Research - (2021) Volume 9, Issue 6
Clinical Evaluation of Peripheral Vascular Disease in Diabetic Foot Ulcer
T Rathnaganpathi and T Raghupathy*
*Correspondence: T Raghupathy, Department of General Surgery, Sree Balaji Medical College & Hospital Affiliated ed to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email:
Abstract
To analyse the clinical presentation, predisposing factors, co-morbidities in patients with diabetic foot ulcer. The study is a descriptive study of Peripheral vascular disease. This study involves a single group of patients with Diabetic foot admitted in SBMCH between the periods of December 2017–July 2019. Smoking of 31%, Hypertension was found in 32% patients, Coronary arterial disease of 23 %, Dyslipidemia of 32 % are the major co- morbidies in this study which peripheral arterial disease is associated in diabetic foot ulcer. It is noted that the prevalence of Peripheral Arterial Disease is 29% in our study. A strong suspicion of Peripheral Arterial Diseases should be discussed with patients with high risk factors associated with PAD, such as male, age >40 years, foot ulcer, duration of the disease >6yrs, smoking, bare foot walking. Our data highlights the need for more work to recognize and target this high risk diabetic foot ulcer population.
Keywords
Dyslipidemia, Hypertension, Coronary arterial disease, Diabetic foot ulcer.
Introduction
Diabetes is a "Global epidemic” with approximately 500 million people worldwide suffering from diabetes, around 1 in 11 people44. According to the International Diabetes Federation (IDF), after China 121 million, India has an estimated 74 million diabetic patients compared to any other country in the world [1-3]. During their lifetime, most diabetics develop foot ulcers that have a significant impact on the quality of life of the patient. The diabetic foot is defined as any foot disease resulting directly from the diabetic condition or its long-term complications [4,5]. One of the most common complications we see in the diabetic population is foot complications, which is a major cause of hospitalization. The WHO identifies a diabetic patient's foot with the high risk of infection, ulceration and loss of deep tissue associated with neurological abnormalities, peripheral vascular disease and/or metabolic complications [6].
One of the major etiological factors in diabetic foot is peripheral artery disease (PAD) which is more prevalent in diabetes patients and about half of diabetic foot ulcer patients have coexisting peripheral artery disease. Prevalence of diabetic foot ulcer ranges from 4 to 10% in hospitalized patients. The Global Lower Extremity Amputation Study Group estimated that between 14 and 24% of patients with DFU may need amputation48. Recent studies suggest that the risk of developing foot ulcer in diabetic patients is approximately 25% across their lives [7,8]. Risk factors for DFU include: male sex, diabetes over 10 years, peripheral neuropathy, irregular foot structure (bone alterations, calluses, thickening of nails), peripheral arterial disease, and smoking, history of ulcers or amputation, and impaired glycemic control49. Peripheral artery disease is defined as clinical disorder where there is stenosis or occlusion of lower limbs arteries. Atherosclerosis is the main cause of peripheral artery disease in people over 4048. Diabetes is associated with a two to fourfold increase in PAD incidence compared to non-diabetic individuals. Peripheral artery disease is a major indicator of foot ulceration in patients with diabetes [9,10]. The physician who treats a patient with diabetes or foot ulcer should therefore also determine the vascular state of the lower limbs and explicitly check for symptoms of ischemia, because up to 50% of these patients have Peripheral artery disease (PAD) [11,12]. Nevertheless, the detection of PAD and its severity assessment in diabetic patients with foot disease is a clinical challenge due to altered clinical presentation of PAD and limitations of diagnostic procedures. In addition, the healing of the wound in these patients is influenced not only by the presence of PAD, but also by factors such as infection and co- morbidity [13].
Materials and Methods
The study is a descriptive study of Peripheral vascular disease.
This study involves a single group of patients with Diabetic foot admitted in SBMCH between the periods of DECEMBER 2017–JULY 2019.
Clinical palpation of lower extremity pulses.
Hand Doppler assessment of arterial flow in pedal vessels.
Ankle-brachial-pressure index (ABPI).
Inclusion criteria
All cases of Diabetic foot admitted in SBMCH between the period from December 2017–February 2019.
