Research - (2021) Volume 9, Issue 4
Comparision of Esmolol and Labetalol in Low Doses for Attenuation of Sympathomimetic Response to Laryngoscopy and Intubation
Joshua Dhavanam Y, Ramlal Porika* and Kommuri Sudha
*Correspondence: Ramlal Porika, Department of Anaesthesiology, Gandhi Medical College/Gandhi Hospital, India, Email:
Abstract
Background and aims: Sympathoadrenal response to direct laryngoscopy and tracheal intubation invariably results in increases in heart rate and elevation in mean arterial pressure. In some instances arrhythmias can be precipitated. These potentially harmful responses may prove to be detrimental in patient at risk. Many techniques and various drugs have been employed to attenuate these haemodynamic responses. No single drug or technique is totally satisfactory. Thus there is a need to find a simple efficient and reliably consistent method.
Materials and methods: Prospective, randomized, controlled, single blinded trial comparing two adrenergic antagonists labetalol (nonselective) and esmolol (B1 selective) in decreasing the pressure response during rigid laryngoscopy and intubation in 90 patients of both sex, who belong to ASA -I &ASA-II of age group 18-55 years , from 2015-2016. Prospective, randomized, controlled, single blinded trial compares two adrenergic antagonists labetalol (nonselective) and esmolol (B1 selective) done by randomly allocating into three groups.
Results: In the control group heart rate, systolic, diastolic and mean arterial blood pressures showed wide fluctuation, a maximal increase at the time of intubation and returned gradually to basal values over 10 minutes. In Labetalol group significant suppression of heart rate and blood pressure was observed when compared to control group which returned to baseline at the end of 10min. whereas low dose esmolol (0.5 mg/kg) is inferior to that of labetalol for the same purpose.
Conclusion: In lower doses, labetalol is a better agent than esmolol in attenuating the sympathomimetic response to laryngoscopy and intubation whereas low dose esmolol is inferior to that of labetalol.
Keywords
Labetalol, Esmolol, Intubation
Introduction
Evidence from laboratory data demonstrates that epipharyngeal and laryngopharyngeal stimulation augments cervical sympathetic activity in efferent fibres of the heart. Even though the elevation in blood pressure and heart rate due to laryngoscopy and intubation are brief, they may have detrimental effects in high risk patients including myocardial infarction, cardiac failure, intracranial hemorrhage and increases in intracranial pressure.. Laryngoscopy and tracheal intubation induces changes in circulating catecholamine levels significantly. Norepinephrine, epinephrine and dopamine levels rise, but the raise in norepinephrine levels is consistently associated with elevation of blood pressure and heart rate [1]. Some authors infact consider the intubation period as one of the greatest risk phase in the surgical patients with coronary artery disease and patients with intracranial aneurysms. Although the response may be transient, it is invariable, significant, often persistent and of great concern.
The techniques of laryngoscopy and tracheal intubation are not confined only to the operating room, but are also employed for non anaesthetic purposes. Few instances are diagnostic laryngoscopy, fibreoptic bronchoscopy; intubation may be required for prevention of aspiration and protection of airway and during mechanical ventilation. All these procedures can also produce sympathetic responses and one should keep in mind that many of these patients are critically ill and at increased risk. Hence it is important to find an effective means of attenuating sympathetic responses to laryngoscopy and tracheal intubation. Many strategies have been advocated to minimize these hemodynamic adverse responses and aimed at different levels of the reflex arc [2]. Block of the peripheral sensory receptors and afferent input – topical application and infiltration of local anaesthetic to superior laryngeal nerve. Block of central mechanism of integration and sensory input – fentanyl, morphine etc. Block of efferent pathway and effector sites i.v. lignocaine, beta blockers, calcium channel blockers, hydralazine etc. No single drug or technique is satisfactory. The aim of this study is to compare esmolol, labetalol and Placebo for the attenuation of the cardiovascular response to direct laryngoscopy and intubation during General Anesthesia.
