Review - (2023) Volume 11, Issue 2
Comparison of clinical performance of flapless implant surgery and conventional flap elevation: a systematic review and meta-analysis
Krishankumar Lahoti*, Sayali Dandekar, Jaykumar Gade, Megha J Agrawal, Minal N Soni and Karan V Jaiswal
*Correspondence: Krishankumar Lahoti, Department of Prosthodontics, Swargiya Dadasaheb Kalmegh Smruti Dental College and Hospital, India, Email:
Abstract
Statement of problem: Clinicians prefer Branemark’s conventional flap elevation approach for implant placement and flapless implantation is still considered a blind procedure with questionable outcomes. Purpose: The purpose of this systematic review was to compare the clinical performance of flapless implant surgery with conventional flap elevation.
Material and Methods: A systematic search of Medline/PubMed and Google scholar databases for articles published before June 2020 was performed by 2 independent reviewers. A manual search of articles was also conducted. Studies published in English that evaluated the survival rate in patients with implant prosthesis were included. The Cohen kappa method was used to calculate inters reviewer agreement.
Results: Twenty three studies were included. Failure rate of dental implants was affected by different insertion technique with a RR of 1.55 (flapless placement vs flap surgery; 95% CI: 0.94 to 2.57; P=0.09) which was not found to be significant.
Conclusion: Flapless surgery can be a possible alternative as it has comparable outcomes with the conventional flap elevation technique. Clinical Implications: Flapless technique should be given consideration in patients whenever appropriate conditions pertaining to the alveolar bone and soft tissue are available as it has comparable clinical performance with conventional flap elevation technique of implant placement.
Keywords
Implant surgery
Introduction
The Brane mark protocol for implant offers an extensive flap elevation approach and is considered as a conventional procedure which is practiced routinely [1]. This approach provides for good visibility of the available underlying bone and is quite frequently necessary for treating bone defects. Over the last few years emphasis is being placed on simplification of the implant placement procedure and for reducing the treatment time which has led the attention towards flapless implantation which entails implants being placed through the mucosa without reflection of the muco-periosteal flap. This can be carried out using blind or digitally planned static guide templates. Furthermore, dynamic navigation systems can be used for improved precision and accuracy [2].
Flapless implantation being less traumatic is known to have benefits like reduced bone resorption, decreased discomfort, shorter treatment duration [3,4]. It also helps to preserve the vascularity, soft‑tissue architecture. Flapless implantation allows the patient to resume normal oral hygiene measures immediately after the procedure [5]. Despite having several advantages, flapless procedure is still feared by many clinicians considering the risks associated with it. Though several reports and clinical trials have been reported but no definitive conclusion could be reached. Therefore, a meta-analysis of published trials was conducted to compare the clinical performance of flapless implant surgery with conventional flap elevation.
Materials and Methods
This review was according to the guidelines of the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement [6].
Study protocol
Before the start of the systematic review, a protocol was developed and registered (Prospero ID: CRD42020197218) aiming to answer the P.I.C.O. question
Population: Patients requiring placement of implant.
Interventions: Flapless implant placement.
Comparison: Conventional Flap Implant placement.
Outcomes: survival rate of implant placement.
Study design
A combination of in vivo studies involving either or both the arches, comparative prospective and randomized or Non-randomized and retrospective clinical trials were included. The presence of comparator and interventional group was a necessary criterion of inclusion.
Inclusion criteria
Prospective randomized or non-randomized studies
Retrospective studies
Exclusion criteria
Review articles on the topic
Case reports and case series
Preclinical studies in animal models
In vitro studies
Retrospective studies
Search strategy
Two electronic databases were used as sources in the search for studies satisfying the inclusion criteria: (a) The National Library of Medicine (MEDLINE via PubMed); (b) Google Scholar for studies published until June 2020.
Search terms combinations of the following key words: ‘‘dental implant’’; ‘‘surgery’’; ‘‘flap’’; and ‘‘flapless’’; “Flapless versus Flap surgery”; “survival rate” with the Boolean operator. Subsequently, a manual search was conducted based on the reference lists of studies included and relevant reviews.
Data extraction
Relevant information was extracted by reviewers for accuracy. Data collected comprised of authors; year of publication; study design; number, age range, and gender distribution of participants; number, type, system, and location of implants; tools for flapless surgery; freehand or guided flapless surgery; implant survival rate, marginal bone loss, follow-up.
Risk of bias in individual trials
Two reviewers independently assessed the risk of bias for each eligible study. The risk of bias of studies was estimated as “low”, “Moderate”, or “high” for each item including following aspects i.e. random sequence generation, allocation concealment, blinding of outcome assessment, incomplete outcome data, blinding of participants and personnel, selective reporting and other bias in the tool.
Statistical analysis
The statistical heterogeneity among studies was assessed using the Q test based on Chi square statistics as well as the I2 index in order to know the percentage of variation in the global estimate that was attributable to heterogeneity (I 2=25%: low; I 2=50%: moderate; and I 2=75%: high heterogeneity). The primary outcome of this meta-analysis was to evaluate the survival rate of implant placement with flapless and flap elevation surgical approach. In the case of dichotomous outcome (exposure events), the estimates of the effect were expressed in risk ratios and 95% CIs. Study estimates were pooled with both the fixed and random effect models. Subgroup analysis was performed considering the difference in the loading protocol and the follow up period of the studies included. Studies having follow up period more than or equal to 3 years were included in the meta-analysis of long term effect of the placement technique on implant survival. In the studies where implants were loaded immediately, analysis was performed to check the effect of immediate loading on the outcome.
Results
Literature search
After the search strategy, a total of 4187 records were identified, and the selection process is summarized in Figure 1.
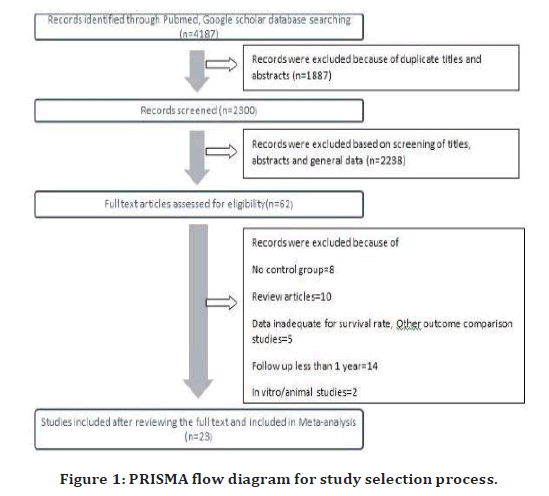
Figure 1. PRISMA flow diagram for study selection process.