Exclusion criteria
All proven case of peripheral vascular disease. An analysis of 100 cases of diabetic foot ulcers was done. These cases were admitted in General surgical department in both male and female wards in Sree Balaji Medical College and Hospital, Chennai during the period of December 2017–February 2019.
Results
In this present study females were affected more than males. There is slightly higher incidence of diabetes mellitus in females and male persons are more prone for diabetic foot ulcers due to trauma, bare foot walking, vascular disease and smoking etc.
In our study, out of 100 cases females constituted 54 and males 46 (Table 1). In Table 2 association on diabetic foot ulcer is more common in the age group of 51-60 years
| Gender | Frequency | Percent |
|---|---|---|
| Female | 54 | 54 |
| Male | 46 | 46 |
| Total | 100 | 100 |
Table 1: Gender frequency.
| Frequency | Percent | |
|---|---|---|
| 31 to 40 years | 2 | 2 |
| 41 to 50 years | 23 | 23 |
| 51 to 60 years | 40 | 40 |
| 61 to 70 years | 22 | 22 |
| 71 to 80 years | 10 | 10 |
| 81 to 90 years | 3 | 3 |
| Total | 100 | 100 |
Table 2: Association with age group.
A significant number of patients were diagnosed to have diabetes. Most of the patients had duration of up to 6-10 years. Our study has no correlation between duration and the prognosis of disease (Table 3). 32 percent of the diabetic foot ulcer has associated with hypertension (Figure 1). 32 percent of the diabetic foot ulcer has associated with lipids (Table 4).
| Frequency | Percent | |
|---|---|---|
| 1 to 5 years | 16 | 16 |
| 6 to 10 years | 29 | 29 |
| 11 to 15 years | 21 | 21 |
| 16 to 20 years | 15 | 15 |
| 21 to 25 years | 4 | 4 |
| 26 to 30 years | 11 | 11 |
| 31 to 35 years | 3 | 3 |
| 36 to 40 years | 1 | 1 |
| Total | 100 | 100 |
Table 3: Duration of diabetes.
| Frequency | Percent | |
|---|---|---|
| No | 68 | 68 |
| Yes | 32 | 32 |
| Total | 100 | 100 |
Table 4: Association with dyslipidemia.
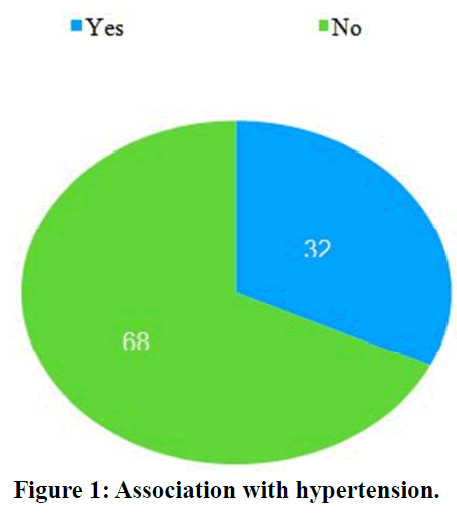
Figure 1. Association with hypertension.
23 percent of the diabetic foot ulcer patients had associated coronary artery disease.
The association was stronger with female sex 63% which indicates their inherent susceptibility towards coronary disease (Table 5). 4 percent of the diabetic foot ulcer has associated with Transient ischemic attack (Figure 2).
| Frequency | Percent | |
|---|---|---|
| No | 77 | 77 |
| Yes | 23 | 23 |
| Total | 100 | 100 |
Table 5: Association with coronary arterial disease.
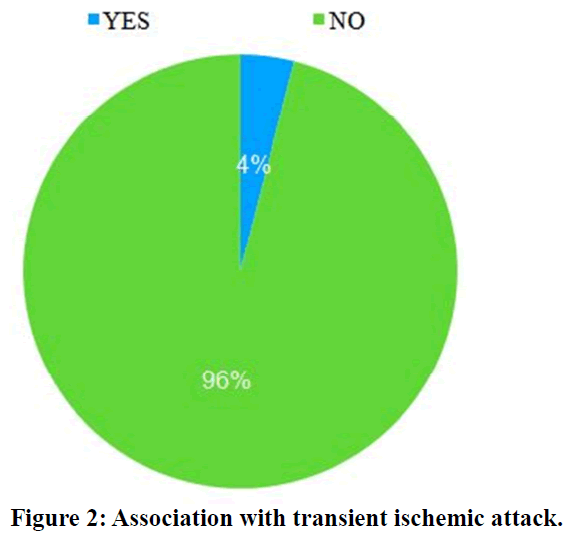
Figure 2. Association with transient ischemic attack.
