Research - (2021) Volume 9, Issue 9
Comparative Evaluation of a Single Dose Dexamethasone With and Without Analgesic on Postoperative Outcomes after Removal of Mandibular Third Molars
Ramvihari Thota* and Senthilnathan Periasamy
*Correspondence: Ramvihari Thota, Department of Oral & Maxillofacial Surgery, Saveetha Dental College & Saveetha Institute of Medical and Technical Science, Saveetha University Tamilnadu, India, Email:
Abstract
Aim: The goal of this study was to see how a single dosage of dexamethasone and a combination of dexamethasone and ketorolac affected postoperative pain, trismus, and edoema following the removal of third molars. Materials and methods: The study looked at forty participants who were scheduled to have their lower third molars surgically removed. Two groups of patients were formed. After surgery, each patient in the first group received 8 mg dexamethasone IV and 30 mg ketorolac IM. Each patient in the second group received 8 mg dexamethasone IV alone following surgery. Postoperative pain was evaluated by visual analogue scale along with facial swelling and trismus on postoperative days 3 and 7. Results: Both the dexamethasone and dexamethasone-ketorolac combinations suppressed pain at the sixth postoperative hour. In comparison to the dexamethasone group, the dexamethasone-ketorolac combination group lost less opening on postoperative days 3 and 7. At postoperative day 3, the dexamethasone and dexamethasone-ketorolac combination groups had decreased postoperative edoema. In comparison to the dexamethasone group, the dexamethasone-ketorolac combination group showed less edoema on postoperative day 7. Conclusion: The combination of a single dosage of dexamethasone and ketorolac has been found to be effective in the treatment of postoperative discomfort, trismus, and edoema after dental surgical procedures, and should be used when substantial soft tissue swelling is expected.
Keywords
The extraction of impacted third molars causes severe soft and bone tissue damage, resulting in discomfort, edoema, and trismus. To prevent these postoperative complications, a variety of medicines have been utilised. Corticosteroids, for example, are well-known adjuncts to surgery for decreasing tissue inflammatory mediators, lowering fluid transudation and edoema [1-4]. Edema usually goes hand in hand with a decrease in postoperative pain, and corticosteroids have some inhibitory effects on prostaglandins [1].
Preoperatively in third molar surgery, single and varied doses of steroids were given intravenously or orally in previous research [5-9]. Dexamethasone has been shown to reduce postoperative edoema after third molar surgery. A single dosage of methylprednisolone decreased edoema and discomfort, but not trismus, in previous studies. Neupert et al [7] in their study after intravenous dexamethasone, no substantial reduction in edoema or trismus was seen.
In the management of postoperative pain and inflammation, nonsteroidal anti-inflammatory medications (NSAIDs) are commonly utilised. NSAIDs are commonly used following oral surgery, when the inflammatory process (including wound edoema and local peripheral dilatation) has already begun [10]. Ketorolac is an anti-inflammatory, antipyretic, and analgesic prostaglandin synthesis inhibitor with anti-inflammatory, antipyretic, and analgesic effects. Its effectiveness in odontology has been documented [10-12]. After impacted third molar removal, NSAIDs and steroids can significantly minimise postoperative sequelae. However, just a few studies have looked at how effective the combined effects of these two medications are. The goal of this study was to see how a single intramuscular dosage of dexamethasone, as well as a ketorolac-dexamethasone combination, affected postoperative pain, trismus, and edema following third molar surgery.
Materials and Methods
Forty healthy outpatients (25 men, 20 women) between 18 and 40 years of age who were to undergo surgical removal of mandibular third molars with partial bone impaction were studied. Patients were excluded from study if their medical history or physical examination suggested adrenal cortical suppression or corticosteroid use over the previous 3 months. Informed written consent was obtained from all patients. Patients were randomly allocated to 2 groups. The patients, surgeon, and examiner were blinded to test and control medications. The dexamethasone group (n 20) was administered 8 mg of dexamethasone intramuscularly after surgery, and 10 mg ketorolac was prescribed 2 times per day as needed. The combination group (n 20) was administered 8 mg of dexamethasone intramuscularly after surgery, and ketorolac 30 mg and prescribed with ketorolac 2 times per day was prescribed. After each operation, 500 mg oral amoxicillin 3 times per day for 5 days was prescribed. Lignocaine 2% plus 1:200.000 adrenaline was used for the inferior alveolar and buccal nerve blocks. All operations were performed by the same surgeon and assistant, using a standardized technique.
