Research - (2021) Volume 9, Issue 6
Clinocopathological Study on Gastro Endoscopic Biopsies in Patients with Special Reference to Helicobacter Pylori
*Correspondence: Parijatham BO, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
Chronic gastritis is the common problem worldwide. The common etiologic agents implicated were smoking, non-steroidal anti-inflammatory drugs (NSAIDs), spicy food and an influence of personality status. But now it has been proved that in addition to these, Helicobacter pylori (H. pylori), a bacterial infective agent, is the major and most common cause. H. pylori gastritis (HPG) is caused by infection of the antral mucosa with H. pylori. Most patients with HPG are asymptomatic. In many cases the antrum appears normal to the endoscopist. Lymphoid follicles with germinal centers are characteristic of an infection with H. pylori. The organisms can be seen in routine hematoxylin and eosin-stained tissue when numerous organisms are present. Special stains are useful when few organisms are present. Stains that may be used to highlight the organisms are Giemsa stain, Warthin¬ Starry silver stain, Gram stain, and immunocytochemical stains. In the present study 3 stains were compared for their efficacy – H&E, Giemsa and Warthin¬ Starry silver stain. It can be concluded from the present study that, Warthin-Starry silver stain was found to be the best stain for the detection of low density H. pylori infection. Giemsa stain can be used for detection of H. pylori infection of moderate to high density. Moreover, presence of neutrophils & lymphoid follicles might be taken as an indirect evidence for H. pylori infection.
Keywords
H&E, Chronic gastritis, Warthin-starry silver stain, Giemsa, H. pylori, Antrum
Introduction
Chronic gastritis is the common problem worldwide. Previously many etiologic agents have been implicated in the causation of this disease such as smoking [1], nonsteroidal anti- inflammatory drugs (NSAIDs) [2], spicy food and an influence of personality status [3]. But now it has been proved that in addition to these Helicobacter pylori, a bacterial infective agent is the most common cause [4]. H. pylori gastritis is caused by infection of the antral mucosa with H. pylori [5]. The gastric antrum extends from its indistinct border with the body to the junction of the pylorus with the duodenum. Most patients with HPG are asymptomatic [6]. In most cases the antrum appears normal to the endoscopist; some patients with active disease in the antrum may demonstrate red streaks. Radiographic differences between antral gastritis caused by H. pylori and not caused by H. pylori have been described; thickened gastric folds, especially in a polypoid configuration, and enlarged areae gastricae favour H. pylori as the cause, whereas antral erosions favor causes other than H. pylori [7].
Histologically, a diffuse, chronic inflammatory infiltrate which includes numerous lymphocytes and plasma cells expands the lamina propria and epithelium [6]. The presence of acute inflammatory cells along with chronic inflammation is best designated an active gastritis and not acute gastritis. Additional microscopic changes include injury to the surface and foveolar epithelium with loss of apical mucin and reactive nuclear changes and erosions [8].
Lymphoid follicles with germinal centers are characteristic of an infection with H. pylori [9]. H. pylori organisms lie in the superficial mucous layer along the mucosal surface and within the gastric pits. The organisms can be seen in routine hematoxylin and eosin-stained tissue when numerous organisms are present. Special stains are useful when few organisms are present. Stains that may be used to highlight the organisms are Giemsa stain, Warthin Starry silver stain, Gram stain, and immunocytochemical stains [10]. Helicobacter heilmannii spiral bacteria are a less frequent cause of active gastritis [11]. The organisms originally known as Gastro pirillumhominis are longer than H. pylori and have multiple spirals [11]. A topographic study of H. pylori density and distribution and the comparison of biopsy sites for the histopathological diagnosis of H. pylori conclude that two antral biopsy specimens, one from the lesser and one from the greater curvature, have close to 100% sensitivity for detecting H. pylori infection [12]. Biopsy specimens from the corpus increase the diagnostic yield if extensive intestinal metaplasia is present in the antrum [13].
In the present study, 3 stains (H&E, Giemsa and Warthin Starry silver stain) were compared for their efficacy in detecting H. pylori in biopsies.