One thousand eight hundred eighty-seven records were excluded for duplicated titles and abstracts, with 2300 records retained. After screening the titles and abstracts, 2238 records were further excluded based on the prespecified inclusion and exclusion criteria. Consequently, 62 records were suitable for full-text screening. After full-text screening, 39 articles that did not meet the requirement were further excluded, of which 8 did not have control group, 10 were reviews or meta-analysis, 5 articles did not have adequate data for meta-analysis/ or had other outcome measures, 14 studies had a follow up of less than 1 year and 2 studies were in vitro/animal studies. Eventually, a total of 23 publications were included in the meta-analysis.
The Cohen’s Kappa value for measuring the agreement strength between the reviewers during study selection were 0.91 in the initial screening of articles and 0.96 in full text assessment indicating “almost perfect” interagreement.
Description of the Studies
These included studies consisted of 23 clinical studies out of which 10 were randomized controlled trails and 2 were retrospective. The descriptive details of these studies are listed in Table 1.
| P | Patients, older than 18 years and in good general health, with partial or complete edentulism requiring placement of implant in either one or both the arches |
| I | Flapless implant placement |
| C | Conventional Flap elevation Implant placement |
| O | Primary outcomes was the survival rate of implant placement with flapless and flap elevation surgical approach |
| S | A combination of in vivo studies involving either or both the arches, comparative prospective randomized or Non-randomized clinical trials and retrospective studies were included |
Table 1: PICOS framework.
A total of 1372 patients with 2320 implants were included in the meta-analysis. The age of the patients ranged from 18 to 85 years. Follow up time ranged from minimum of 1 year to 9 years. Of the 23 included studies, 7 of the included studies have a long follow-up of 3 years or more. [7-22] In 10 of the included studies, flapless surgery was performed by guided approach [23-25] while remaining 13 were performed by the free hand approach. Six studies used soft tissue punch in the flapless technique while other 16 studies were performed by direct drill preparation through the soft tissue and in 1 study a crystal relief incision was used for implant placement. In 5 studies, implant placement was performed only in the mandibular jaw [26-35].
Information about loading time was also stated. In 5 studies, implants were loaded with immediate/early loading protocol after the placement for both the flapless and flap surgery groups [36]. Sixteen studies applied a conventional delayed loading protocol [37] whereas 2 studies [38] involved both immediate/early loading and delayed loading Figure 2 to Figure 4.
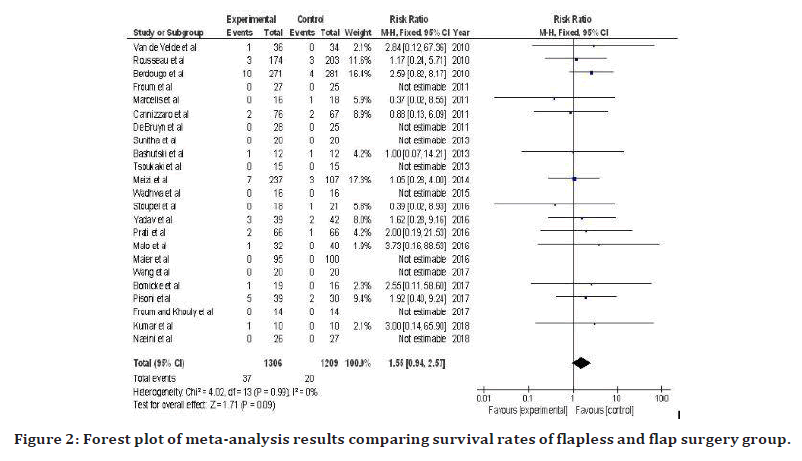
Figure 2. Forest plot of meta-analysis results comparing survival rates of flapless and flap surgery group.
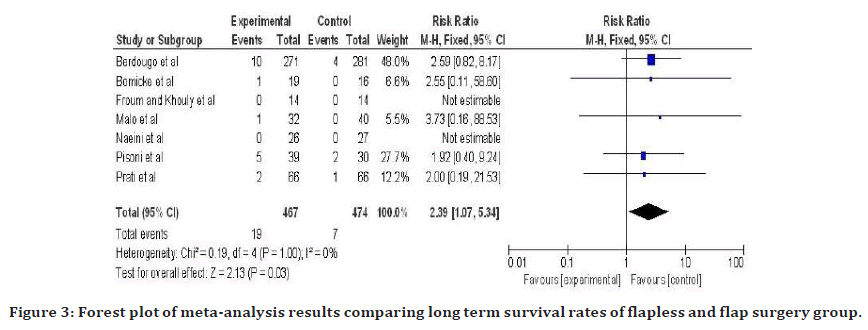
Figure 3. Forest plot of meta-analysis results comparing long term survival rates of flapless and flap surgery group.
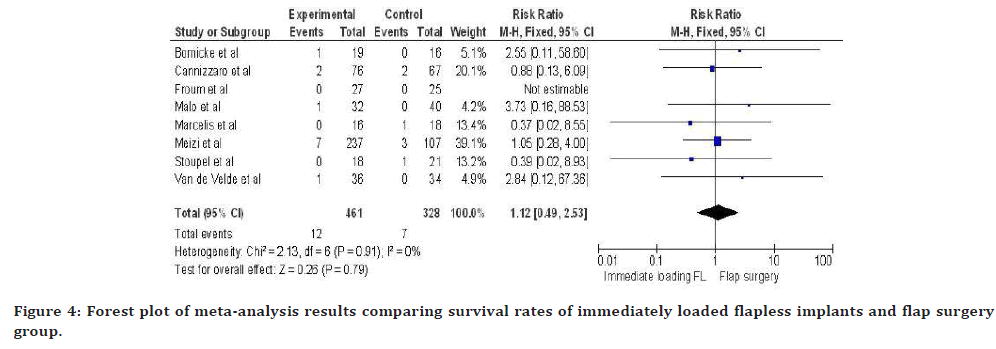
Figure 4. Forest plot of meta-analysis results comparing survival rates of immediately loaded flapless implants and flap surgery group.