Pain intensities were evaluated by a visual analogue scale with horizontal line that ran from “no pain” (0) to “worst pain” (10). The assessments were made each hour during postoperative first 8 hours. Interincisal opening was evaluated by measuring the distance on maximal opening between the right maxillary and mandibular central incisor with a calliper. Measurements were made preoperatively and on postoperative days 3 and 7. Before surgery, the outer contour of the cheek was measured using the method described by Amin et al. [13]. This measurement was repeated on postoperative days 3 and 7 to register the degree of facial swelling. All measurements were performed by the same examiner. Differences between groups were analyzed with a 1-way analysis of variance (ANOVA).
Results
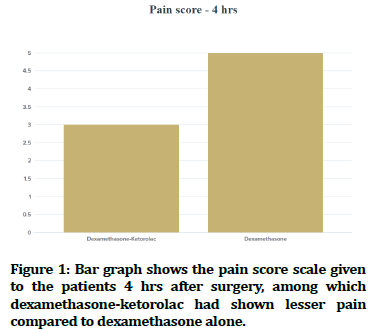
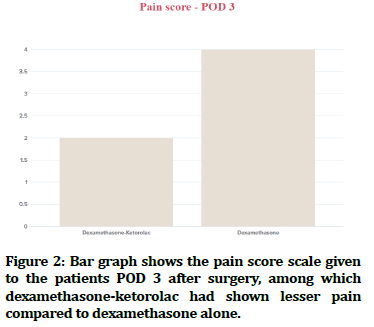
There was a significant difference in pain intensity between the dexamethasone and dexamethasoneketorolac groups at the sixth (P.016) and seventh (P.003) hours (Figures 1 and 2). At the 6-hour observation, the combination of dexamethasone and ketorolac reduced pain intensity in comparison to the control group (P.05). In contrast to control, both dexamethasone and dexamethasone-ketorolac combination decreased pain during the seventh postoperative hour (P .05). Although the dexamethasone-ketorolac combination group reported less pain at 4 and 5 hours than the dexamethasone group, there was no statistically significant difference in pain levels between the two groups.
Figure 1. Bar graph shows the pain score scale given to the patients 4 hrs after surgery, among which dexamethasone-ketorolac had shown lesser pain compared to dexamethasone alone.
Figure 2. Bar graph shows the pain score scale given to the patients POD 3 after surgery, among which dexamethasone-ketorolac had shown lesser pain compared to dexamethasone alone.
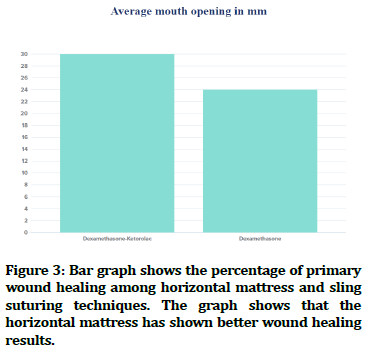
On days 3 (P.014) and 7 (P.023), there was a significant difference in interincisal opening between the dexamethasone and dexamethasone-ketorolac groups (Figure 3). In comparison to the dexamethasone group, the dexamethasone-ketorolac combination group lost less opening on postoperative days 3 and 7. (P .05).
Figure 3. Bar graph shows the percentage of primary wound healing among horizontal mattress and sling suturing techniques. The graph shows that the horizontal mattress has shown better wound healing results.
On days 3 and 7, there was a significant difference in postoperative edoema between the dexamethasone and dexamethasone-ketorolac groups (P-0.001). At postoperative day 3, the dexamethasone and dexamethasone-ketorolac combination groups had decreased postoperative edoema. In compared to the dexamethasone group, the dexamethasone-ketorolac combination group showed less edoema on postoperative day 7. (P-0.05). Although the dexamethasone-ketorolac combination group had reduced postoperative swelling than the dexamethasone group at postoperative day 3, there was no statistically significant difference between the two groups' postoperative swelling values (P-0.05).
