Research - (2022) Volume 10, Issue 6
Comparison of Different Types of Barriers Used in Non-Vital Bleaching: A Retrospective Study
*Correspondence: Pradeep S, Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences (SIMATS), India, Email:
Abstract
Introduction: Despite these excellent properties, GIC(Glass ionomer cements ) also possesses several undesirable characteristics such as long setting time, difficulties in manipulation and insertion, high costs, and potential of discoloration. In order to overcome these limitations, various alternative formulations have been developed. Aim: To compare and evaluate the root reinforcement potential of four different intraorifice barriers: resin-modified glass ionomer cement (RMGIC), and Glass ionomer cements,(GIC) Materials and Methods: The treatment records of patients who had undergone treatment in Saveetha Dental College between 2019 to 2021 were assessed for this study. The extracted data was tabulated in a spreadsheet (Excel 2017: Microsoft Office) and analysed using SPSS 19.0 version software (SPSS, Inc., Chicago). Descriptive statistics and chi-square tests were performed with the level of significance at 5% (P<0.05). Conclusion: Future development of the conventional bleaching agents by the addition of radical scavengers such as thiocarbamide or using sodium per carbonate is promising in terms of minimal penetration of hydrogen into the periodontal space.
Keywords
Endodontically treated teeth, Intra orifice barrier, Nanohybrid composite, Reinforcement
Introduction
The most common causes of dental discoloration are trauma, drugs, several genetic defects, decay, and also age. So to correct the discoloration of teeth with no pulp or damaged/necrosed pulp, internal bleaching is recommended. We can compare microleakage of several materials that are used for this purpose of bleaching such as resin modified glass ionomer and OrthoMTA used as an intraorifice barrier in non-vital bleaching [1].
Recent scientific progression has shown some evidence that the pH at the root surface is reduced due to intracoronal placement of bleaching pastes, which is actually enhancing osteoclastic activity. Hence, it is suggested that a protective barrier must be used over the canal filling to prevent leakage of the bleaching agents [2,3].
Traumatic injury to the anterior tooth is one of the main causes that mostly result in a non-vital tooth with discoloration. In the present era of aesthetic dentistry, bleaching of discolored teeth either vital or non-vital, has become popular [4]. It is considered a conservative clinical approach, where a chemical or bleaching agent is applied to the surface or the interior of the tooth. Non-vital or internal tooth-bleaching is used to lighten a discolored tooth that previously received root canal therapy [5].
Today’s market offers a variety of bleaching agents for tooth-whitening. Of these, sodium perborate, also called perboric acid, is the most trusted among dentists for use as an internal bleaching agent, due to excellent results and its respect for the periodontal tissues. “Walking bleach” technique, an internal bleaching procedure can be used for whitening of discolored root-filled teeth, which is mostly used among dental practitioners with good aesthetic results, safe and has good prognosis [6,7].
It is critical to maintain a coronal seal to prevent micro leakage into the canal space. The degree to which different temporary restorative materials are capable of establishing and maintaining a good coronal seal is questionable. Webber et al. reported that the sealing ability of temporary fillings decreased over time [6]. He showed that the least discoloration was seen in the control group with distilled water and that these tooth discolorations occurred even though the sealer does not penetrate into the dentinal tubules. Tooth discoloration following sealer application showed an increasing progression over twelve months in an in vitro trial.
Realizing this, permanent restorative materials (glass ionomer or composite resin) were placed as an additional layer beneath these intermediate restorative materials to seal the pulp chamber floor [6,8]. However, the pulp chamber often lacks adequate retention to prevent the dislodgement of the restorative material. It may be due to loss of depth due to caries or fracture of the coronal tooth structure [9].
A case report showed results about discoloration of hard dental tissues after the application of white MTA, so even with white MTA, discoloration occurs due to the iron oxidation process (tetracalcium aluminum ferrite) [10]. Although mineral trioxide aggregate (MTA) portrays very high biocompatibility, this material can very much lead to undesirable tooth discolorations in the aesthetic region of the dentition [6,10]. Depending on the situation, the walking bleach technique can be a less complicated methodology for both patients and dentists. In-office bleaching can mostly only produce short-term prognosis, majorly depending on the dehydration of the tooth. The risk of root resorption cannot be exactly determined [11]. Like this various studies have been done in our institutions [12-31]. The purpose of this study was to compare different types of barriers used in non-vital bleaching.