Among the 23 studies, 1306 implants were placed through a flapless procedure with failure of 37 implants (2.8%) and 1209 implants were placed through a flapped procedure with failure of 20 implants (1.6%). Implant survival ranged from 87.2-100% for Flapless implant placement and 92–100% for flap elevation surgery.
No implant failure was found in 9 studies. All the articles included data regarding the implant survival rate and surgical technique used. None of the studies directly correlated the survival rates with the surgical technique used [39].
Quality Assessment
Quality assessment was done pertaining to the following aspects: random sequence generation, allocation concealment, blinding of outcome assessments, and incomplete outcome data. If all criteria were met, the study was considered to be at low risk of bias. The study was classified as having a high risk of bias if two or more criteria were not met. The assessment of each trial is summarized in Tables 2 and 3.
| Reference | Published Time | Study | Patients | Gender | Location | Flapless technique | Follow-up time | Age range(y) | Failed implants | Survival Rate | Loading time | Marginal bone loss | Implant surface modification(Brand) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Van de Velde, et al.[18] | 2010 | RCT | 13 patients | 9 females | All max posterior | Drill preparation | 18 mo | 39-75(55.7) | 1/36(T) | 97.2%(T) | Immediate | 1.95±0.7(T) | Sand blasted and acid-etched (SLA, Straumann, Basel, Switzerland) |
| 70 implants | 4 males | 0/34(C) | 100%(C) | 1.93±0.42(C) | ||||||||||
| 2 | Rousseau, et al. [25] | 2010 | R | 219 patients | 125 females | 49 max anterior; | Drill preparation | 2 yr | 23-84 | 3/174(T) | 98.3%(T) | Conventional | NM | Straumann Dental Implant |
| 377 implants | 93 males | 87 max post; | 3/203(C) | 98.5%(C) | System (Insitut Straumann, Basel, Switzerland). | |||||||||
| 4 mand ant; | sandblasted and acid etched | |||||||||||||
| 77 mand post | ||||||||||||||
| 3 | Berdougo, et al. [14] | 2010 | R | 169 patients | 111 females | 102 ant max; | Drill preparation | 4yr | 20-84 | 10/271(T) | 96.3%(T) | NM | NM | NM |
| 552 implants | 58 males | 215 max post; | 4/281(C) | 98.6%(C) | ||||||||||
| 29 mand ant; | ||||||||||||||
| 206 mand | ||||||||||||||
| 4 | Froum, et al. [20] | 2011 | P | 52 patients | 35 females | NM | Drill preparation | 12 mo | NM | 0/27(T) | 100%(T) | Early Loading | 0.25±1.02(T) | Oxidized(Noble Replace Select Tapered, Noble Biocare, Goteborg, Sweden) |
| 52 implants | 25 males | 0/25(C) | 100%(C) | 0.73±1.03(C) | ||||||||||
| 5 | Marcelis, et al. [15] | 2011 | P | 20 patients | NM | Both max and mand | Drill preparation | 1 yr | 48.7±16.4 | 0/16(T) | 100%(T) | Conventional | 0.06±0.12(T) | Sandblasted+Fluoride(Osseospeed, AstraTech, Sweden) |
| 20 implants | 1/18(C) | 94.4%(C) | 0.1±0.1(C) | |||||||||||
| 6 | Cannizzaro, et al. [4] | 2011 | RCT | 40 patients | 20 females | NM | Drill preparation | 1 yr | 22-65 | 2/76(T) | 97.3%(T) | Immediate | 0.38±0.42(T) | Sandblasted and Acid- NP etched((SwissPlus, |
| 143 implants | 20 males | 2/67(C) | 97%(C) | 0.43±0.4(C) | Zimmer Dental, | |||||||||
| Carlsbad, USA)) | ||||||||||||||
| 7 | De Bruyn, et a.l [26] | 2011 | P | 49 patients | 27 females | 26 max ant; | Drill preparation | 1-3 yrs | 20-79 | 0/28(T) | 100%(T) | NM | 1.4±0.8(T) | Porous anodized |
| 53 implants | 21 males | 16 max post; | 0/25(C) | 100%(C) | 1.27±1.1(C) | surface (TiUnite, | ||||||||
| 2 mand ant; | Nobel Biocare, | |||||||||||||
| 9 mand post | Goteborg, | |||||||||||||
| Sweden) | ||||||||||||||
| 8 | Sunitha, et al. | 2013 | P | 40 patients | 15 females | 18 max ant; | Drill preparation | 2 yrs | 25-62 | 0/20(T) | 100%(T) | Conventional | 0.09±0.02(T) | Root form implant with internal hex abutment connection system |
| 40 implants | 25 males | 10 max post; | 0/20(C) | 100%(C) | 0.47±0.4(C) | |||||||||
| 4 mand ant; | ||||||||||||||
| 8 mand post | ||||||||||||||
| 9 | Bashutski, et al. [16] | 2013 | RCT | 24 patients | 14 females | 5 max ant; | Punch | 15 mo | NM | 1/12(T) | 92%(T) | Conventional | NM | Micro-threaded, platform switching |
| 24 implants | 10 males | 19 max post | 1/12(C) | 92%(C) | implants with a fluoride-modified nanostructure surface | |||||||||
| 10 | Tsoukaki, et al. [28] | 2013 | RCT | 20 patients | 16 females | Both max and mand | Drill prepataion | 12 wks | 47.47±9.72(T) | 0/15(T) | 100%(T) | Conventional | 0.00±0.00(T) | Sandblasted+Fluoride(Osseospeed, AstraTech, Sweden) |
| 30 implants | 24 males | 0/15(C) | 100%(C) | 0.29±0.06(C) | ||||||||||
| 46.40±9.52(C) | ||||||||||||||
Table 2: Details of studies included in meta-analysis.