Materials and Methods
Processing of gastric biopsy
H&E stained sections of all the cases were reviewed and fresh sections were taken from the blocks for staining by Giemsa, and WSS stains. Morphological changes in all cases were studied with special reference to atrophy, dysplasia, metaplasia, neutrophilic infiltration, lymphoid follicle formation, plasma cell infiltration, & malignant changes. All endoscopic gastric mucosal biopsies taken from different sites were brought in 10% buffered formalin. After overnight fixation in formalin, processing was done manually followed by paraffin embedding and section cutting in rotary microtome. Serial sections of 5μm thickness were made & stained with Giemsa WSS stain.
Staining procedures haematoxylin and eosin
Section: Paraffin procedure
• Section brought down to water.
• Stained in Haematoxylin -10min.
• Washed in water -5min.
• Differentiated in 1% acid alcohol -5 to 10 sec.
• Washed in water.
• Blueing done with lithium carbonate for 5 mins.
• Washed in running water.
• Counter stained in 1% eosin -30sec.
• Blot dried.
• Dehydrated, cleared and mounted in DPX.
Results: Nucleus stained blue colour.
Cytoplasm and connective tissue tained pink colour H. pylori-blueish rods.
Giemsa stain procedure
• Sections brought down to water.
• Stained with Giemsa stain -5min.
• Slides blotted.
• Cleared in xylene.
• Mounted in DPX.
Results: H. pylori were stained dark blue colour Background was stained pink to pale blue colour.
Warthin-starry silver stain
Section: Paraffin
Results: H. pylori stained black coloured Background was stained yellow.
Developer solution
• To 0.3g Hydroquinone 10 ml buffer (pH 3.6) added.
• To 1ml of this solution 15ml of gelatin solution added.
• Mixed and kept at 40°C.
• 3 ml of 2% Silver Nitrate solution was taken in buffer (pH 3.6) and kept at 55°C.
• The solutions are mixed immediately before use.
Methods
Chronic Gastritis was classified as per updated Sydney System of Classification of Gastritis. Accordingly etiological parameters (H. pylori, (or) atrophic (or) alcoholic) and morphological parameters (neutrophilic activity (or) lymphoid follicle & hyperplasia (or) atrophy (or) intestinal metaplasia) and finally topographical parameters (antrum (or) corpus (or) both) were included in the final report respectively.
Results
A total of hundred cases of endoscopic gastric mucosal biopsies done for various indications were studied. The mean age of the patients was 50 yrs. Sex ratio in our study was M: F = 1.2: 1.
Clinical profile
Thirty five patients had symptoms of dyspepsia alone and thirty one patients had epigastric pain along with dyspepsia. Twelve patients had complaints of nausea and vomiting on and off along with epigastric pain. Twenty two patients had history of weight loss along with dyspepsia and epigastric pain. Dyspepsia was the most common feature for which gastric biopsies were taken. Duration of symptoms ranging from six to twelve months.
Site of biopsy
Sixty three were antral biopsy specimens; thirty one biopsies from corpus and six from both antrum and corpus were taken (Table 1). Sixty three cases of antral biopsy specimen showed chronic gastritis in fifty eight cases, malignancy in four cases and one polyp. Thirty two out of fifty eight antral gastritis were H. pylori gastritis. So, the most common cause for antral gastritis were due to H. pylori infection. Thirty one biopsies from corpus showed chronic gastritis in twelve cases, malignancy in twelve cases and three polyps. Eight out of twelve chronic gastritis in the corpus were H. pylori gastritis. Six biopsies were taken from both antrum and corpus. chronic gastritis were seen in two case, malignancy in four cases. Sixty percent malignancy (12 out of 20 malignant cases) was seen in the corpus and twenty percent (4 out of 20 malignant cases) from antral biopsy and twenty percent (4 out of 20 cases) from both areas. Whereas eighty percent (58 out of 72 chronic gastritis)of chronic gastritis were seen in the antrum and sixteen percent(12 out of 72 chronic gastritis) in the corpus.
| Site | Normal | Polyp | Malignancy (per total malignancy) | Chronic gastritis (per totalgastritis) | Total |
|---|---|---|---|---|---|
| Antrum | - | 1 | 4 (20%) | 58 (80%) | 63 |
| Corpus | 4 | 3 | 12 (60%) | 12 (16%) | 31 |
| Both | - | - | 4 (20%) | 2 (2.7%) | 6 |
| Total | 4 | 4 | 20 | 72 | 100 |
Table 1: Site of biopsy and distribution of lesions.