Materials and Methods
This is a retrospective study, conducted in a university setting. The study was approved by the institutional ethical committee. The ethical clearance for the study was obtained from the Institutional Scientific Review Board. The treatment records of patients who had undergone treatment in Saveetha Dental college between 2019 to 2021 were assessed for this study. 104 patients underwent non-vital leaching. Cross checking of data including digital entry and intraoral photographs was done by an additional reviewer, and as a measure to minimize sampling bias, samples for the group were picked by the simple random sampling method. Digital entry of clinical examination and intraoral photographs were assessed. The extracted data was tabulated in a spreadsheet (Excel 2017: Microsoft Office) and analysed using SPSS 19.0 version software (SPSS, Inc., Chicago). Descriptive statistics and chi-square tests were performed with the level of significance at 5% (P<0.05).
Results
Majority of the patients had used GIC as the barrier. 14.79% had used GIC as a barrier in the age group 10- 21. 60.56% had used GIC as a barrier in the age group 22-35. 14.08% had used GIC as a barrier in the age group 36-55, p value was found to be <0.05 resulting in GIC being commonly used as a gingival barrier in non-vital bleaching procedure (Figure 1). Majority of the patients had used GIC as the barrier. 24.65% of females used GIC as barrier in non-vital bleaching. 64.79% of male had used GIC as a barrier in non-vital bleaching, p value was found to be <0.05 resulting in GIC was commonly used as a gingival barrier in non-vital bleaching procedure (Figure 2).
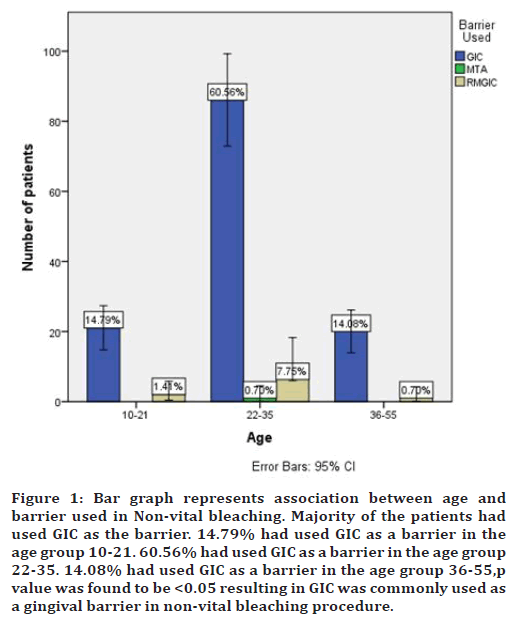
Figure 1. Bar graph represents association between age and barrier used in Non-vital bleaching. Majority of the patients had used GIC as the barrier. 14.79% had used GIC as a barrier in the age group 10-21. 60.56% had used GIC as a barrier in the age group 22-35. 14.08% had used GIC as a barrier in the age group 36-55,p value was found to be <0.05 resulting in GIC was commonly used as a gingival barrier in non-vital bleaching procedure.
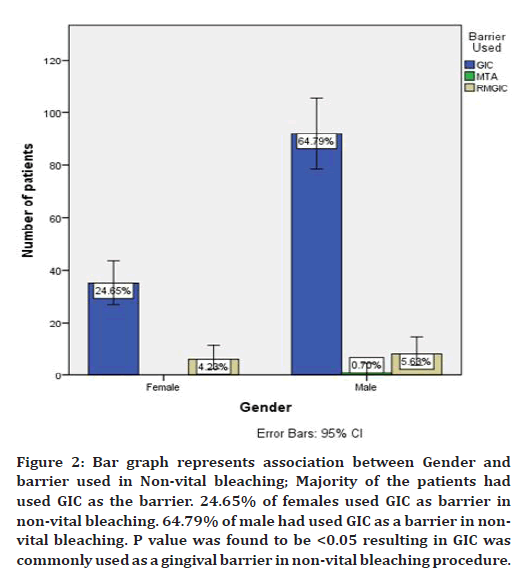
Figure 2. Bar graph represents association between Gender and barrier used in Non-vital bleaching; Majority of the patients had used GIC as the barrier. 24.65% of females used GIC as barrier in non-vital bleaching. 64.79% of male had used GIC as a barrier in nonvital bleaching. P value was found to be <0.05 resulting in GIC was commonly used as a gingival barrier in non-vital bleaching procedure.