| Name | Published time | Sequence generation | Allocation concealment | Incomplete outcome data addressed | Blinding | Estimated potential risk of bias | |
|---|---|---|---|---|---|---|---|
| 1 | Van de Velde | 2010 | Yes | Adequate | Yes | Yes | Low |
| 2 | Rousseau | 2010 | Yes | Inadequate | No | No | High |
| 3 | Berdougo | 2010 | No | Inadequate | No | No | High |
| 4 | Froum | 2011 | Yes | Adequate | Yes | Unclear | Moderate |
| 5 | Marcelis | 2011 | No | Inadequate | Yes | No | High |
| 6 | Cannizzaro | 2011 | Yes | Adequate | Yes | Yes | Low |
| 7 | De Bruyn | 2011 | No | Inadequate | Yes | No | High |
| 8 | Sunitha | 2013 | Yes | Adequate | Yes | Yes | Low |
| 9 | Bashutski | 2013 | Yes | Adequate | Yes | Yes | Low |
| 10 | Tsoukaki | 2013 | Yes | Adequate | Yes | Yes | Low |
| 11 | Meizi | 2014 | Yes | Inadequate | No | No | High |
| 12 | Wadhwa | 2015 | Yes | Unclear | No | No | High |
| 13 | Stoupel | 2016 | Yes | Adequate | Yes | Yes | Low |
| 14 | Yadav | 2016 | Yes | Adequate | Yes | No | Moderate |
| 15 | Prati | 2016 | No | Inadequate | Yes | No | High |
| 16 | Malo | 2016 | No | Unclear | No | No | High |
| 17 | Maier | 2016 | Yes | Inadequate | Yes | No | High |
| 18 | Wang | 2017 | Yes | Adequate | Yes | Yes | Low |
| 19 | Bomicke | 2017 | Yes | Adequate | Yes | Yes | Low |
| 20 | Pisoni | 2017 | Yes | Adequate | Yes | Yes | Low |
| 21 | Froum and Khouly | 2017 | Yes | Unclear | Unclear | Yes | Moderate |
| 22 | Kumar | 2018 | Yes | Unclear | Yes | Unclear | Moderate |
| 23 | Naeini | 2018 | No | Inadequate | Yes | No | High |
Table 3: Results of quality assessment.
Among the 23 studies, 4 were judged to be at moderate risk of bias, [40-43] 9 were at low risk of bias.[44-45] and rest 10 were considered of high risk of bias Table 4.
| Reason for exclusion | References |
|---|---|
| No Control Group | Nikzad, et al. |
| Jeong, et al. | |
| Lee, et al. | |
| Tee | |
| Kareem, et al. | |
| Oliver, et al. | |
| Komiyama, et al. | |
| Altinci, et al. | |
| Review articles | Voulgarakis, et al. |
| Lin, et al. | |
| Chrcanovic, et al. | |
| Vohra, et al. | |
| Romero Ruiz, et al. | |
| Llamas-Monteagudo, et al. | |
| Zhuang, et al. | |
| Yadav, et al. | |
| Singh, et al. | |
| Cai, et al. | |
| Data inadequate for survival rate/ studies having other outcome measures | Danza, et al. |
| Pozzi, et al. | |
| Rana, et al. | |
| Jesch, et al. | |
| Kaur, et al. | |
| Follow uo period of less than 1 year | Arisan, et al. |
| Lindeboom, et al. | |
| Nickenig, et al. | |
| Al Juboori, et al. | |
| Katsoulis, et al. | |
| Mazzocco, et al. | |
| Kanwar, et al. | |
| Samad, et al. | |
| Shamsan, et al. | |
| Singla, et al. | |
| Gupta, et al. | |
| Divakar, et al. | |
| Anumala, et al | |
| Sun, et al. | |
| In vitro/ Animal studies | Jeong, et al. |
| Martinez, et al. |
Table 4: Summary of excluded articles.
Meta-analysis
For comparison of marginal bone loss between the two surgical approaches, 23 studies were included with 2320 implants placed in 1372 patients.
As statistically significant heterogeneity was (Chi2=4.02, df=13, p=0.99; I2=0%) not observed across the studies, a fixed effect model was carried out. In this study, failure rate of dental implants was affected by different insertion technique with a RR of 1.55 (flapless placement vs flap surgery; 95% CI: 0.94 to 2.57; P=0.09) indicating that failures in flapless procedure are 1.55 times likely to happen when compared with flapped procedure but the effect was not found to be statistically significant. Thus the relative risk reduction is -55% which indicates that flapless surgery has 55% more risk of implant failure. Since RR could be affected by risk of bias all the low bias studies were also pooled separately and RR of 1.35 resulted (295% CI: 0.55-3.35, P=0.51) which was not significant. Regarding the implant survival rate over the follow up period of three years or more, 7 studies were included in the meta-analysis. As low heterogeneity was found between the studies (Chi2=7.26, df=6, p=0.30; I2=0%), fixed effect model was carried out and forest plot was generated. The test of overall effect showed that the difference in implant survival rate between the 2 groups was statistically significant with a RR of 2.39(95% CI: 1.07 to 5.34; P= 0.03) indicating that in the studies with follow up of 3 or more years, flapless surgery has more failures compared to that seen with flap surgery. Meta-analysis of the immediate loading flapless surgery with flap surgery generated a fixed effect model based on the low heterogeneity (Chi2=2.13, df=13, p=0.91; I2=0%) with RR of 1.12 which was not statistically significant (95% CI: 0.49 to 2.53; P=0.79) indicating that immediately loaded implants placed with flapless technique have failure rates comparable to the flap surgery.
Publication bias
The funnel plot did not show asymmetry when the studies reporting the survival rate were analyzed indicating absence of publication bias. (Figures 5 to Figure 7).
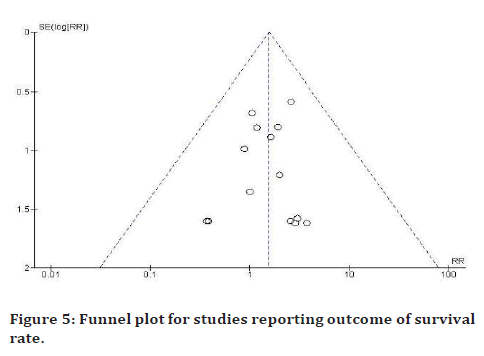
Figure 5. Funnel plot for studies reporting outcome of survival rate.