Materials and Methods
Prospective, randomized, controlled, single blinded trial comparing two adrenergic antagonist’s labetalol (nonselective) and esmolol (B1 selective) in decreasing the pressure response during rigid laryngoscopy and intubation was conducted in the Department of Anaesthesiology & Critical Care Gandhi Hospital, Secunderabad on 90 patients. The study after obtaining approval of ethics committee of hospital and with written informed consent to evaluate the efficacy of esmolol and labetalol in attenuating pressor response to laryngoscopy and intubation. Ninety patients who fulfill the following criteria were included in the study.
Inclusion criteria: ASA physical status I and II of both genders with Weight between 35-80 kgs, Age between 18‐55 years, elective surgical procedures, requiring general anesthesia and orotracheal intubation were included in the study.
Exclusion criteria: ‐ Patients with cardiovascular, pulmonary ,hepatic ,and renal disease; Those on Beta blockers; Patients with difficult airway, Laryngoscopy and intubation time more than 30 s, or requiring more than two attempts were excluded from the study.
Sample size: ‐ Ninety patients (N=90) were divided into three groups, group C (control n=30), group E (esmolol n=30) and group L (labetalol n=30) were taken.
Pre-anaesthetic evaluation was done on the evening before surgery with complete history, clinical, airway and systemic examination of cardiovascular and respiratory was done.
99 All the selected patients were allocated into three groups consisting of 30 patients each.
99 Blinding was done using SNOSE (Sequentially numbered opaque sealed envelope) technique.
99 GROUP –C: Is the control group who received 10ml of 0.9% normal saline IV as placebo.
99 Group E: Is the Esmolol group who received 0.5 mg/ kg diluted with 0.9 % saline to 10 ml IV.
99 Group L: Is the Labetalol group who received 0.25 mg / kg diluted with 0.9% saline to 10 ml IV.
All patients included in the study were premedicated with tablet Alprazolam 0.5 mg and tablet Ranitidine 150 mg orally at bed time the previous night before surgery. They were kept nil orally 10 pm onwards on the previous night. All patients underwent the basic investigations were done.
On arrival of the patient in the operating room, an 18-gauge intravenous cannula was secured and an infusion of ringer lactate was started. The patients were connected to multiparameter monitor that records heart rate, non-invasive measurements of SBP, DBP, MAP, EtCO2 and continuous ECG monitoring and oxygen saturation. The baseline systolic, diastolic blood pressure, mean arterial pressure and heart rate were recorded. The cardiac rate and rhythm were also monitored from a continuous visual display of electrocardiogram from lead II.
In the control group 10ml of 0.9%saline was given both at 2 ,5 min prior to intubation. In the Esmolol group 0.5mg/kg of esmolol (diluted with 0.9%saline to 10ml) was given 2min prior and 10ml of 0.9%saline 5 min prior to intubation. In the labetalol group 10ml of 0.9%saline administered 2min prior and 0.25mg/kg of labetalol (diluted with 0.9%saline to 10ml) 5 min prior to intubation. All patients were premedicated intravenously 10 min prior to induction with inj. ondansetron 0.1 mg/kg, inj. Tramadol 2 mg/kg, inj. midazolam 0.05 mg/kg and inj.glycopyrrolate 0.2mg.
The patients were pre-oxygenated with 100% 02 by a face mask for 3 min. Induction was done with inj. thiopentone 5mg/kg and after 30 s relaxation achieved with inj succinylcholine 2 mg/kg 90s later the patient was intubated using a Macintos laryngoscope. All intubations were done by the experienced laryngoscopist. Tracheal tubes of ID 7.0 mm and 8.5 mm were used for female and male patients, respectively. Anesthesia was maintained by N2O (60%) and O2 (40%), intermittent boluses of vecuronium bromide intravenously and propofol infusion (5 mg/kg/hr). At the end of surgery, neuromuscular blockade was reversed with inj. neostigmine (40μg/kg) and inj. atropine (20 μg/kg).