Distribution of lesion and site in percentage
Ninety two percent of antral biopsies showed chronic gastritis, six percent malignancy and 1 percent showed polyp. Thirty nine biopsies from corpus showed chronic gastritis, thirteen showed malignancy nine percent polyp and twelve percent normal. Sixty six biopsies containing both antral and corporal mucosa showed chronic gastritis, thirty three percent showed malignancy. Out of 72 chronic gastritis, 42 cases were H. pylori gastritis. Of this 32 H .pylori gastritis (76%) were antral gastritis and 8 cases (l4%) from corpus. 2 cases from both corpus and antrum (Table 2).
| Site | H. pylori gastritis |
|---|---|
| Antrum | 32 |
| Corpus | 8 |
| Antrum and Corpus | 2 |
| Total | 42 |
Table 2: No. of H. pylori gastritis and its site.
Histopathological findings
Chronic gastritis and associated lesions
The morphological parameters as per updated Sydney system of classification of gastritis were analysed as follows. Accordingly, sections with a diffuse chronic inflammatory infiltrate including numerous lymphocytes and plasma cells expanding the lamina propria and the epithelium of the gastric mucosa were taken as chronic gastritis. Seventy two cases showed features of chronic gastritis. Sections showing neutrophilic infiltration along with chronic inflammatory cells were reported as chronic active gastritis. Neutrophils are seen in the lamina propria within the epithelium (particularly in the region of the glandular neck), and within the foveolar lumen, where they may form "pit abscesses/ crypt abscess". Fifty six cases showed activity. The bacterium were generally seen near the site of neutrophilic infiltration. This is quite clearly seen with Giemsa stain. Four cases of malignancy showed neutrophilic infiltration (Table 3).
| Histopathological findings | Neutorphil activity | Intestinal metaplasia | Lymphoid hyperplasia | Atrophy | H. pylori H & E/WSS |
|---|---|---|---|---|---|
| Normal-4 | - | - | - | - | - |
| Chronic gastritis-72 | 56 | 16 | 27 | 14 | 37/42 |
| Polyp-4 | 1 | - | - | - | - |
| Malignancy-20 | 4 | 9 | 2 | 3 | 13-Nov |
| Total-100 | 61 | 25 | 29 | 17 | 48/55 |
Table 3: Histopathological examination with H&E stain.
Sections with increased lymphocytic aggregates along with lymphoid follicles were also reported. Lymphoid hyperplasia was seen in twenty nine cases. Almost all H. pylori gastritis showed lymphoid hyperplasia. Intestinal metaplasia was seen in twenty five cases. In seven cases intestinal metaplasia was seen in the entire width of the gastric mucosa observed. Sixteen chronic gastritis cases showed intestinal metaplasia.
Atrophy of the glandular mucosa (decreased number of glands) was seen in seventeen cases. Fourteen cases of chronic gastritis showed atrophic changes.
In Warthin starry silver stain H. pylori appeared black spiral rods in a yellow background. Fifty five cases were positive with this stain. Gastric mucosal changes are not made out with this stain. Fifty one cases of H&E stained section showed H. pylori. Four cases which was negative with H&E was positive for Giemsa stain. Seven cases which was negative with H&E was positive for WSS stain. Three cases with low density H. pylori not stained with Giemsa was stained by WSS stain. Fifty five cases were H. pylori gastritis. Thirteen were positive for malignancy. Considering WSS as gold standard the sensitivity and specificity for Giemsa and H&E were calculated (Table 4). Sensitivity and Specificity of Stains is showed in Table 5.
| Satin | H. pylori |
|---|---|
| H & E | 48 |
| Giemsa | 52 |
| WSS | 55 |
Table 4: H. pylori.
| Stain | Sensivity | Specificity |
|---|---|---|
| H & E | 87.27% | 94.50% |
| Giemsa | 94.54% | 100% |
| WSS | 100% | 100% |
Table 5: Sensitivity and specificity of stains.
Gastric adeno carcinoma and polyps
Twenty cases were malignant with severe cytological abnormality with fused and cribriform glands. Eleven cases of malignancy were associated with chronic gastritis, four cases with intestinal metaplasia and three cases with atrophic gastritis. Thirteen cases were positive for H. pylori. Four cases were gastric mucosal polyps; three located in the corpus and one in the antrum. Four cases showed normal histological features.
Figure 1 to Figure 19 shows histopathological characteristics.