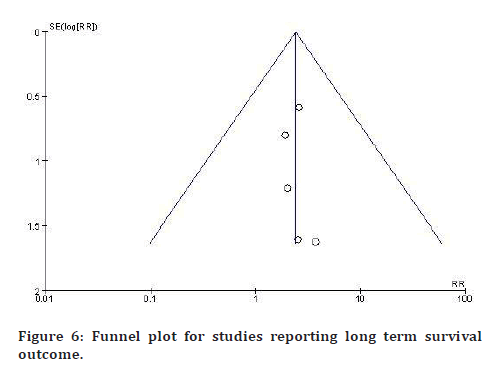
Figure 6. Funnel plot for studies reporting long term survival outcome.
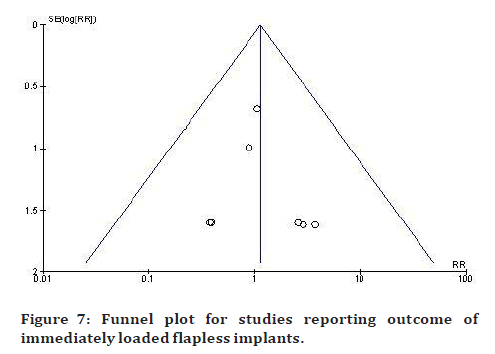
Figure 7. Funnel plot for studies reporting outcome of immediately loaded flapless implants.
Discussion
The current systematic review and meta-analysis compares the survival rates of the implants placed with flapless and flap surgery with extended evidence of the long term clinical performance and the effect of immediate loading of the placement technique.
Earlier reviews [46] provided controversial evidence regarding the flapless implant placement approach compared with flap elevation. Some studies [47] showed similar survival rates of the implants placed with the flapless as well as flap elevation approach while Chranovic et al and Zhuang et al found significant difference between the survival rates between the two approaches indicating that flapless implantation increased the risk of implant failure.
The implant prognostic criteria were previously described by Albrektsson and Zarb. Implants were considered successful if the following criteria were met: Absence of mobility, absence of paresthesia or pain, absence of peri-implant pathology or radiographic radiolucency’s, and marginal bone loss < 1mm during the first year and < 0.2mm/year in the following years. For the analysis of the implant survival minimum follow up period of 1 year was considered excluding the studies with follow up less than one year or unloaded implants. As the authors sought to eliminate the studies that followed participants for limited time, this systematic review can be considered to have robust data [48-50].
Evidence from total of 23 studies indicated that there was no significant difference between the implant survival rates of the two techniques which is in accordance with the previous review by Cai et al and Lin et al. In the present meta-analysis, it was identified that the that the risk of implant failure was 1.55 times higher in flapless implantation approach than the conventional flap elevation which is slightly less than the findings of Altinci et al [51] and Voulgarakis et al [52]. The findings showed that there is increased risk of failure in flapless placement of implants which could be attributed to this technique being a “blind” approach. Possible reasons of high implant failure in the flapless surgery may be interference in Osseo integration [53] and less accessibility due to poor vision. In recent studies computer guided flapless implantation are widely used to control the direction and depth of the implant. So the blind flapless approach can now be compared with the Conventional flap elevation technique if it is aided by the pre-operative three-dimensional planning. To maximize the treatment outcome it is important to correlate the restoratively driven implant position with the alveolar bone which can be achieved with the CT imaging and fabrication of surgical guides. As both the approaches have comparable effects with regard to the survival rates flapless surgery could be considered safe in patients having sufficient amount of alveolar bone and keratinized tissue. Three controlled studies, comparing guided flapless surgery with conventional open flap surgery and reporting on patient-centered outcomes [53-59] demonstrated a statistically significant reduction in immediate postoperative pain, use of analgesics, swelling, edema, hematoma, hemorrhage, and trismus when flapless guided surgery was performed. Chang et al in 2018 [60], evaluated the accuracy of implant placement with a computer-aided fabricated surgical template concluding that both the median of the linear deviation and angular deviation with surgical templates was in the clinically acceptable range.
The long term clinical performance was assessed by the meta-analysis of the studies having followed up time of 3 or more years. Seven studies were included with follow up ranging from 3 to 9 years. The result of the meta-analysis showed that implants placed with flapless approach are 1.51 times more likely to fail than with conventional approach which was found to be statistically significant. The technique used for flapless surgery could have influenced the outcome as earlier studies used free hand flapless approach without the 3D pretreatment planning and CT guided templates.
Flapless implantation surgeries are also known to have better patient acceptance because of the less discomfort and pain [61-65]. Campelo and Mazzocco, et al. [66] have concluded that patients that received flapless implants did not require any pain management. Cannizzaro, et al. concluded that flapless implant placement is associated with significantly less pain, post-surgical swelling and was more preferred by the patients. Boardman et al suggested that flapless procedure yielded higher pink esthetic scores [67-69]. Furthermore, flapless procedure can be beneficial to the health of the peri-implant soft tissue. Studies by Tsoukaki, You, Al-Juboori have found that flapless approach produced better values concerning probing depth, gingival index, BOP. Healthy peri-implant tissue will lead to better resistance to inflammation and bacterial invasion [70,73].
The original Branemark protocol required a two-stage surgery with a submerged healing period of at least 3 months in the mandible and 6 months in the maxilla, allowing the implant to Osseo integrate without exposure to external trauma. Under defined circumstances early or immediate loading are now deemed viable alternatives as it is assumed that immediate loading of implants may have positive biomechanical stimuli on the bone during healing enhancing biological fixation of implants. The ultimate goal is to reduce the number of surgical interventions and to shorten the treatment time, all without compromising the success of the implants. Immediate loading can be either functional occlusal loading or non-functional loading where the implant prosthesis is kept out of direct occlusal contact. Different from the results of the meta-analysis by Zhuang, et al. 2018, the current analysis did not establish a significant difference in the survival rates of the immediately loaded implants with the 2 techniques. The results showed that implants placed with flapless approach that are loaded immediately are 1.22 times more likely to encounter implant failure compared to flap elevation. As significant difference was not obtained both the procedures could be considered equally reliable when the implants are loaded immediately which is in agreement with several previous reports that have recommended flapless procedures to be used in immediately loaded implants [74,76].