Discussion
Much of the fracture susceptibility of endodontically treated teeth is intrinsic to the root canal morphology, dentin thickness, canal shape, and size and curvature of the external root; thus, special attention should be given for securing sufficient remaining dentin. However, enlargement of the coronal third of the root canal space is considered important to support root canal length measurement, debris removal, effective irrigation, and canal obturation [32].
Our results show that the highest age group among which non-vital bleaching was required by patients was between 15-25 years was 50 % and the least among the age group between 36-55 was 13.46 %. The management of dental trauma to immature permanent teeth in young children can be challenging. As a result of dental trauma, these teeth may become non-vital, which leads to arrested root development Root‑canal treatment at this time is a significant challenge.
In our results, when the association between Gender and barrier used in non-vital bleaching was done, the majority of the patients were males who had used GIC as the barrier. 24.65% of females used GIC as barrier in non-vital bleaching. 64.79% of male had used GIC as a barrier in non-vital bleaching. Fragile dentin walls and the large open apex. Apexification has long been the treatment of choice, enjoying considerable success in preserving traumatized nonvital immature teeth.Ca (OH)2 has been the material most frequently used to induce the formation of a calcified apical barrier in teeth with non-vital immature apices [33].
In our study, 60.56% of the majority of patients had used GIC as a barrier in the age group 22-35 and the least used material among the same age group was 0.7% MTA. This shows that the durability and preference was more for GIC among a larger group.
MTA provides a superior seal against microleakage when used as an intracanal medicament. Nagas et al. results of study also showed the lowest values for fracture resistance for MTA among all the tested groups [34].
Recently, a new calcium silicate‑based bio ceramic material, Bio Aggregate, has been introduced with the intention of preserving the properties and clinical applications of MTA without its negative characteristics. Bio Aggregate is composed of tricalcium silicate, dicalcium silicate, tantalum pent oxide, calcium phosphate monobasic, hydroxyapatite, and amorphous silicon dioxide
There are different options to treat discolored teeth such as restorative procedures, veneers and crowns. Actually, bleaching of non-vital teeth is a routine conservative approach to have a suitable esthetic result for endodontically treated teeth. Various methods to bleach non-vital teeth have been proposed [35,36]. Various materials have been used to achieve a coronal seal like cavit, intermediate restorative material, GIC, zinc oxide eugenol cement, resin modified GIC, compomer, composites and recently MTA. Each of these materials has their own benefits and limitations [37].
Analyzing the results in the present study, it has been observed that there was a statistically significant difference found among the groups tested. At this point, it would be interesting to compare the results obtained in the study with the results obtained in previous studies using these materials. There are very few studies available at present using the above materials as coronal sealants. The results of the study were compared with various other leakage studies using these materials, either alone or in combination [38,39]. Research in further laboratory study with different materials coupled with clinical trials is is important in future.
Conclusion
External bleaching of endodontically treated teeth using an in-office technique requires a very increased concentration gel. It might act as a complementing factor to the walking bleach technique, if the results are not satisfactory after 3–4 visits. As there have been known diagnosed discoloration of hard dental tissues after the application of white MTA, even with white MTA, discoloration occurs due to the iron oxidation process (tetra calcium aluminum ferrite). Therefore, it is important to always be aware of the possible complications and risks that are associated with the different bleaching techniques.
Acknowledgement
The authors are thankful to Saveetha Institute of Medical and Technical Sciences for providing a platform to express our knowledge.
Conflict of Interest
The author declares no conflict of interest.