Figure 1. H. Pylori attached to gastric epithelium H & E 40x.
Figure 2. Poor visualization of H. pylori H&E 40x.
Figure 3. H. pylori attached to gastric epithelium giemsa 10x.
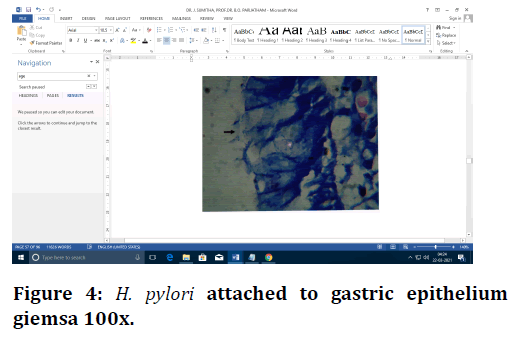
Figure 4. H. pylori attached to gastric epithelium giemsa 100x.
Figure 5. Gastric mucosa giemsa 10x.
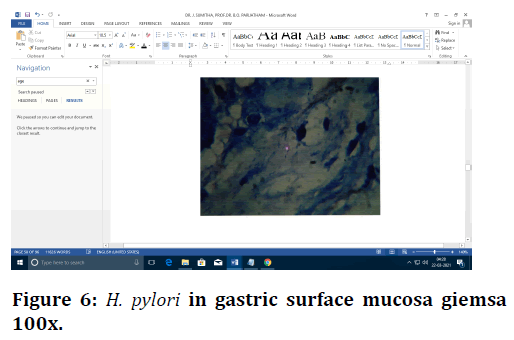
Figure 6. H. pylori in gastric surface mucosa giemsa 100x.
Figure 7. H. pylori WSS 4x.
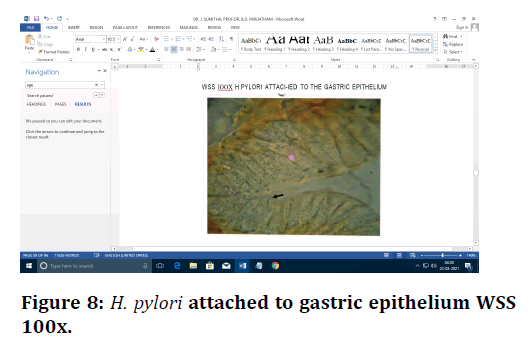
Figure 8. H. pylori attached to gastric epithelium WSS 100x.
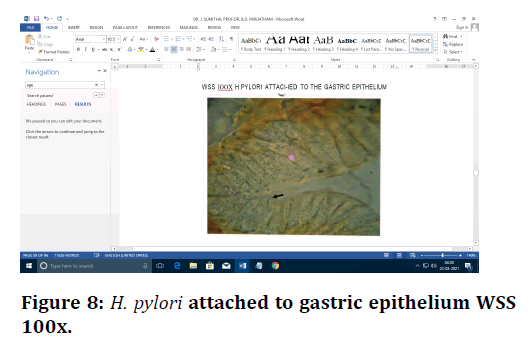
Figure 9. H. pylori attached to surface epithelium WSS 40x.
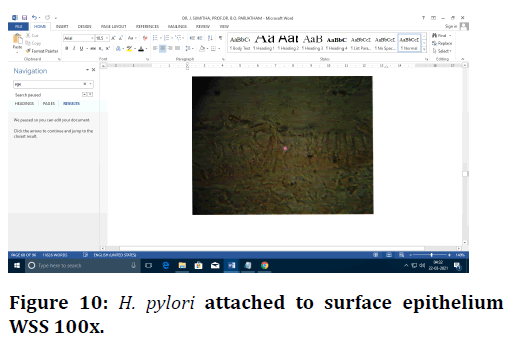
Figure 10. H. pylori attached to surface epithelium WSS 100x.
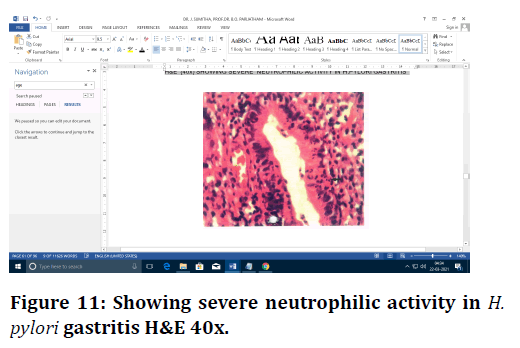
Figure 11. Showing severe neutrophilic activity in H. pylori gastritis H&E 40x.