However, it is not always possible to avoid reflection of flap for implant placement. Flapless approach cannot be performed when the bone is inadequate or in the presence of bone defects and bone grafting is required. Also, when there is a need for periodontal plastic surgeries or very less volume of soft tissue is available conventional flap elevation technique would provide for superior results. Few studies have also changed the technique while performing the implant placement as flapless placement could not be possible.
This systematic review provides enough evidence about flapless surgery being a possible alternative as it has comparable outcomes with the conventional procedure. The results of the studies should be interpreted with caution as few studies with high and moderate risk of bias were included as excluding these studies would exclude the data of significant value. Furthermore, success of implant therapy cannot be only defined according to the survival rates. Another shortcoming of the study is the inclusion of 2 retrospective studies and the nature of retrospective studies is inherently associated with flaws which are either manifested as gaps in information or incomplete data. The authors strongly believe that, for a more definitive conclusion double blinded high strength randomized controlled trials with greater sample are required. The use of CT guided templates with flapless approach and the use and efficacy of dynamic implant placement are still needed to be explored.
Conclusion
The overview of the selected studies indicated that both the approaches for implant placement have comparable survival rates irrespective of the technique used for placement loading protocol. Hence, flapless technique should be given consideration in patients whenever appropriate conditions pertaining to the alveolar bone and soft tissue are available.
References
- Albrektsson T, Brånemark PI, Hansson HA, et al. Osseointegrated titanium implants: Requirements for ensuring a long-lasting, direct bone-to-implant anchorage in man. Acta Orthop Scand 1981; 52:155-70.
- Aydemir CA, Arısan V. Accuracy of dental implant placement via dynamic navigation or the freehand method: a split‐mouth randomized controlled clinical trial. Clin Oral Implants Res 2020; 31:255-63.
- Arısan V, Karabuda CZ, Özdemir T. Implant surgery using bone‐and mucosa‐supported stereolithographic guides in totally edentulous jaws: surgical and post‐operative outcomes of computer‐aided vs. standard techniques. Clin Oral Implants Res 2010; 21:980-8.
- Cannizzaro G, Felice P, Leone M, et al. Flapless versus open flap implant surgery in partially edentulous patients subjected to immediate loading: 1-year results from a split-mouth randomised controlled trial. Eur J Oral Implantol 2011; 4:177-88.
- Sclar AG. Guidelines for flapless surgery. J Oral Maxillofac Surg 2007; 65:20-32.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010; 8:336-41.
- Berdougo M, Fortin T, Blanchet E, et al. Flapless implant surgery using an image‐guided system. A 1‐to 4‐year retrospective multicenter comparative clinical study. Clinical Implant Dentistry and Related Research. 2010; 12:142-52.
- Froum SJ, Khouly I. Survival Rates and Bone and Soft Tissue Level Changes Around One-Piece Dental Implants Placed with a Flapless or Flap Protocol: 8.5-Year Results. Int J Periodontics Restorative Dent 2017; 37.
- Prati C, Zamparini F, Scialabba VS, et al. A 3-Year Prospective Cohort Study on 132 Calcium Phosphate-Blasted Implants: Flap vs Flapless Technique. Int J Oral Maxillofac Implants. 2016; 31.
- Pisoni L, Ordesi P, Siervo P, et al. Flapless versus traditional dental implant surgery: Long-term evaluation of crestal bone resorption. J Oral Maxillofac Surg 2016; 74:1354-9.
- Naeini EN, Dierens M, Atashkadeh M, et al. Long‐term clinical outcome of single implants inserted flaplessly or conventionally. Clin Implant Dent Relat Res 2018; 20:829-37.
- Malo P, de Araújo Nobre M, Lopes A. Three‐Year Outcome of Fixed Partial Rehabilitations Supported by Implants Inserted with Flap or Flapless Surgical Techniques. J Prosthodont 2016; 25:357-63.
- Bömicke W, Gabbert O, Koob A, et al. Comparison of immediately loaded flapless-placed one-piece implants and flapped-placed conventionally loaded two-piece implants, both fitted with all-ceramic single crowns, in the posterior mandible: 3-year results from a randomised controlled pilot trial. Eur J Oral Implantol 2017;10.
- Berdougo M, Fortin T, Blanchet E, et al. Flapless implant surgery using an image‐guided system. A 1‐to 4‐year retrospective multicenter comparative clinical study. Clin Implant Dent Relat Res 2010; 12:142-52.
- Marcelis K, Vercruyssen M, Naert I, et al. Model‐based guided implant insertion for solitary tooth replacement: a pilot study. Clin Oral Implants Res 2012; 23:999-1003.
- Bashutski JD, Wang HL, Rudek I, et al. Effect of flapless surgery on single‐tooth implants in the esthetic zone: A randomized clinical trial. J Periodontol 2013; 84:1747-54.
- Maier FM. Initial Crestal Bone Loss After Implant Placement with Flapped or Flapless Surgery-A Prospective Cohort Study. Int J Oral Maxillofac Implants 2016; 31:876-83.
- Van de Velde T, Glor F, De Bruyn H. A model study on flapless implant placement by clinicians with a different experience level in implant surgery. Clin Oral Implants Res 2008; 19:66-72.
- Yadav R, Agrawal KK, Rao J, et al. Crestal bone loss under delayed loading of full thickness versus flapless surgically placed dental implants in controlled type 2 diabetic patients: a parallel group randomized clinical trial. J Prosthodont 2018; 27:611-7.
- Froum SJ, Cho SC, Elian N, et al. Survival rate of one-piece dental implants placed with a flapless or flap protocol--a randomized, controlled study: 12-month results. Int J Periodontics Restorative Dent 2011; 31.
- Wadhwa B, Jain V, Bhutia O, et al. Flapless versus open flap techniques of implant placement: a 15-month follow-up study. Indian J Dent Res 2015; 26:372.