Discussion
Even when teeth are removed using a moderate surgical approach, surgical removal of third molars produces substantial pain, edoema, and trismus. The use of steroids, which are effective anti-inflammatory medications, has been recommended as a way to lessen the complications associated with the removal of third molars. As a result, these individuals are an attractive clinical experimental model for studying these complications and the possible therapeutic effects of anti-inflammatory medicines. NSAIDs have been used to prevent postoperative pain in the majority of trials, [13,14] and to treat edoema and trismus, steroid injections have been employed [4,15]. Since the discovery of prostaglandins' function in local pain, inhibitors of prostaglandin production have been widely employed to prevent pain. Many studies have demonstrated the effectiveness of NSAIDs like diclofenac and ketorolac [10-12]. Because glucocorticoids like prednisolone and dexamethasone are strong anti-inflammatory drugs, they've also been utilised to manage postoperative complications in oral and maxillofacial surgery. [13-16]. Milles et al. [5] conducted a study where 11 patients were given 16 mg methylprednisolone orally the night before surgery and 20 mg methylprednisolone intravenously immediately before surgery in a crossover trial. At 48 hours after surgery, they found that a modest dosage of methylprednisolone decreased edoema by 34%. Holland et al. [5,16] showed the use of a single dosage of 40 mg intravenous methylprednisolone shortly before surgery reduced edoema 24 hours later, with no effect after 7 days. He also stated that the steroid only had a positive effect on pain on the first postoperative day.
Only a few studies have looked at the effectiveness of an NSAID and steroid combination in the management of postoperative pain after third molar surgery. Because of the analgesic qualities of the NSAID and the reduction of inflammation by both medicines, such a combination should theoretically result in maximum analgesic and anti-inflammatory efficacy. Our findings support this hypothesis. In comparison to the other group, the combination of dexamethasone and ketorolac reduced pain intensity. In comparison to both dexamethasone groups, the dexamethasone-ketorolac combination group lost less opening on postoperative days 3 and 7. On the third postoperative day, the dexamethasone and dexamethasone-ketorolac combination groups had decreased postoperative edoema. In comparison to both the dexamethasone and ketorolac groups, the dexamethasone-ketorolac combination group showed less edoema on postoperative day 7. The current study's findings demonstrate that combining ketorolac with dexamethasone has a superior analgesic and antiinflammatory effect than using a glucocorticosteroid alone.
Other studies have found that when the two medications are given together, the effect is amplified. Schultze- Mosgau et al. [17] showed in comparison to the placebo group, utilising a combination of ibuprofen and methylprednisolone, reported a 56 percent reduction in edoema. In contrast to placebo, the visual analogue scale indicated a 67.7% decrease in postoperative pain. Lin et al. [18] after third molar surgery, the combination of diclofenac and prednisolone had a superior analgesic and anti-inflammatory impact. Hyrkas et al. [19] the combination of methylprednisolone and diclofenac was compared to diclofenac. They discovered that combining methylprednisolone with diclofenac provided better pain alleviation than diclofenac alone.
There are a few contraindications to using steroids, including active or inactive TB, glaucoma, diabetes mellitus, and acute or chronic infection. Despite the fact that prolonged steroid usage can produce adrenal suppression, it has been reported that healthy patients given single massive doses of steroids had no adverse effects [6,19]. In addition, Williamson and colleagues found that after 7 days, the adrenal suppression caused by an 8 mg intravenous dosage of dexamethasone reverted to normal.
Many studies have demonstrated that dexamethasone reduces pain, although no clear mechanism for this action has been identified. According to the authors, the swelling rendered the tissue stiff and generated tension ache, which was relieved after the face edoema was reduced with dexamethasone. On day 3, when the highest swelling was seen, eight milligrams of dexamethasone intramuscularly dramatically decreased postoperative edoema. The large reduction in edoema most likely resulted in less tissue strain and discomfort.
Conclusion
Finally, a single 8 mg dexamethasone intramuscular injection was beneficial in greatly lowering pain on postoperative days 3 and 7. Dexamethasone can reduce postoperative edoema and discomfort following surgical extraction of lower third molars, but it has no effect on trismus following surgical extraction of third molars. The combination of a single dosage of dexamethasone and ketorolac has been found to be effective in the treatment of postoperative discomfort, trismus, and edoema after dental surgical procedures, and should be used when substantial soft tissue swelling is expected.
Acknowledegements
None. No funding to declare.
References
- James R, Hupp DMDJM, Myron R, et al. Contemporary oral and maxillofacial surgery. South Asia Edition E-Book 7th Edn Elsevier India 2019.