31 percent of the diabetic foot ulcer has associated with smoking (Table 6). 12 percent of the diabetic foot ulcer has no flow or absent flow. 18 percent of the diabetic foot ulcer patients have decreased or feeble flow and 70 percent had normal or regular flow (Table 7).
| Frequency | Percent | |
|---|---|---|
| No | 69 | 69 |
| Yes | 31 | 31 |
| Total | 100 | 100 |
Table 6: Association with smoking.
| Frequency | Percent | |
|---|---|---|
| Present | 70 | 70 |
| Feeble | 18 | 18 |
| Absent | 12 | 12 |
| Total | 100 | 100 |
Table 7: Association with pulse.
In this above table ankle brachial pressure index measured in the diabetic foot ulcer patient 29 % of the patient has ischemic changes in which 12 % of the cases severe ischemia and mild to moderate ischemic changes around 17% (Figure 3).
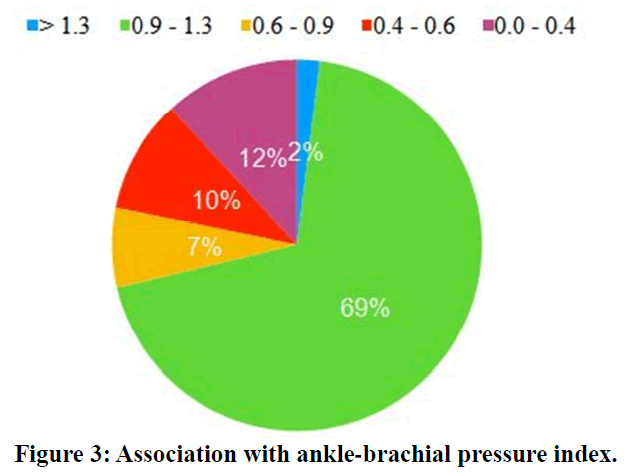
Figure 3. Association with ankle-brachial pressure index.
49 percent of the diabetic foot ulcer has brittle or abnormal nail. 51 percent of the diabetic foot ulcer patients have normal nails (Table 8). 12 percent of the diabetic foot ulcer presented with deformity.
| Frequency | Percent | |
|---|---|---|
| Brittle | 49 | 49 |
| Normal | 51 | 51 |
| Total | 100 | 100 |
Table 8: Association with nails.
88 percent of the diabetic foot ulcer patients have no deformity (Figure 4). 12 percent of the diabetic foot ulcer has no flow or absent flow.
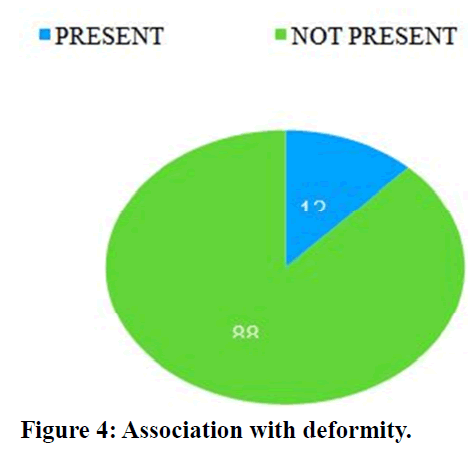
Figure 4. Association with deformity.
17 percent of the diabetic foot ulcer patients has mono phasic flow and 71 percent had bi-phasic flow (Figure 5). Figure 6 and Figure 7 shows diabetic foot with various stages.