- Kumar D, Sivaram G, Shivakumar B, et al. Comparative evaluation of soft and hard tissue changes following endosseous implant placement using flap and flapless techniques in the posterior edentulous areas of the mandible—a randomized controlled trial. Oral Maxillofac Surg. 2018; 22:215-23.
- Wang F, Huang W, Zhang Z, et al. Minimally invasive flapless vs. flapped approach for single implant placement: a 2‐year randomized controlled clinical trial. Clin Oral Implants Res 2017; 28:757-64.
- Stoupel J, Lee CT, Glick J, et al. Immediate implant placement and provisionalization in the aesthetic zone using a flapless or a flap‐involving approach: a randomized controlled trial. J Clin Periodontol. 2016; 43:1171-9.
- Rousseau P. Flapless and traditional dental implant surgery: an open, retrospective comparative study. J Oral Maxillofac Surg 2010; 68:2299-306.
- De Bruyn H, Atashkadeh M, Cosyn J, et al. Clinical outcome and bone preservation of single TiUnite™ implants installed with flapless or flap surgery. Clin Implant Dent Relat Res 2011; 13:175-83.
- Fortin T, Bosson JL, Isidori M, et al. Effect of flapless surgery on pain experienced in implant placement using an image-guided system. Int J Oral Maxillofac Implants 2006; 21.
- Tsoukaki M, Kalpidis CD, Sakellari D, et al. Clinical, radiographic, microbiological, and immunological outcomes of flapped vs. flapless dental implants: a prospective randomized controlled clinical trial. Clin Oral Implants Res 2013; 24:969-76.
- Meizi E, Meir M, Laster Z. New-design dental implants: a 1-year prospective clinical study of 344 consecutively placed implants comparing immediate loading versus delayed loading and flapless versus full-thickness flap. Int J Oral Maxillofac Implants 2014;29.
- Zhuang J, Zhao D, Wu Y, et al. Evaluation of outcomes of dental implants inserted by flapless or flapped procedure: A meta-analysis. Int J Implant Dent 2018;27:588-98.
- Lin GH, Chan HL, Bashutski JD, et al. The effect of flapless surgery on implant survival and marginal bone level: a systematic review and meta‐analysis. J Periodontol 2014; 85:e91-103.
- Cai H, Liang X, Sun DY, et al. Long-term clinical performance of flapless implant surgery compared to the conventional approach with flap elevation: A systematic review and meta-analysis. World J Clin Cases. 2020; 8:1087.
- Chrcanovic BR, Albrektsson T, Wennerberg A. Flapless versus conventional flapped dental implant surgery: a meta-analysis. PLoS One 2014; 9:e100624.
- Albrektsson T, Zarb G, Worthington P, et al. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int j oral maxillofac implants 1986; 1:11-25.
- Danza M, Carinci F. Flapless surgery and immediately loaded implants: a retrospective comparison between implantation with and without computer-assisted planned surgical stent. Stomatologija 2010; 12:35-41.
- Fortin T, Bosson JL, Isidori M, et al. Effect of flapless surgery on pain experienced in implant placement using an image-guided system. Int J Oral Maxillofac Implants 2006; 21.
- Nkenke E, Eitner S, Radespiel‐Tröger M, et al. Patient‐centred outcomes comparing transmucosal implant placement with an open approach in the maxilla: a prospective, non‐randomized pilot study. Clin Oral Implants Res 2007; 18:197-203.
- Chang RJ, Chen HL, Huang LG, et al. Accuracy of implant placement with a computer-aided fabricated surgical template with guided parallel pins: A pilot study. J Chin Med Assoc 2018; 81:970-6.
- Jané-Salas E, Roselló-LLabrés X, Jané-Pallí E, et al. Open flap versus flapless placement of dental implants. A randomized controlled pilot trial. Odontology 2018; 106:340-8.
- Campelo LD, Camara JR. Flapless implant surgery: a 10-year clinical retrospective analysis. Int J Oral Maxillofac Implants 2002; 17.
- Boardman N, Darby I, Chen S. A retrospective evaluation of aesthetic outcomes for single‐tooth implants in the anterior maxilla. Clin Oral Implants Res 2016; 27:443-51.
- You TM, Choi BH, Li J, et al. Morphogenesis of the peri-implant mucosa: a comparison between flap and flapless procedures in the canine mandible. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107:66-70.
- Al-Juboori MJ, Ab Rahman S, Hassan A, et al. What is the effect of initial implant position on the crestal bone level in flap and flapless technique during healing period? J Periodontal Implant Sci 2013; 43:153-9.
- Nikzad S, Azari A. Custom-made radiographic template, computed tomography, and computer-assisted flapless surgery for treatment planning in partial edentulous patients: a prospective 12-month study. J Oral Maxillofac Surg 2010; 68:1353-9.
- Jeong SM, Choi BH, Kim J, et al. A 1-year prospective clinical study of soft tissue conditions and marginal bone changes around dental implants after flapless implant surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011; 111:41-6.
- Lee DH, Choi BH, Jeong SM, et al. Effects of flapless implant surgery on soft tissue profiles: a prospective clinical study. Clin Implant Dent Relat Res 2011; 13:324-9.
- Tee YL. Minimally invasive surgical placements of nonsubmerged dental implants: a case series report, evaluation of the surgical technique and complications. J Oral Implantol 2011; 37.
- Kareem JJ, Al Garrawi HA, Badeia RA. A clinical assessment of periimplant marginal bone loss and soft tissue status in dental implant placed by flapless implant surgery (A one-year prospective study). MDJ 2012; 9:70-82.
- Oliver R. Flapless dental implant surgery may improve hard and soft tissue outcomes. J Evid Based Dent Pract 2012; 12:87-8.
- Komiyama A, Hultin M, Näsström K, et al. Soft tissue conditions and marginal bone changes around immediately loaded implants inserted in edentate jaws following computer guided treatment planning and flapless surgery: a≥ 1‐year clinical follow‐up study. Clin Implant Dent Relat Res 2012; 14:157-69.