Source of Funding
✓ The present study is sponsored by:
✓ Saveetha Institute of Medical and Technical Sciences, Saveetha Dental College and Hospitals, Saveetha University, India
✓ Soma beverages.
References
- Torabinejad M, Ung B, Kettering JD. In vitro bacterial penetration of coronally unsealed endodontically treated teeth. J Endod 1990; 16:566–569.
- Raina R, Loushine RJ, Weller RN, et al. Evaluation of the quality of the apical seal in Resilon/Epiphany and Gutta-Percha/AH Plus-filled root canals by using a fluid filtration approach. J Endod. 2007; 33:944–947.
- Caplan DJ, Weintraub JA. Factors related to loss of root canal filled teeth. J Public Health Dent 1997; 57:31–39.
- Valera MC, Camargo CHR, Carvalho CAT, et al. Effectiveness of carbamide peroxide and sodium perborate in non-vital discolored teeth. J Applied Oral Sci 2009; 17:254–261.
- Weiger R, Kuhn A, Löst C. In vitro comparison of various types of sodium perborate used for intracoronal bleaching of discolored teeth. J Endod 1994; 20:338–341.
- Torabinejad M, Walton RE, Fouad A. Endodontics: Principles and Practice. Elsevier Health Sciences 2008; 496.
- Swanson K, Madison S. An evaluation of coronal microleakage in endodontically treated teeth. Part I: Time periods. J Endod 1987; 13:56–59.
- Berman LH, Hargreaves KM, Cohen SR. Cohen’s pathways of the pulp expert consult-E-Book. Elsevier health sciences 2010; 992.
- Pisano DM, DiFiore PM, McClanahan SB, et al. Intraorifice sealing of gutta-percha obturated root canals to prevent coronal microleakage. J Endod 1998; 24:659–662.
- Baba NZ. Contemporary restoration of endodontically treated teeth: Evidence-based diagnosis and treatment planning. Quintessence Publishing Company 2013; 218.
- Tselnik M, Baumgartner JC, Marshall JG. Bacterial leakage with mineral trioxide aggregate or a resin-modified glass ionomer used as a coronal barrier. J Endod 2004; 30:782–784.
- Muthukrishnan L. Imminent antimicrobial bioink deploying cellulose, alginate, EPS and synthetic polymers for 3D bioprinting of tissue constructs. Carbohydr Polym 2021; 260:117774.
- PradeepKumar AR, Shemesh H, Nivedhitha MS, et al. Diagnosis of vertical root fractures by cone-beam computed tomography in root-filled teeth with confirmation by direct visualization: A systematic review and meta-analysis. J Endod 2021; 47:1198–1214.
- Chakraborty T, Jamal RF, Battineni G, et al. A review of prolonged post-COVID-19 symptoms and their implications on dental management. Int J Environ Res Public Health 2021; 18.
- Muthukrishnan L. Nanotechnology for cleaner leather production: A review. Environ Chem Lett 2021; 19:2527–2549.
- Teja KV, Ramesh S. Is a filled lateral canal-A sign of superiority? J Dent Sci 2020; 15:562.
- Narendran K, Sarvanan A. Synthesis, characterization, free radical scavenging and cytotoxic activities of phenylvilangin, a substituted dimer of embelin. Indian J Pharm Sci 2020; 82:909-912.
- Reddy P, Krithikadatta J, Srinivasan V, et al. Dental caries profile and associated risk factors among adolescent school children in an Urban South-Indian City. Oral Health Prev Dent 2020; 18:379–386.
- Sawant K, Pawar AM, Banga KS, et al. Dentinal microcracks after root canal instrumentation using instruments manufactured with different NiTi alloys and the saf system: A systematic review. Adv Sci Inst Ser E Appl Sci 2021; 11:4984.
- Bhavikatti SK, Karobari MI, Zainuddin SLA, et al. Investigating the antioxidant and cytocompatibility of mimusops Elengi linn extract over human gingival fibroblast cells. Int J Environ Res Public Health 2021; 18.