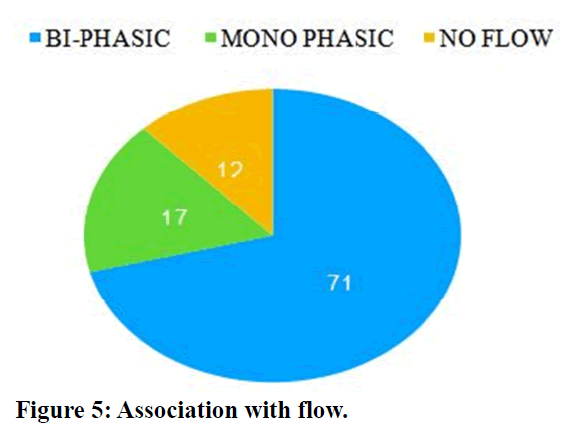
Figure 5. Association with flow.
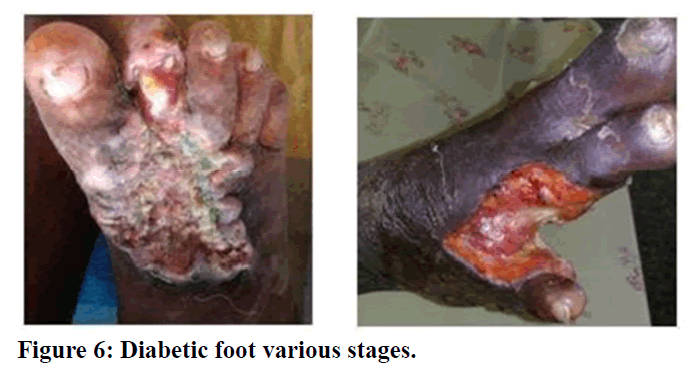
Figure 6. Diabetic foot various stages.
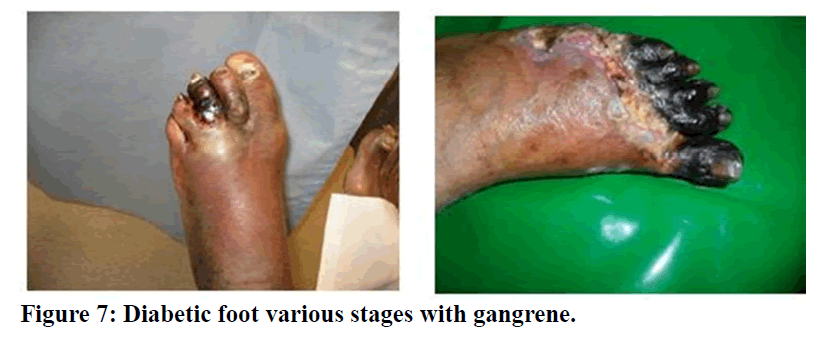
Figure 7. Diabetic foot various stages with gangrene.
Discussion
Out of 100 patients, 31 had a history of smoking. Out of 31 patients 15 (32.6%) have a strong association between smoking and peripheral vascular disease. In a study Khan Y et al in which the studies report of 69.5% patients have smoking as strong association with peripheral vascular disease50. Smoking with diabetes foot ulcer have a strong association with peripheral vascular disease. Smoking of 31%, Hypertension was found in 32% patients, Coronary arterial disease of 23 %, Dyslipidemia of 32 % are the major co-morbidies in this study which peripheral arterial disease is associated in diabetic foot ulcer. The most common pathological shift associated with Peripheral Arterial Disease was atherosclerosis, which caused an artery to harden directly caused by an atheromatous plaque. Nonetheless, a number of causative factors for atherosclerosis have been identified [14,15].
Hyperlipidemia/Hypercholesterolemia, obesity, diabetes mellitus and exposure to infection, cigarette smoking were all significant and independent risk factors studies found a stronger link between tobacco abuse and Peripheral Arterial Disease. Heavy smokers have higher risk of Peripheral Arterial Disease in ex- smokers than in non-smokers51-53. In our study hyperlipidemia/ hypercholesterolemia independent risk factor which is about 37.5% in females and 62.5% in males. Among hypertensive females’ risk was 59.37% and in males were 40% [16]. In association with coronary arterial disease risk factor were around 45% in females and 56.5%in males.In association with diabetic in female hypertension followed by hyperlipdemia have a strong association towards peripheral arterial disease. Among smoking, the amputation and mortality rates are also higher. In our study we found that patients out of 15 were 32% of the prevalence of smokers [17]. There is a need for a systematic assessment of peripheral vascular disease due to atherosclerosis in all diabetic patients, particularly patients with diabetic foot infections.
