Research - (2022) Volume 10, Issue 7
Comparison of Open versus Laparoscopic Appendectomy in Patients with Acute Appendicitis in Terms of Postoperative Complications
Awni Ismail Sultan1*, Sami Hassoon Ali2 and Mohammed Mohammud Habash3
*Correspondence: Awni Ismail Sultan, Department of surgery, College of Medicine, Tikrit University, Iraq, Email:
Abstract
Although laparoscopy in abdominal surgery is considered a gold standard, some surgeons still question its safety. Therefore, this study aims to compare potential postoperative complications of traditional open appendectomy versus laparoscopy in patients with acute appendicitis. This retrospective analysis was conducted for patients in Iraqi hospitals within the cities of Kirkuk and Jalawla from February 2020 and continued until May 2022. A total of 260 patients who underwent appendectomy were enrolled in 2 groups, the first for open surgery and the second for laparoscopic surgery. The basic characteristics of groups, the surgical approaches and their results (postoperative complications) were studied. The results proved that 140 (53.8%) patients had undergone open surgery versus 120 (46.2%) had undergone laparoscopy, and the majority of them were of the age group (18-30) years and they were females 46 (56.79%). The complication rates after open surgery were significantly higher in terms of surgical site infection (14.3%), paralytic ileus (5.0%) and abdominal abscess (1.9%) compared to the laparoscopic approach (6.5%, 0.8%, and 0.0% respectively). Thus, it has been concluded that laparoscopic appendectomy is a typical and safe surgical procedure.
Keywords
Appendectomy, Laparoscopy, Infection, Paralytic ileus, Abscess
Introduction
One of the main reasons for abdominal surgery is acute appendicitis, which can affect all ages, and is the most common abdominal emergency worldwide [1]. In general, open appendectomy (OA) has been considered the key standard in the remedy of acute appendicitis since it was described by Charles Mc Brney, et al. [2,3]. Besides, the German physician Semm, et al. performed the first laparoscopic appendectomy in 1983, and with the advent of laparoscopy, abdominal surgery has witnessed a remarkable improvement [4- 6]. Laparoscopic appendectomy (LA) has gained great popularity among surgeons since its inception, due to its many advantages such as minimal incisions, best view of the peritoneal cavity, safe reconnoitering, mild pain, and relatively quick recovery. Despite this, some of them remained skeptical about its safety and preference over open appendectomy [7,8]. It is worth noting, that cases of appendicitis are often an emergency and at odd hours when the laparoscopic equipment is not fully prepared and even the competent staff in all hospitals [9]. One of the main criticisms of laparoscopic appendectomy may be the costs involved in surgery for the use of single-use instruments, in addition to the possibility of some troublesome consequences after surgery [10,11]. Several studies have been conducted to compare the two surgical approaches to appendectomy, with conflicting results [12-14]. Therefore, we designed this comparative study to evaluate the post-operative consequences of conventional open appendectomy and laparoscopic surgery in acute appendicitis patients.
Methods
A retrospective analysis was conducted of 260 Iraqi patients diagnosed with acute appendicitis who underwent a surgical procedure for appendectomy (either laparoscopic or open) in the surgical and emergency surgery departments of hospitals in the cities of Kirkuk and Jalawla by surgeons with experience in open surgery as well as laparoscopic, for the extended period from February 2020 to May 2022. The approval of the Research Ethics Committee of the Directorate of Health of both cities was obtained. For all patients, before surgery, the necessary clinical and laboratory examinations were performed, in addition to an abdominal ultrasound to ensure the correct diagnosis, after obtaining the informed consent of each patient. The study included both genders, whose ages ranged from 18-50 years old. On the contrary, patients with no proven diagnosis, ages less than 18 years, who had undergone any previous abdominal surgery, who had coagulation disorders, contraindicated laparoscopic surgery, and who were not qualified for anesthesia, and pregnancy were excluded. The cases of appendectomy were separated into two groups; the first one was open appendectomy (OA), while the second group was laparoscopic appendectomy (LA). As for comparing patients between the two groups in this study, the variables included the characteristics of the patient (age and gender) and the time of the operation (from skin incision to wound closure). While the post-operative complications included the following: wound infection, paralytic ileus, and intra-abdominal abscesses. These complications were monitored by specialized health personnel, and all information was recorded. After data collection, statistical analysis was performed using SPSS program (version 26) descriptively and also in order to compare between the variables of the surgical groups. Appropriate parametric and non-parametric tests were used for specific differences between study variables, considering that a p-value of less than 0.05 is statistically significant.