- Karobari MI, Basheer SN, Sayed FR, et al. An in vitro stereomicroscopic evaluation of bioactivity between neo MTA Plus, Pro Root MTA, Biodentine & glass ionomer cement using dye penetration method. Materials 2021; 14.
- Rohit Singh T, Ezhilarasan D. Ethanolic extract of Lagerstroemia Speciosa (L.) Pers., induces apoptosis and cell cycle arrest in HepG2 cells. Nutr Cancer 2020; 72:146–156.
- Ezhilarasan D. Micro RNA interplay between hepatic stellate cell quiescence and activation. Eur J Pharmacol 2020; 885:173507.
- Romera A, Peredpaya S, Shparyk Y, et al. Bevacizumab biosimilar BEVZ92 versus reference bevacizumab in combination with FOLFOX or FOLFIRI as first-line treatment for metastatic colorectal cancer: A multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol 2018; 3:845–855.
- Raj R K. β‐Sitosterol‐assisted silver nanoparticles activates Nrf2 and triggers mitochondrial apoptosis via oxidative stress in human hepatocellular cancer cell line. J Biomed Materials Res 2020; 108:1899-908.
- Vijayashree Priyadharsini J. In silico validation of the non-antibiotic drugs acetaminophen and ibuprofen as antibacterial agents against red complex pathogens. J Periodontol 2019; 90:1441–1448.
- Priyadharsini JV, Vijayashree Priyadharsini J, et al. In silico analysis of virulence genes in an emerging dental pathogen A. baumannii and related species. Arch Oral Biol 2018; 94:93–98.
- Uma Maheswari TN, Nivedhitha MS, Ramani P. Expression profile of salivary micro RNA-21 and 31 in oral potentially malignant disorders. Braz Oral Res 2020; 34:e002.
- Gudipaneni RK, Alam MK, Patil SR, et al. Measurement of the maximum occlusal bite force and its relation to the caries spectrum of first permanent molars in early permanent dentition. J Clin Pediatr Dent 2020; 44:423–428.
- Chaturvedula BB, Muthukrishnan A, Bhuvaraghan A, et al. Dens invaginatus: A review and orthodontic implications. Br Dent J 2021; 230:345–350.
- Kanniah P, Radhamani J, Chelliah P, et al. Green synthesis of multifaceted silver nanoparticles using the flower extract of Aerva lanata and evaluation of its biological and environmental applications. Chem Select 2020; 5:2322.
- Tuna EB, Dinçol ME, Gençay K, et al. Fracture resistance of immature teeth filled with Bio aggregate, mineral trioxide aggregate and calcium hydroxide. Dent Traumatol 2011; 27:174–178.
- Rafter M. Apexification: A review. Dent Traumatol 2005; 21:1–8.
- Nagas E, Uyanik O, Altundasar E, et al. Effect of different intraorifice barriers on the fracture resistance of roots obturated with Resilon or gutta-percha. J Endod 2010; 36:1061–1063.
- Gutmann JL. Contemporary perspective on root-end filling materials in surgical endodontics. Australian Endod Newsletter 2010; 16:15–7.
- Anthony JM. Comparative obturation techniques in the canine. J Veterinary Dent 1991; 8:24-29.
- Stock CJR, Gulabivala K, Walker RT. Color Atlas and Text of Endodontics. Mosby-Wolfe; 1995. 291 p.
- Kwon OH, Park SH. Evaluation of internal adaptation of dental adhesive restorations using micro-CT. Restorative Dent Endod 2012; 37:41-49.
- Johnson ME, Stewart GP, Nielsen CJ, et al. Evaluation of root reinforcement of endodontically treated teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90:360–364.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences (SIMATS), Chennai, IndiaReceived: 26-May-2022, Manuscript No. JRMDS-22-64999; , Pre QC No. JRMDS-22-64999 (PQ); Editor assigned: 28-May-2022, Pre QC No. JRMDS-22-64999 (PQ); Reviewed: 14-Jun-2022, QC No. JRMDS-22-64999; Revised: 17-Jun-2022, Manuscript No. JRMDS-22-64999 (R); Published: 24-Jun-2022