Previous studies aimed at researching the prevalence of Peripheral Arterial Disease, regardless of foot ulcer, in the diabetic population.
This research aimed at evaluating the burden of Peripheral Arterial Disease in diabetic patients particularly diabetic foot ulcer (DFU) and the prevalence is 29%.
Mohan et al reported 3.9 percent prevalence of Peripheral Arterial Disease in diabetics in South India which has been doubled in 10 years [18]. They compared their data with Western research, where the frequency ranged from 22% to 45%. Another South India study reported a lower prevalence of Peripheral Arterial Disease among Indians 13 %. A similar study reported a prevalence of 42 % from Greece [19-22].
In a study based tertiary setting in Eastern India, Peripheral Arterial Disease (ABPI<0.9) was diagnosed in 141 (34.4%) patients54. Peripheral Arterial Disease occurred in 46 percent of foot ulceration subjects compared with 32.7 percent of non-foot ulceration subjects [23-27]. In our study Peripheral Arterial Disease (ABPI <0.9) was around 29%. Mohan et al concluded that, with advancing age, the prevalence of Peripheral Arterial Disease in diabetics increased from 15% at 10 years to 45% at 20 years from diagnosis of diabetes. In a study of the Central Indian population, the duration of diabetes<10 years was 30% correlated with Peripheral Arterial Disease, while the length of the interaction was > 10yrs doubled to 60% and tripled in 20 years [28].
Conclusion
In South Indian, Peripheral Arterial Disease prevalence in diabetic foot ulcer is high. Peripheral Arterial Disease incidence and various factors coexisting with Diabetic foot ulcer and Peripheral Arterial Disease are examined in the present study. Risk factors for peripheral arterial disease are growing age and longer duration of diabetes. High prevalence increases the risk of amputation of diabetic foot ulcer. It is noted that the prevalence of Peripheral Arterial Disease is 29% in our study. A strong suspicion of Peripheral Arterial Diseases should be discussed with patients with high risk factors associated with PAD, such as male, age >40 years, foot ulcer, duration of the disease >6yrs, smoking, bare foot walking. Using hand held Doppler can accurately and cost effectively assists in early diagnosis. In addition, a triple diagnosis checklist including distal pulse charting, ABPI and Doppler analysis should be observed to diagnose a Peripheral Arterial Disease correctly as soon as possible. Our data highlights the need for more work to recognize and target this high risk diabetic foot ulcer population.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledegements
The encouragement and support from Bharath University, Chennai, is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Wagner FW. Management of the diabetic-neurotrophic foot. Part II. A classification and treatment program for diabetic, neuropathic, and dysvascular foot problems. Instr Course Lect 1979; 28:143-65.
- Aksoy DY, Gürlek A, Cetinkaya Y, et al. Change in the amputation profile in diabetic foot in a tertiary reference center: Efficacy of team working. Exp Clin Endocrinol Diabetes 2004; 112:526-30.
- Bouter KP, Storm AJ, Uitslager R, et al. The diabetic foot in Dutch hospitals: Epidemiological features and clinical outcome. Eur J Med 1993; 2:215-8.
- Rao N, Lipsky BA. Optimising antimicrobial therapy in diabetic foot infections. Drugs 2007; 67:195-214.
- Leymarie F, Richard JL, Malgrange D. Factors associated with diabetic patients at high risk for foot ulceration. Diabetes Metabol 2005; 31:603-5.
- Tentoiours NE. Prevalence of MRSA in infected and uninfected Diabetic foot and ulcers. Clin Microbiol Infections 2004; 186-9.
- Rauner MS, Heidenberger K, Pesendorfer EM. Model-based evaluation of diabetic foot prevention strategies in Austria. Health care Management Sci 2005; 8:253-65.