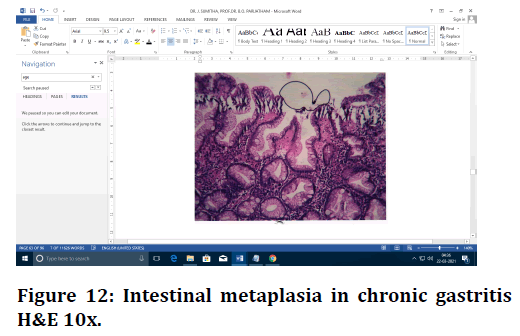
Figure 12. Intestinal metaplasia in chronic gastritis H&E 10x.
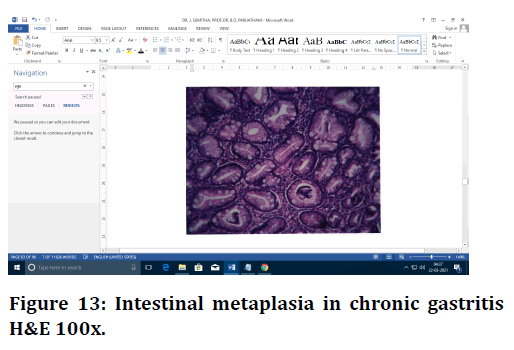
Figure 13. Intestinal metaplasia in chronic gastritis H&E 100x.
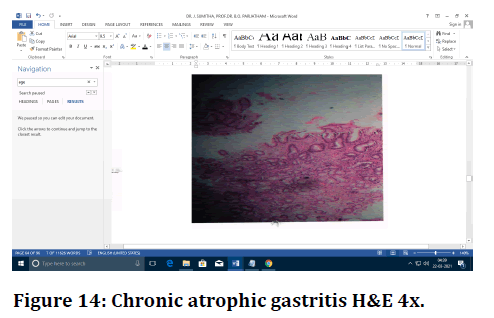
Figure 14. Chronic atrophic gastritis H&E 4x.
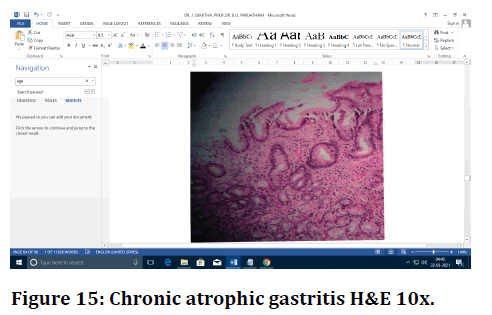
Figure 15. Chronic atrophic gastritis H&E 10x.
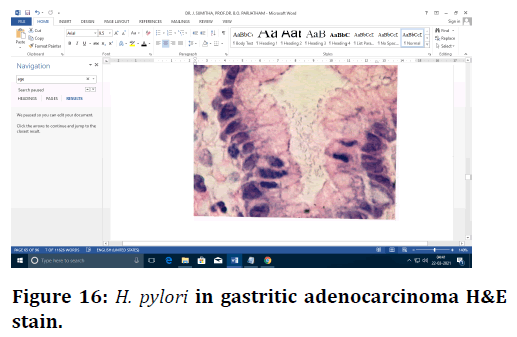
Figure 16. H. pylori in gastritic adenocarcinoma H&Estain.
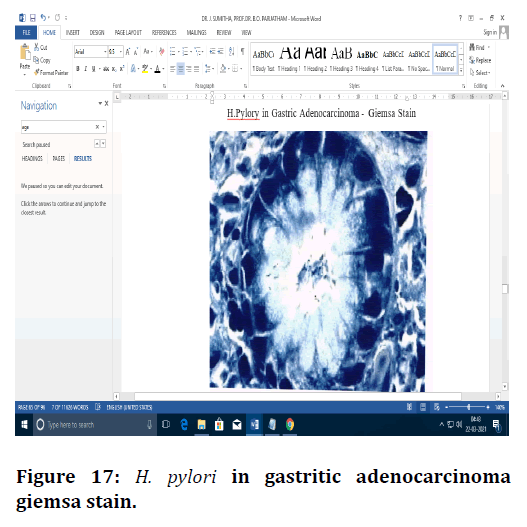
Figure 17. H. pylori in gastritic adenocarcinoma giemsa stain.