- Alexander RE, Throndson RR. A review of perioperative corticosteroid use in dentoalveolar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2000; 90:406–415.
- Montgomery MT, Hogg JP, Roberts DL, et al. The use of glucocorticosteroids to lessen the inflammatory sequelae following third molar surgery. J Oral Maxillofac Surg 1990; 48:179–87.
- Gersema L, Baker K. Use of corticosteroids in oral surgery. J Oral Maxillofac Surg 1992; 50:270–7.
- Milles M, Desjardins PJ. Reduction of postoperative facial swelling by low-dose methylprednisolone: an experimental study. J Oral Maxillofac Surg 1993; 51:987–91.
- Beirne OR, Ross Beirne O, Hollander B. The effect of methlyprednisolone on pain, trismus, and swelling after removal of third molars. Oral Surg Oral Med Oral Pathol 1986; 61:134–8.
- Neupert EA, Lee JW, Philput CB, et al. Evaluation of dexamethasone for reduction of postsurgical sequelae of third molar removal. J Oral Maxillofac Surg 1992; 50:1177–1182.
- Esen E, TaÅ?ar F, Akhan O. Determination of the anti-inflammatory effects of methylprednisolone on the sequelae of third molar surgery. J Oral Maxillofac Surg 1999; 57:1201–1206.
- ElHag M, Coghlan K, Christmas P, et al. The anti-inflammatory effects of dexamethasone and therapeutic ultrasound in oral surgery. Br J Oral Maxillofac Surg 1985; 23:17–23.
- Wuolijoki E, Oikarinen VJ, Ylipaavalniemi P, et al. Effective postoperative pain control by preoperative injection of diclofenac. Eur J Clin Pharmacol 1987; 32:249–52.
- Hyrkäs T, Ylipaavalniemi P, Oikarinen VJ, et al. Preoperative intravenous diclofenac for postoperative pain prevention in outpatients. Br J Oral Maxillofac Surg 1993; 31:351–354.
- van der Westhuijzen AJ, Roelofse JA, Grotepass FW, et al. Randomized double-blind comparison of tiaprofenic acid and diclophenac sodium after third molar surgery. Oral Surg Oral Med Oral Pathol 1994; 78:557–66.
- Amin MM, Laskin DM. Prophylactic use of indomethacin for prevention of postsurgical complications after removal of impacted third molars. Oral Surg Oral Med Oral Pathol 1983; 55:448–451.
- Hyrkäs T, Ylipaavalniemi P, Oikarinen VJ, et al. Postoperative pain prevention by a single-dose formulation of diclofenac producing a steady plasma concentration. J Oral Maxillofac Surg 1992; 50:124–127.
- Olstad OA, Skjelbred P. Comparison of the analgesic effect of a corticosteroid and paracetamol in patients with pain after oral surgery. Br J Clin Pharmacol 1986; 22:437–42.
- Holland CS. The influence of methylprednisolone on post-operative swelling following oral surgery. Br J Oral Maxillofac Surg 1987; 25:293–299.
- Schultze-Mosgau S, Schmelzeisen R, Frölich JC, et al. Use of ibuprofen and methylprednisolone for the prevention of pain and swelling after removal of impacted third molars. J Oral Maxillofac Surg 1995; 53:2–7.
- Lin TC, Lui MT, Chang RC. Premedication with diclofenac and prednisolone to prevent postoperative pain and swelling after third molar removal. Zhonghua Yi Xue Za Zhi 1996; 58:40–44.
- Hyrkäs T, Ylipaavalniemi P, Oikarinen VJ, et a. A comparison of diclofenac with and without single-dose intravenous steroid to prevent postoperative pain after third molar removal. J Oral Maxillofac Surg 1993; 51:634–636.
Author Info
Ramvihari Thota* and Senthilnathan Periasamy
Department of Oral & Maxillofacial Surgery, Saveetha Dental College & Saveetha Institute of Medical and Technical Science, Saveetha University Tamilnadu, Chennai, Tamil Nadu, IndiaCitation: Ramvihari Thota, Senthilnathan Periasamy,Comparative Evaluation of a Single Done Dexamethasone With and Without Analgesic on Postoperative Outcomes after Removal of Mandibular Third Molars, J Res Med Dent Sci, 2021, 9(9): 18-21
Received: 14-Aug-2021 Accepted: 06-Sep-2021