HR, systolic blood pressure (SBP), and diastolic blood pressure (DBP) were recorded prior to induction, at time of intubation and 1, 3, 5, and 10 min after intubation. Mean arterial pressure (MAP) was also calculated for the same time stations. Abnormal ECG changes were also recorded. We studied the hemodynamic response to laryngoscopy and intubation for a period of 10 min as this is the average period for which hemodynamic changes are believed to last.
Results
The average age was 35.83 years in group C, 36.53 years in group E and 36.2 years in group L .Youngest patient in the study group was 28 years and oldest was 48 years. The average weights of the patients were 55.37 kgs in group C, 56.57 kgs in group E ,55.53 kgs in group L respectively. There was no significant difference in age and weight among the three groups. There was no significant difference in gender among the three groups (Table 1).
| Group C | Group E | Group L | p value C and E | p value E and L | p value C and L | |
|---|---|---|---|---|---|---|
| Mean Age(yrs) | 35.93 ± 4.72 | 36.2 ± 4.49 | 35.86 ± 4.73 | 0.82 | 0.77 | 0.95 |
| Weight(Kg) | 55.36 ± 10.51 | 55.57 ± 10.94 | 55.53 ± 10.36 | 0.94 | 0.988 | 0.94 |
| Male/Female | 15/15 | 16/14 | 15/15 | 1 | 1 | 1 |
Table 1: Comparison of age and weight distribution among the groups (N=90).
The pre induction values of pulse rate (PR) were comparable between groups with no significant difference. There was no statistically significant difference in PR throughout study time between the esmolol and control groups (p>0.05). At intubation and 1, 3, 5 and10 min post intubation PR was significantly lower in the labetalol group compared to the control group. (p<0.05). The PR were significantly less in the labetalol group throughout the study time compared with the esmolol group at intubation and 1,3,5 and10 min post intubation (Figure 1).
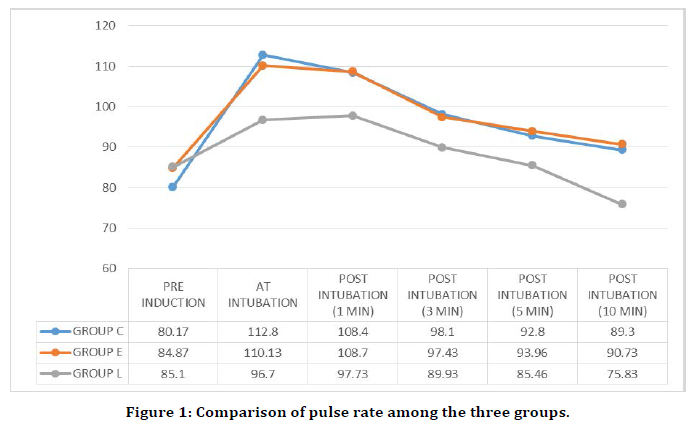
Figure 1. Comparison of pulse rate among the three groups.
The pre induction values of SBP were comparable between groups with no significant difference. SBP increased in both esmolol and control groups at all times except at 10th min post intubation. However, no significant difference was present among the groups (p>0.05). Compared with the control group values SBP was significantly lower at all-time stations in the labetalol group at intubation and 1,3,5and10 min post intubation (p<0.05). SBPs were significantly less in patients receiving labetalol compared to those who received esmolol (p<0.01 at intubation and 1, 3 ,5 and 10th min post intubation) (Figure 2).