- Malmstedt J. Diabetes and peripheral arterial disease. Mol Med Surg 2012.
- Schaper NC, Apelqvist J, Bakker K. The international consensus and practical guidelines on the management and prevention of the diabetic foot. Current Diabetes Reports 2003; 3:475-9.
- Benotmane A, Faraoun K, Mohammedi F, et al. Treatment of diabetic foot lesions in hospital: Results of 2 successive five-year periods, 1989-1993 and 1994-1998. Diabetes Metabol 2004; 30:245-50.
- Milne AC, Avenell A, Potter J. Meta-analysis: protein and energy supplementation in older people. Annals Internal Med 2006; 144:37-48.
- Birrer RB, Dellacorte MP, Grisafi PJ. Prevention and care of diabetic foot ulcers. Am Family Physician 1996; 53:601-11.
- Boulton AJM. The diabetic foot. In, Oletsky JM, Diabetes mellitus management and complications churchill Livingstone, New York 2nd Edn. 2000; 225-75.
- Day MR, Harkless LB. Factors associated with pedal ulceration in patients with diabetes mellitus. J Am Podiatr Med Assoc 1997; 87:365-9.
- Delbridge L, Ctercteko G, Fowler C, et al. The aetiology of diabetic neuropathic ulceration of the foot. Br J Surg 1985; 72:1-6.
- LoGerfo FW, Coffman JD. Vascular and microvascular disease of the foot in diabetes: Implications for foot care. New Eng J Med 1984; 311:1615-9.
- Menzoian JO, LaMorte WW, Paniszyn CC, et al. Symptomatology and anatomic patterns of peripheral vascular disease: Differing impact of smoking and diabetes. Annals Vascular Surg 1989; 3:224-8.
- Holman RC, Herron CA, Sinnock P. Epidemiologic characteristics of mortality from diabetes with acidosis or coma, United States, 1970-78. Am J Public Health 1983; 73:1169-73.
- Tyagi A, Lavanya S, Prasad GH. A clinical study of peripheral vascular disease due to atherosclerosis in diabetic foot infections. Int Surg J 2018; 5:931-6.
- Thulasikumar G, Vijayasarathy S. Assessment of prevalence and risk factors of peripheral arterial disease in diabetic foot ulcer. Int J Surg Med 2017; 3:156-166.
- Nagateja, Lingaraju N. Prevalence and risk factors of peripheral vascular disease in diabetic foot lesions. Int J Sci Stud 2016; 3:32-36.
- Lipsky BA, Weigelt JA, Sun X, et al. Developing and validating a risk score for lower-extremity amputation in patients hospitalized for a diabetic foot infection. Diabetes Care 2011; 34:1695-700.
- Jeffcoate WJ, Chipchase SY, Ince P, et al. Assessing the outcome of the management of diabetic foot ulcers using ulcer- related and person-related measures. Diabetes Care 2006; 29:1784-7.
- Greenland P, Knoll MD, Stamler J, et al. Major risk factors as antecedents of fatal and nonfatal coronary heart disease events. JAMA 2003; 290:891-7.
- Murrie JA, Callam MJ. Femoral and distal arteries. In: Morris PJ, Malt RE. Oxford Textbook of Surgery. Oxford, UK: Oxford University Press; 1995; 7.
- Second European Consensus Document on chronic critical leg ischemia. Circulation 1991; 84:IV1-26.
- Blair JF, Bandyk DF. Real-time color doppler in arterial imaging. In: Yao JS, Pearce WH. Technologies in vascular surgery. Philadelphia, Pennsylvania: Saunders 1991; 129-49.
- Premalatha G, Shanthirani S, Deepa R, et al. Prevalence and risk factors of peripheral vascular disease in a selected South Indian population: The Chennai urban population study. Diabetes Care 2000; 23:1295-300.
Author Info
T Rathnaganpathi and T Raghupathy*
Department of General Surgery, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: T Rathnaganpathi, T Raghupathy, Clinical Evaluation of Peripheral Vascular Disease in Diabetic Foot Ulcer, J Res Med Dent Sci, 2021, 9(6): 312-318.
Received: 01-Apr-2021 Accepted: 23-Jun-2021