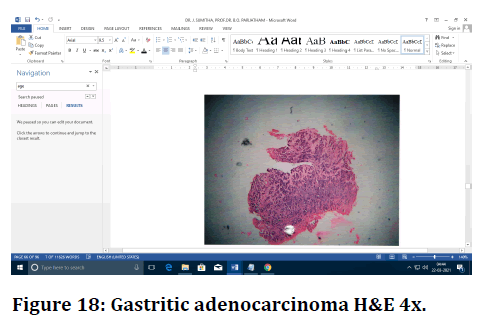
Figure 18. Gastritic adenocarcinoma H&E 4x.
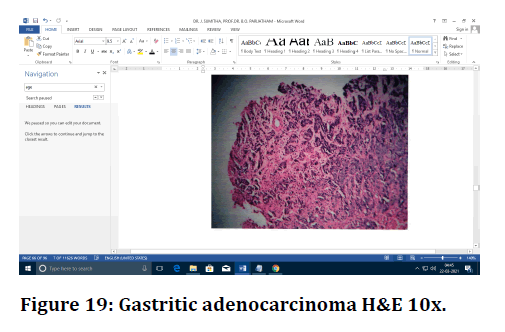
Figure 19. Gastritic adenocarcinoma H&E 10x.
Discussion
Biopsy sampling of the gastric mucosa at diagnostic endoscopy provides information that cannot be obtained otherwise. The most common indication for gastric biopsy is the need to know whether the patient is infected with Helicobacter pylori or not and whether the stomach is gastric or not. Microscopic examination of gastric biopsy specimens gives, in addition to H. pylori status, information about the grade, extent, and topography of gastritis- and atrophy-related alterations in the gastric mucosa. This information provides further possibilities for the assessment of risk and likelihood of various gastric disorders. In the present study H. pylori was positive in 55 cases. Of which forty two were pylori gastritis and thirteen were malignant. So 42 out of 72 cases were H. pylori gastritis (58.33%). So H. pylori are the most common cause for chronic gastritis in our study. This is comparable to studies done by Vijaya et al. [14] and Zhang et a1 [15]. In the present study activity (neutrophilic infiltration) was seen in 68 cases. (56 cases out of 72 chronic gastritis-77.7%). H. pylori are more densely seen near neutrophilic infiltration and crypt abscess. This is similar to study done by Tanko [16] in 2008. In their study, Neutrophil activity was observed in 83% of chronic gastritis.
In the current study, Intestinal metaplasia was seen in 25 cases. Of which 16 were seen with chronic gastritis and 9 with malignancy. So 16 out of 72 cases were showing intestinal metaplasia (23%). This is comparable to studies done by Tanko et al [16]. H. pylori was not seen with intestinal metaplasia. In such cases corporal biopsies of the same cases in some patients showed H. pylori. In the present study atrophy was seen in 17 cases. Of which 14 were seen with chronic gastritis and 3 with malignancy. So 14 out of 72 cases were showing intestinal metaplasia (19.4%).This is comparable to studies done by Abu Ahmad et al [17].
The normal gastric mucosa contains very few lymphocytes in the lamina propria. Lymphoid follicles and aggregates are characteristic of H. pylori associated gastritis. Lymphoid follicle prevalence between 27.4% and 100% has been reported in gastric mucosa from patients with H. pylori associated gastritis. Wyatt and Rathbone [18] investigated 419 pairs of antral and corporal mucosal biopsy specimens and found lymphoid follicles in 27.4% of patients with H. pylori associated gastritis. Eidt and Stolte studied "two to three antral specimens" from 2692 patients with H. pylori infection and detected lymphoid follicles and aggregates in 53.8% of those patients. Genta and Hammer [9] found that the prevalence of lymphoid follicles was 63.8% in patients with chronic gastritis and 100% in patients with H. pylori infection. In the present study lymphoid follicle was seen in 29 cases. Of which 27 were seen with chronic gastritis and 2 with malignancy. So 27 out of 72 cases were showing lymphoid follicle (37%). Twenty seven out of 42 H. pylori gastritis was associated with lymphoid hyperplasia (64%). This is somewhat similar to studies done by Eidt and Stolte et al [19]. Presence of neutrophils as a sign of activity & lymphoid follicles were found significantly in association with H. pylori infection, therefore presence of this feature might be taken as an indirect evidence for H. pylori infection.