- Altinci P, Can G, Gunes O, et al. Stability and marginal bone level changes of SLActive Titanium‐Zirconium implants placed with flapless surgery: A prospective pilot study. Clin Implant Dent Relat Res 2016; 18:1193-9.
- Voulgarakis A, Strub JR, Att W. Outcomes of implants placed with three different flapless surgical procedures: a systematic review. Int J Oral Maxillofac Surg 2014 ; 43:476-86.
- Vohra F, Al‐Kheraif AA, Almas K, et al. Comparison of crestal bone loss around dental implants placed in healed sites using flapped and flapless techniques: a systematic review. J Periodontol 2015; 86:185-91.
- Romero-Ruiz MM, Mosquera-Perez R, Gutierrez-Perez JL, et al. Flapless implant surgery: A review of the literature and 3 case reports. J Clin Exp Dent 2015; 7:e146.
- Llamas-Monteagudo O, Girbes-Ballester P, Vina-Almunia J, et al. Clinical parameters of implants placed in healed sites using flapped and flapless techniques: A systematic review. Med Oral Patol Oral Cir Bucal 2017; 22:e572.
- Yadav MK, Verma UP, Parikh H, et al. Minimally invasive transgingival implant therapy: A literature review. Natl j maxillofac surg 2018; 9:117.
- Singh K, Rao J, Afsheen T, et al. Survival rate of dental implant placement by conventional or flapless surgery in controlled type 2 diabetes mellitus patients: a systematic review. Indian J Dent Res 2019; 30:600.
- Danza M, Tortora P, Quaranta A, et al. Randomised study for the 1-year crestal bone maintenance around modified diameter implants with different loading protocols: a radiographic evaluation. Clin Oral Investig 2010; 14:417-26.
- Pozzi A, Tallarico M, Marchetti M, et al. Computer-guided versus free-hand placement of immediately loaded dental implants: 1-year post-loading results of a multicentre randomised controlled trial. Eur J Oral Implantol 2014; 7:229-42.
- Rana S, Verma A, Palwankar P, et al. Affect of flap and flapless implant placement on crestal bone level and implant stability.
- Jesch P, Jesch W, Bruckmoser E, et al. An up to 17‐year follow‐up retrospective analysis of a minimally invasive, flapless approach: 18 945 implants in 7783 patients. Clin Implant Dent Relat Res. 2018; 20:393-402.
- Lindeboom JA, Van Wijk AJ. A comparison of two implant techniques on patient‐based outcome measures: a report of flapless vs. conventional flapped implant placement. Clin Oral Implants Res 2010; 21:366-70.
- Nickenig HJ, Wichmann M, Schlegel KA, et al. Radiographic evaluation of marginal bone levels during healing period, adjacent to parallel‐screw cylinder implants inserted in the posterior zone of the jaws, placed with flapless surgery. Clin Oral Implants Res 2010; 21:1386-93.
- Katsoulis J, Avrampou M, Spycher C, et al. Comparison of implant stability by means of resonance frequency analysis for flapless and conventionally inserted implants. Clin Implant Dent Relat Res 2012; 14:915-23.
- Mazzocco F, Jimenez D, Barallat L, et al. Bone volume changes after immediate implant placement with or without flap elevation. Clin Oral Implants Res 2017; 28:495-501.
- Kanwar K, Madan R, Kanwar S, et al. Comparative evaluation of peri-implant vertical crestal bone changes following implant placement with'flapless' and'with-flap'techniques–In vivo study. Asian J Oral Health Allied Sci 2016; 6:3-8.
- Samad AA, Haider AA, Shihab OI. Comparison between flapless and flap dental implant surgery: A clinical and radiographic study. Zanco J Med Sci. 2016; 20:1267.
- Shamsan YA, Eldibany RM, El Halawani GN, et al. Flapless versus conventional flap approch for dental implant placement in the maxillary esthetic zone. Alex dent j 2018; 43:80-5.
- Singla N, Kumar S, Jain S, et al. Crestal Bone Changes around immediately loaded Single-piece Implants using Flap and Flapless Technique: A Radiographic Study. J Contemp Dent Pract 2018; 19:949-54.
- Gupta R, Luthra RP, Kukreja S. To compare and evaluate the difference in crestal bone loss after implant placement by conventional flap and flapless technique followed by early loading of implants: An in vivo study. Int J Appl Dent Sci 2018; 4:213-8.
- Divakar TK, Gidean Arularasan S, Baskaran M, et al. Clinical evaluation of placement of implant by flapless technique over conventional flap technique. J Maxillofac Oral Surg 2020; 19:74-84.
- Anumala D, Haritha M, Sailaja S, et al. Effect of flap and flapless implant surgical techniques on soft and hard tissue profile in single-stage dental implants. J Orofac Sci 2019; 11:11.
- Sun C, Zhao J, Liu Z, Tan L, et al. Comparing conventional flap‐less immediate implantation and socket‐shield technique for esthetic and clinical outcomes: a randomized clinical study. Clin Oral Implants Res 2020; 31:181-91.
- Jeong SM, Choi BH, Li J, et al. Flapless implant surgery: an experimental study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 104:24-8.
- Pérez‐Albacete Martínez C, Vlahović Z, Šćepanović M, et al. Submerged flapless technique vs. conventional flap approach for implant placement: experimental domestic pig study with 12‐month follow‐up. Clin Oral Implants Res 2016; 27:964-8.
- Sunitha RV, Sapthagiri E. Flapless implant surgery: a 2-year follow-up study of 40 implants. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116:e237-43.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at , Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Krishankumar Lahoti*, Sayali Dandekar, Jaykumar Gade, Megha J Agrawal, Minal N Soni and Karan V Jaiswal
Department of Prosthodontics, Swargiya Dadasaheb Kalmegh Smruti Dental College and Hospital, Nagpur, IndiaReceived: 05-Jan-2023, Manuscript No. jrmds-22-44173; Accepted: 07-Jan-2023, Pre QC No. jrmds-22-44173; Editor assigned: 07-Jan-2023, Pre QC No. jrmds-22-44173; Reviewed: 21-Jan-2023, QC No. jrmds-22-44173; Revised: 27-Jan-2023, Manuscript No. jrmds-22-44173; Published: 04-Feb-2023