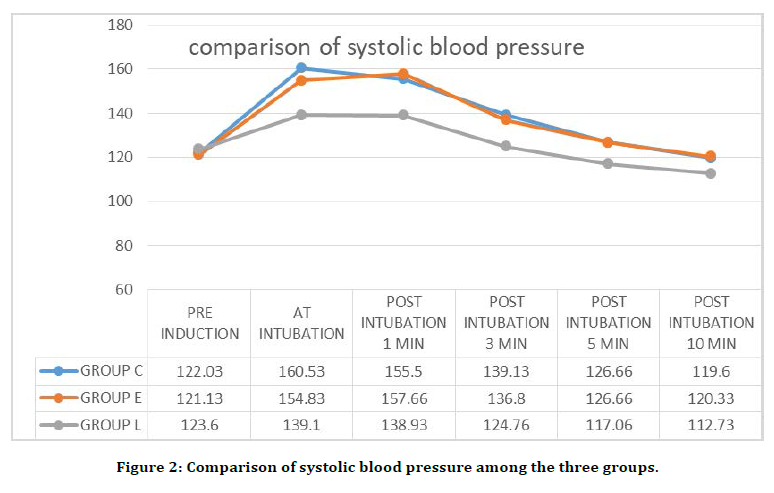
Figure 2. Comparison of systolic blood pressure among the three groups.
The pre induction values of DBP were comparable between groups with no significant difference. Below given (Table 1)shows that DBP at 1 minute post intubation in the esmolol group was significantly less than that in the control group (p=0.0038). At all other times it was comparable between the groups (p>0.05). DBP in the labetalol group was comparable with the control group with no significant difference. Diastolic pressures were not significantly different between labetalol and esmolol groups (p>0.05) (Figure 3).
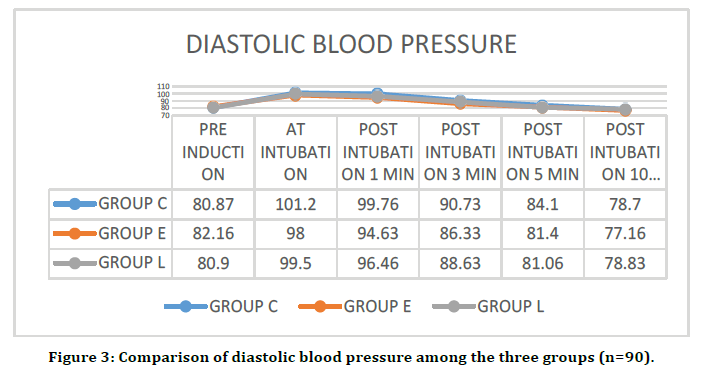
Figure 3. Comparison of diastolic blood pressure among the three groups (n=90).
The pre induction values of MAP were comparable between groups with no significant difference. MAP was significantly less at the time of intubation in the esmolol group (p<0.05) compared with the control group. All other postintubation values were comparable between the two groups and not statistically significant (p>0.1).Compared with controls as shown in the table, it was significantly less in the labetalol group at all times except at 10th minute post intubation, There was no statistically significant difference between values of labetalol and esmolol groups (p>0.05), except at the time of intubation, 1 and 3 min post intubation when it was significantly less in the labetalol group (Figure 4).
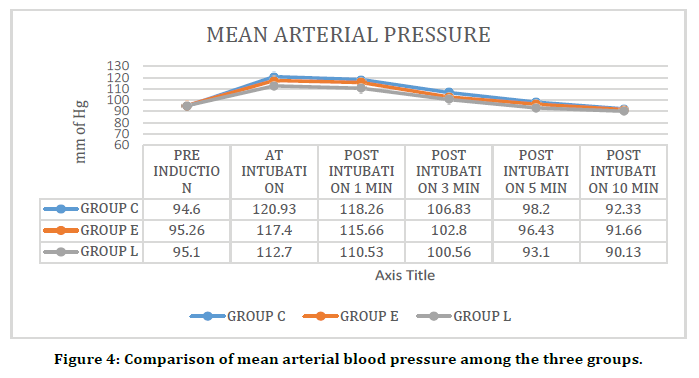
Figure 4. Comparison of mean arterial blood pressure among the three groups.
