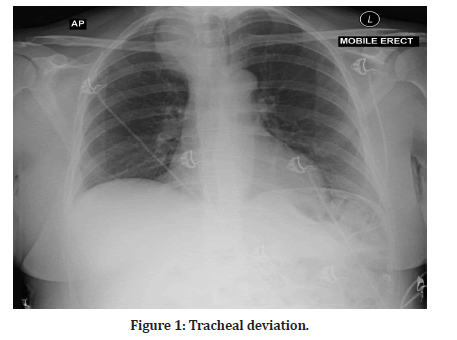
Figure 1: Tracheal deviation.
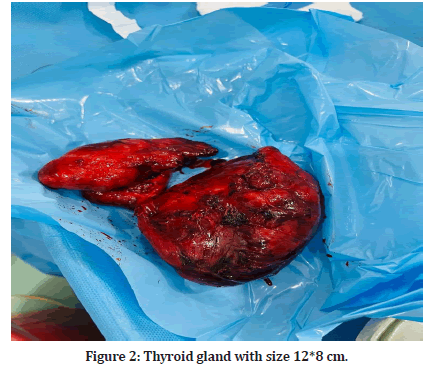
Figure 2: Thyroid gland with size 12*8 cm.
Results
Our patient in whom it was attempted CEA was successful. The patient was comfortably maintained sedated but awake during the procedure with no untoward effect. Monitoring of the pulse, respiratory effort, BP and peripheral oxygen saturation was carried out and patient maintained these parameters without additional support. The surgery lasted for more than 90 minutes, additional injection of 10 ml of our mixture was required through the epidural catheter to maintain analgesic effect.
Discussion
Providing safe anesthesia for thyroid surgery can be a difficult task for two reasons (1) Possibility of tracheal deviation or compression because of enlarged thyroid, (2) Possibility of hemodynamic disturbances including arrhythmias and hypotension related to the functional status of the thyroid. Conventional general anesthesia with endotracheal intubation may not always be possible and even hazardous in certain situations. Endotracheal intubation can become a traumatic procedure precipitating laryngeal oedema occasionally. Anesthetic gases, Propofol and muscle relaxants can all become arrhythmogenic in the presence of covert or even occult hypo or hyperthyroidism states. As in other situations where general anesthesia becomes a high-risk proposition, regional anesthesia is considered the safer alternative. But for thyroid surgery, regional anesthetic techniques have neither been adequately described nor practiced widely. Cervical epidural anesthesia aims to anesthetize the skin in front of the neck where the incision would be placed. The front of the neck is supplied by 2nd and 3rd cervical rami which form the transverse cutaneous nerve of the neck. The lower part of the neck and the part lateral to sternocleidomastoid muscle is supplied by supraclavicular nerves which arise from the 3rd and 4th cervical ventral rami. For delivering CEA, we introduced the epidural catheter in the C7 –T1 vertebra interspace and guided it upwards by keeping the bevel of the Tuohy needle facing cranially. By using the technique described above, the upper level of sensory block obtained was at C2 level and the lower level varied from T5 to T10. Cervical epidural anesthesia has been used mainly for hand, upper limb, shoulder and upper thoracic wall surgery including mastectomy. It has also been used for carotid artery surgery [1], parathyroid surgery [2], neck dissection for head and neck cancers [3] and for the treatment of complex regional pain syndromes of the upper limb [4]. Adequate surgical anesthesia with a high degree of patient acceptance has been reported by all authors. The main reasons why CEA has not come into wide clinical usage are fears of its potential complications. These include its effects on respiratory function especially phrenic nerve controlled diaphragmatic movements and cardio-vascular stability. Despite the concern over pulmonary dysfunction with CEA, it is rarely of clinical significance even in debilitated patient (1). Phrenic nerve is the sole motor supply to the diaphragm and also contains wide spread sensory fibers. It arises chiefly from the fourth cervical ramus but also contains contributions from the 3rd and 5th. Being mainly a motor nerve, it is exceptionally resistant to the effects of Lignocaine when it is used at a concentration of 1% and deployed in the epidural space. Stevens, et al. [5] found a measurable reduction in bedside pulmonary function test after CEA. They found that the forced expiratory volume (FEV) and forced vital capacity (FVC) decreased by 12 – 16% after using 300 mg of Lignocaine but these changes were not clinically significant. They concluded that the motor block of phrenic nerve is incomplete after CEA. Capdevila et al 6 using ultrasonography found that the diaphragmatic excursion decreased from 5.6 to 4.4. cm after CEA. They found that although CEA provided painless rehabilitation, it affected diaphragmatic function and respiratory drive. We found that CEA did not have any effect on respiratory