In the present study chronic gastritis was seen in 58 out of 72 cases (80%) in the antrum, 12 cases out of 72 cases (16%) in the corpus. This is comparable to previous studies done. Maximum and minimum percentage positivity were observed at antral lesser curvature and corpus greater curvature, respectively. Eighty per cent of the patients had antral predominant gastritis and in 82%, H. pylori was predominantly observed in antral biopsies. Gastritis was more commonly seen in antrum compared to corpus, whereas carcinoma was found more in corpus.
Histopathalogical detection of H. pylori
In most cases, H. pylori can be recognized in a good H&E stain. However, the sensitivity of this is low especially when there are not many bacteria. Given the well documented implications of H. pylori infection, correct and prompt diagnosis is essential. Therefore, most laboratories use an additional staining method in the identification of the organism .In our study H&E stain could pick up H. pylori in moderate and severe density but could not pick up low density. Whereas Warthin starry stain were able to pick up most number of cases even at a low density. Similarly, the two investigators (Robin Warren & Barry Marshall) used H&E stain and Warthin-Starry silver method to identify H. pylori. But they observed that H. pyloriwere difficult to see with H&E stain, but stained well by the Warthin-Starry silver method.
Also WSS stain has been considered the gold standard for detection of H. pylori by Genta et al [20] in their study on comparison of H&E and Genta stain. A study by Cutler et a1 [21] for the detection of H. pylori by WSS stain has shown it to have a sensitivity of 93.1% and specificity of 99%. Marshall et al [22] were the first to use Warthin Starry Stain for the detection of H. pylori in histological sections prepared from gastric biopsy specimens. According to them H. pylori were difficult to see with H&E stain but stained well with Warthin Starry silver stain. So our study correlate well with Robert warren and Barry Marshall study, Genta et al study, Cutler et al study and study by Marshall et al. [22] Taking Warthin starry stain as gold standard, sensitivity and specificity for Giemsa & H&E were calculated.
Warthin-Starry silver stain was found to be the best stain for the detection of low density H. pylori infection. Giemsa stain has comparable sensitivity to Warthin- Starry silver stain in detection of routine H. pylori infection. It can therefore be used for detection of H. pylori infection of moderate to high density. Though H&E stain is well tested, cheap and an easy staining method, requiring a relatively short period of time to perform, with high reproducibility, it still missed a significant number of cases (25%) as compared to other two stains studied.
Carcinoma stomach
Twenty out of 100 gastric endoscopic biopsies (20 %) of patients were diagnosed as gastric carcinoma. In a study of 159 dyspeptic patients by Simha et al. [23] (28.9%) were cases of gastric cancer. Eight of the twenty patients (40%) in the present study belong to the Fifth decade. Similarly in a study of 39 cases by Usha et al. [24], maximum number of patients (33.3%) belonged to the fifth decade. Fourteen of the twenty (70%) were male, similar to the 59% recorded by Usha et al. in a study of 39 gastric cancer patients. Twelve of the twenty malignancy (60%) were locate in the corpus. This contrasts with the figures quoted by Mingl881 in which 52% of gastric cancers were located in antrum, 28% in fundus, and 11% both in fundus and pylorus and 9% in whole of the stomach.13 cases of carcinoma were H. pylori positive (65%).
Conclusion
Endoscopic gastric mucosal biopsies are commonly done in patients with dyspepsia, to rule out H. pylori infection, and other types of gastritis. H. pylori infection is the most common cause of chronic gastritis in our study similar to the results seen in other studies. Histology helps in finding associated premalignant & malignant lesions, in addition to H. pylori detection. It can be concluded from the present study that Warthin-Starry silver stain is the gold standard in staining H. pylori, especially when H. pylori density is low; the other two stains can be used when H. pylori density is high.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledegements
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Valla JD. Peptic ulcer disease and related disorders. In:Abrantine E, Adamson JW, Kokko LA, et al. (Eds) Harrison's principals of internal medicine. 15th Edn. 2001; 1:1653-4.
- Khokar N, Gill ML. Gastrointestinal injury from non-steroidal anti-inflammatory drugs. Rawal Med J 2003; 28:22-4.