Discussion
The sequence of induction of anaesthesia, laryngoscopy and tracheal intubation are associated with marked hemodynamic changes and autonomic reflex activity which may be a cause of concern in many high risk patients [3]. Laryngoscopy and intubation is associated with rise in heart rate, blood pressure and incidence of cardiac arrhythmias. These potentially dangerous changes disappear within 5 minutes of onset of laryngoscopy [4]. Although these responses of blood pressure and heart rate are transient and short lived they may prove to be detrimental in high risk patients especially in those with cardiovascular disease, increased intracranial pressure or anomalies of the cerebral blood vessels.
Attenuation of sympathetic responses during laryngoscopy and intubation is of prime concern to the anesthesiologist more so in high risk subjects as mentioned earlier. Many strategies have been recommended which include minimizing the duration of laryngoscopy to less than 20 seconds, topical application of local anesthetics, Beta blockers calcium channel blockers, Clonidine, Sodium Nitroprusside lignocaine. No single drug or technique is satisfactory9. Each technique has advantages and disadvantages, the most obvious being that the prevention often outlasts the stimulus. Bachofen M4 stated the criteria for selection appropriate drug to prevent sympathetic response. The drug must be applicable regardless of patient collaboration, prevent impairment of cerebral blood flow and avoid arousal of the patients. It should neither be time consuming nor affect the duration and modality of ensuing anesthesia. Beta blockers have been compared with fentanyl, nitroprusside, nitroglycerine, calcium channel blockers, etc.; however, studies comparing esmolol (cardio selective beta blocker) and labetalol (nonselective adrenergic blocker) are lacking.
Esmolol hydrochloride is an ultra-short acting, beta-one selective adrenergic receptor blocker with a distribution half-life of 2 min and an elimination half-life of 9 min. Esmolol appears quite suitable for use during a short-lived stress such as tracheal intubation or ECT. Labetalol is an adrenergic receptor blocking agent with mild alpha1- and predominant beta-adrenergic receptor blocking actions (alpha:beta blockade ratio of 1:7 for iv and 1:3 for PO administration). The onset of action of i.v. labetalol is 5 min. We studied the hemodynamic response to laryngoscopy and intubation for a period of 10 min as this is the average period for which hemodynamic changes are believed to last. Demographic data comparing age, sex, weight shows no statistically significant difference among the three groups and has been compared with other studies.
In present study mean age group of control group ,esmolol and labatelol was 35.93 ± 4.72, 36.2 ± 4.49,and 35.86 ± 4.73 respectively which was comparable to the study conducted by Singh et al. [5] in which the mean age group of control group ,esmolol and labatelol was 30.28,31.08 and 30.56 respectively. In present study the sex ratio is 15:15 in control group which is coming to 50% males and 50% females, sex ratio is 16:14 in esmolol group which is coming to 53.3% males and 46.7% females and sex ratio is 15:15 in labetalol group which is coming to 50% males and 50% females. In the study conducted by Singh, et al. [5]. The total number of patients taken are 75 among which the sex ratio (male:female) is 17:8 in control group which is coming to 68% males and 32% females, sex ratio is 15:10 in esmolol group which is coming to 60% males and 40% females and sex ratio is 15:10 in labetalol group which is coming to 60% males and 40% females which shows that the sex distribution is comparable to the present study.
In present study mean weight distribution in kg in control group which is coming to 55.36 ± 10.51 ,mean weight distribution in kg in esmolol group which is coming to 56.57 ± 10.94 and mean weight distribution in kg in labetalol group which is coming to 55.53 ± 10.36 . In the study conducted by Singh et al. [5] the total number of patients taken are 75 among which the weight distribution in kg in control group which is coming to 58.1 , weight distribution in kg in esmolol group which is coming to 56 and weight distribution in kg in labetalol group which is coming to 57.8 which shows that the weight distribution is comparable to the present study.
In the study conducted by Singh et al. [5] 75 patients were scheduled for general anaesthesia the baseline pulse rates were recorded and heart rates were compared at intubation1,3,5,and10 min post intubation between control group ,esmolol and labetalol group. There was no significant effect of esmolol on PR when compared to the control group. Labetalol had a significantly (p<0.05) better effect than esmolol in controlling PR at all points during the study.