functions. None of our patients had changes in breathing pattern or fall in peripheral arterial oxygen saturation on pulse oximetry. Acute paralysis of the diaphragm should produce violent contractions of the abdominal muscles as a compensatory mechanism. This was not found in any of our patient. Also, none the patient not developed pulmonary atelectasis post operatively. The other major concern with CEA has been its effects on heart rate and hemodynamic stability. CEA can result in cardiac sympathectomy which can depress phasic and tonic dynamic modulation of the cardiac cycle [6,7]. This can lead to a lack of increase in heart rate and a decrease in mean arterial pressure. CEA has also been found to attenuate the alcuronium induced tachycardia as a result of cardiac sympathetic denervation [8,9]. The cardiovascular stimulatory effects of Ketamine are also suppressed partially by CEA9. The most frequently reported side effects of CEA are hypotension and bradycardia. In our experience on our patient there is no cardiovascular side effect. the patient not required ionotropic support or an anti-arrhythmia medication. These effects were specially marked in patients with difficult endotracheal intubation or hyperthyroid state. Thus, the cardiac sympathetic denervation effect of CEA may be especially useful in patients with hyperthyroidism. Our patient operated under CEA was maintained in a state of conscious – sedation. This allows continuous verbal communication with the patient and early detection of recurrent laryngeal nerve injury which can occur during thyroid surgery.
Conclusion
Review of literature and our own experience shows that CEA is a safe and reliable technique. It can be easily learnt by anesthetists who are already familiar with lumbar epidural anesthesia. The complication rates are low and easily manageable. The risks of diaphragmatic paralysis and hemodynamic stability are present but rarely of clinical significance. We recommend this technique as the procedure of choice for thyroid surgery with large goiter and obvious tracheal deviation.
References
- Bonnet F, Derosier JP, Pluskwa F, et al. Cervical epidural anaesthesia for carotid artery surgery. Canadian J Anaesthesiol 1990; 37:353–358.
- Michalek P, David I, Adamec M, et al. Cervical epidural anaesthesia for combined neck and upper extremity procedure: A pilot study. Anaesth Analg 2004; 99:1833–1836.
- Wittich DJ, Berny JJ, Davis RK. Cervical epidural anaesthesia for head and neck surgery. Laryngoscope 1984; 94:615–619.
- Buchheit T, Crews JC. Lateral cervical epidural catheter placement for continuous unilateral upper extremity analgesia and sympathetic block. Regional Anaesthesia Pain Med 2000; 25:313–3177.
- Stevens RA, Frey K, Sheikh T, et al. Time course of the effects of cervical epidural anaesthesia on pulmonary function. Regional Anaesthesia Pain Med 1998; 23:20-24.
- Capdevila X, Biboulet P, Rubenovitch J, et al. The effects of cervical epidural anaesthesia with bupivacaine on pulmonary function in conscious patients. Anaesth Analg 1998; 86:1033–1038.
- Tanaka M, Goyagi T, Kimura T, et al. The effects of cervical and lumbar epidural anaesthesia on heart rate variability and spontaneous sequence barorefl ex sensitivity. Anaesth Analg 2004; 99:924–929.
- Omete K, Iwasaki H, Namiki A. Cervicothoracic epidural anaesthesia blunts pancuronium induced increase in heart rate in humans. Acta Anaesthesiol Scand 1993; 37:415–418.
- Mayumi T, Dohi S, Takahashi T. Cardiovascular effects of ketmine in humans with cervical or lumbar epidural blockade. Anaesthesiology 1985; 62:39–43.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Department of Anesthesiologist, Alazizya General Hospital, Wasit Health Director, IraqCitation: Ali M Hasan Altaiey, Cervical Epidural Anesthesia for Large Goiter with Tracheal Deviation, J Res Med Dent Sci, 2022, 10 (12): 108-110.
Received: 22-Nov-2022, Manuscript No. jrmds-22-78013; , Pre QC No. jrmds-22-78013(PQ); Editor assigned: 24-Nov-2022, Pre QC No. jrmds-22-78013(PQ); Reviewed: 08-Dec-2022, QC No. jrmds-22-78013(Q); Revised: 12-Dec-2022, Manuscript No. jrmds-22-78013(R); Published: 19-Dec-2022