- Anderson J, Anderson JV, Baker LRI, et al. Gastrointestinal disease. In: Kumar and Clark. Clinical medicine: 5th Edn. Philadelphia: WB Saunders 2002; 272.
- Minhas KZ, Goraya F, Javid S, et al. Endoscopic and histopathological evaluation of 306 dyspepsic patients. Pak J Gastroentrol 2003; 17:4-7.
- Rubin C. Are there three types of Helicobacter pylori gastritis?. Gastroenterology 1991; 112:2108.
- Bhattacharya B, Montgomery E. Non-neoplastic disorders of the stomach. In: Iacobuzio-Donahue CA, Montgomery EA, Ed. Gastrointestinal and liver pathology, Philadelphia, Elsevier 2005; 66-125.
- Dheer S, Levine MS, Redfern RO, et al. Radiographically diagnosed antral gastritis: Findings in patients with and without Helicobacter pylori infection. Br J Radiol 2002; 75:805.
- Appelman H. Gastritis: Terminology, etiology, and clinicopathological correlations-another biased view. Hum Pathol 1994; 25:1006.
- Genta R, Hamner H. The significance of lymphoid follicles in the interpretation of gastric biopsy specimens. Arch Pathol Lab Med 1994; 118:740.
- Madan E, Kemp J, Westblom T, et al. Evaluation of staining methods for identifying Campylobacter pylori. Am J ClinPathol 1988; 90:450.
- Morris A, Ali M, Thomsen L, et al. Tightly spiral-shaped bacteria in the human stomach: Another cause of active chronic gastritis?. Gut 1990; 31:139.
- Genta R, Graham D. Comparison of biopsy sites for the histopathologic diagnosis of Helicobacter pylori: A topographic study of H. pylori density and distt:ibution. Gastrointest Endosc 1994; 40:342.
- Fox JG, Wang TC. Inflammation, atrophy, and gastric cancer. J Clin Invest 2007; 117:60-9.
- Vijaya D, Chandrashekar N, Nagarantnamma T, et al. Simple stain for Helicobacter pylori. J Clin Diagnostic Res2012; 4:664-666.
- Zhang C, Yamada N, Wu YL, et al. Helicobacter pylori infection, glandular atrophy and intestinal metaplasia in superficial gastritis, gastric erosion, erosive gastritis, gastric ulcer and early gastric cancer. World J Gastroenterol 2005; 11:791-6.
- Tanko MN, Manasseh AN, Echejoh GO, et al. Relation between Helicobacter pylori, inflammatory (neutrophil) activity, chronic gastritis, gastric atrophy and intestinal metaplasia. Niger J ClinPract 2008; l1:270-4.
- Abu-Ahmad NM, Odeh A, Sallal AKJ. Prevalence of Helicobacter pylori gastritis at the north of Jordan. Jordan J Bio Sci 2011; 4:71-76.
- Wyatt, Dixon MF. Chronic gastritis-a pathogenetic approach. J Pathol 1988; 154:113-24.
- Stolte M, Eidt S. Chronic erosions of the antral mucosa: a sequel of Helicobacter pylori-induced gastritis. J Gastroenterol 1992; 30: 846-50.
- Genta RM, Rabason GO, Graham DY. Simultaneous visualization of H. pylori and gastric morphology: A new stain. Hum pathol 1994; 25:221-6.
- Cutler AF, Havstad S, Ma CK, et al. Accuracy of invasive and non-invasive test to diagnose H. pylori infection. Gastroenterol 1995; 36-41.
- Marshall BJ, Warren JR. Unidentified curved bacilli in stomach of patients with gastritis and peptic ulceration. Lancet 1984; 1:1311- 1315.
- Simha MR, Doctor VM. Histological analysis of upper gastrointestinal endoscopic biopsises. Indian J Gastroenterol 1986; 5:197.
- Usha Singh SD, Shukla HS, Gupta S, et al. A clinicopathological study of carcinoma stomach. Indian J pathol Microbiol 1988; 31:266-71.
Author Info
Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, IndiaCitation: Sumitha J, Parijatham BO, Clinocopathological Study on Gastro Endoscopic Biopsies in Patients with Special Reference to Helicobacter Pylori , J Res Med Dent Sci, 2021, 9(6): 352-359
Received: 08-May-2021 Accepted: 23-Jun-2021 Published: 30-Jun-2021