In our study also there was no significant effect of esmolol on PR when compared to the control group. Labetalol had a significantly (p<0.05) better effect than esmolol in controlling PR at all points during the study. It seems that when instrumentation stimulus is present labetalol maintains the PRs within normal ranges. When the effect of stimulus weans off, as occurs at 10 min postintubation, the drug`s effect takes over and pulse rates go below baseline values.
In the study conducted by Singh et al. [5] 75 patients were scheduled for general anaesthesia the baseline systolic blood pressures were recorded and were compared at intubation1,3,5,and10 min post intubation between control group ,esmolol and labetalol group. In preventing the increases in SBP esmolol was completely ineffective as there was no significant difference between values of esmolol and control groups during the study period (p>0.05). Labetalol prevented the increase in SBP significantly throughout the study period as compared to control and esmolol groups (p<0.05). In our study also there was no significant difference between values of esmolol and control groups during the study period (p>0.05). Labetalol prevented the increase in SBP significantly throughout the study period as compared to control and esmolol groups (p<0.05).
Ramanathan et al. [6] used 20 mg labetalol to prevent rise in SBP successfully. Inada [7] found 10 mg (0.14 mg/kg) labetalol ineffective in attenuating the rise in systolic pressure. This difference might be because of the lower dose they used and the timing of giving of labetalol (2 min prior to intubation) because of which the peak effect of drug was lost at intubation. Maharaj [8] failed to blunt the blood pressure response with 0.25 and 0.5 mg/kg labetalol. However, they did not mention the timing of giving the drug. Esmolol even in doses exceeding >1mg/kg have been found to be ineffective in controlling systolic pressure rise.
In the study conducted by Singh et al. [5] 75 patients were scheduled for general anaesthesia the baseline diastolic blood pressures were recorded and were compared at intubation1,3,5,and10 min post intubation between control group ,esmolol and labetalol group. When compared to controls the rise in DBP was not attenuated (p>0.05) in any of the study groups .There was a significant difference between esmolol and control values at 1 minute postintubation (p<0.05). This was an isolated finding because no significant difference was observed at subsequent points of study. In intergroup comparison of esmolol and labetalol, none of them was found to be better (p>0.05).
In our study conducted in which 90 patients were scheduled for general anaesthesia the baseline diastolic blood pressures were recorded and were compared at intubation 1,3,5,and10 min post intubation between control group ,esmolol and labetalol group. When compared to controls the rise in DBP was not attenuated (p>0.05) in any of the study groups .There was a significant difference between esmolol and control values at 1 minute post intubation (p<0.05) and there was a significant difference between labatelol and control values at 1 minute post intubation (p<0.05) This was an isolated finding because no significant difference was observed at subsequent points of study. In intergroup comparison of esmolol and labetalol, none of them was found to be better (p>0.05).
In the study conducted by Singh, et al. [5] 75 patients were scheduled for general anaesthesia the baseline mean arterial blood pressures were recorded and were compared at intubation1, 3, 5, and 10 min post intubation between control group ,esmolol and labetalol group. Comparing the esmolol group with control revealed that the esmolol group had a significantly less MAP at intubation (p=0.044). When the labetalol group was compared with the control group the MAP was significantly less at all points (p<0.05) except at 10 min post intubation when the values were comparable. Between esmolol and labetalol there was no significant difference in values except at 1 min post intubation (labetalol having lower MAPs). This observation was an isolated finding and no significant difference (p>0.05) was found at any other point during the study period.
In our study 90 patients were scheduled for general anaesthesia the baseline mean arterial blood pressures were recorded and were compared at intubation 1, 3,5, and10 min post intubation between control group ,esmolol and labetalol group. Comparing the esmolol group with controls revealed that the esmolol group had a significantly less MAP at intubation (p=0.0247). This observation is the same as made by Sharma et al. [9] and Bakiye et al. [10] in their studies, although esmolol was not at all effective in controlling MAP rise after laryngoscopy and intubation (p>0.05) thereafter . When the labetalol group was compared with the control group the MAP was significantly less at all points (p<0.05) except at 10 min post intubation which is comparable with the study conducted by Singh Between esmolol and labetalol There was no statistically significant difference between the groups (P>0.05), except at the time of intubation 1 and 3 min post intubation when it was significantly less in the labetalol group. MAP increase was attenuated by labetalol but not esmolol.
The only side effect observed was that of labetalol in form of bradycardia, intraoperatively. Nine patients (30 %) developed bradycardia (pulse rate <50 beats per minute) after the study period of 10 min and had to be given atropine in 0.2 mg increments (max. 0.01 mg/kg). All the patients responded to atropine treatment. There were no recurrent episodes of bradycardia. No other side effects were observed. We recorded three episodes of atrial ectopics just after intubation. The atrial ectopics recorded in our study were attributed to tracheal intubation and not thiopentone induction. All three ectopics occurred at the time of intubation or just after the intubation and there were no abnormal ECG changes between the duration of induction and intubation.
Conclusion
In lower doses, labetalol (0.25 mg/kg) is a better agent than esmolol (0.5 mg/kg) in attenuating the sympathomimetic response to laryngoscopy and intubation whereas low dose esmolol (0.5 mg/kg) is inferior to that of labetalol for the same purpose. Bradycardia is a potential side effect of labetalol.
References
- Low JM, Harvey JT, Prys-Roberts C. et al. Studies of anaesthesia in relation to hypertension. VII: Adrenergic response to laryngoscopy. Br J Anaesth 1986; 58:471-477.
- Warwick W. Gray’s anatomy. 36th Edn. Edinburgh: Churchill Livingstone, 2000.
- Black TE, Kay B, Healy TEJ. Reducing the hemodynamic responses to laryngoscopy and intubation. Anaesth 1984; 39:883-887.
- Bachofen M. Suppression of blood pressure increases during intubation: Lidocaine or fentanyl. Anaesth 1988; 37:156-161.
- Singh SP, Quadir A, Malhotra P. Comparison of esmolol and labetalol, in low doses, for attenuation of sympathomimetic response to laryngoscopy and intubation. Saudi J Anaesth 2010; 4:163–168.
- Ramanathan J, Sibai BM, Madie WC, et al. The use of labetalol for attenuation of hypertensive response to endotracheal intubation in preeclampsia. Obstet Gynecol 1988; 159:650-654.
- Inada E, Cullen DJ, Nemeskal R, et al. Effect of labetalolon the hemodynamic response to intubation: A controlled, randomized double-blind study. J Clin Anesth 1989; 1:207-213.
- Maharaj RJ, Thompson M, Brock JG, et al. Treatment of hypertension following endotracheal intubation. A study comparing the efficacy of labetalol, practolol and placebo. S Afr Med J 1983; 63:691-694.
- Sharma S, Mitra S, Grover VK, et al. Esmolol blunts the haemodynamic responses to tracheal intubation in treated hypertensive patients. Can J Anaesth 1996; 43:778-782.
- Bakiye U, Ogurlu M, Gezer E. Effects of esmolol, lidocaine and fentanyl on haemodynamic responses to endotracheal intubation: A comparative study. Clin Drug Investig 2007; 27:269-277.
Author Info
Joshua Dhavanam Y, Ramlal Porika* and Kommuri Sudha
Department of Anaesthesiology, Gandhi Medical College/Gandhi Hospital, Hyderabad, IndiaCitation: Joshua Dhavanam Y, Ramlal Porika, Kommuri Sudha, Comparision of Esmolol and Labetalol in Low Doses for Attenuation of Sympathomimetic Response to Laryngoscopy and Intubation, J Res Med Dent Sci, 2021, 9 (4):137-144.
Received: 07-Mar-2021 Accepted: 19-Mar-2021