Results
Of the total 260 patients, 140 (53.8%) of whom underwent a conventional open appendectomy (OA), while 120 (46.2%) of them underwent a laparoscopic (LA) procedure as shown in Figure 1. In general, no deaths were recorded during the study period. Among 260 patients, 126 (48.5%) were between (18-30) years old, compared to 134 (51.5%) aged between (31-50) years. It was noticed that the highest percentage of patients whose ages ranged between (18-30) years was in the laparoscopic surgery group (26.5%), while the highest percentage of patients whose ages ranged between (31-50) years was in the open surgery group (31.9%). There was a clear significant difference between them (p=0.007). As for the distribution of participating patients by gender, 106 (40.8%) patients were male and 154 (59.2%) were female. The highest proportion of females was recorded in the open group (35.8 %), while the highest proportion of males was in the laparoscopic group (22.7 %), with a clear significant difference (p=0.011) as presented in Table 1.
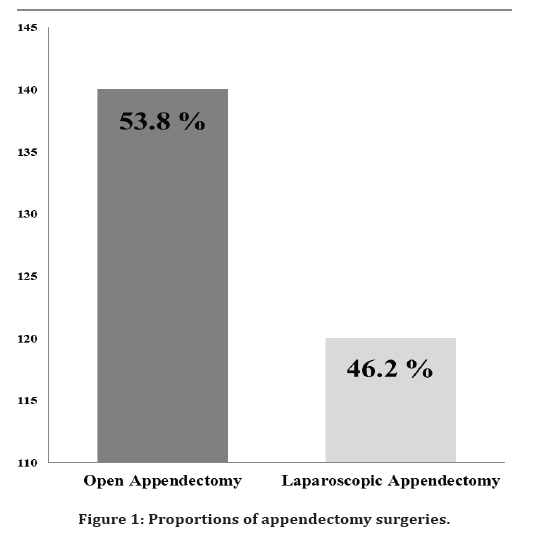
Figure 1. Surgical training questionnaire
| Basic variables | OA | LA | Total | P value | |
|---|---|---|---|---|---|
| N=140 (53.8%) | N=120 (46.2%) | N=260 (100%) | |||
| Age | 18-30 | 57 (21.9 %) | 69 (26.5 %) | 126 (48.5 %) | 0.007 |
| 31-50 | 83 (31.9 %) | 51 (19.6 %) | 134 (51.5 %) | ||
| Gender | Male | 47 (18.0 %) | 59 (22.7 %) | 106 (40.8 %) | 0.011 |
| Female | 93 (35.8 %) | 61 (23.5 %) | 154 (59.2 %) | ||
Table 1: Basic variables of patients and operation time between the two surgical groups.
As for the average operating time in both surgical groups, it was shorter in the laparoscopic surgery group (46.67 ± 3.57 minutes) than the open surgery group (51.11 ± 1.64 minutes) as shown in Table 2. 37 infection sites (14.3%), 13 paralytic ileus, and 5 (1.9%) abdominal abscesses were recorded in the open group versus 17 (6.5 %), 2 (0.8%), 0 (0.0 %), respectively in the laparoscopic group. Significant difference was seen in each postoperative complication between the two groups and the most of those complications were observed in the open group as shown in Table 3. The results proved that the majority of these postoperative complications occurred in patients whose ages ranged between (31-50) years and in females as illustrated in Table 4.
| Operating time (Mean ± SD) | OA | LA | P value |
| 51.11 ± 1.64 | 46.67 ± 3.57 | 0.001 |
Table 2: Operating time (minutes) for both surgical groups.
| Complications | OA | LA | Total | P value |
|---|---|---|---|---|
| N=140 (53.8%) | N=120 (46.2%) | N=260 (100%) | ||
| Site infection | 37 (14.3 %) | 17 (6.5 %) | 54 (20.8 %) | 0.015 |
| Paralytic ileus | 13 (5.0%) | 2 (0.8%) | 15 (5.8%) | 0.009 |
| Abdominal abscesses | 5 (1.9 %) | 0 (0.0 %) | 5 (1.9 %) | 0.037 |
Table 3: Postoperative complications for both surgical groups.
| Complications | Basic variables | OA | LA | Total | P value | |
|---|---|---|---|---|---|---|
| N=140 | N=120 | N=260 | ||||
| Site infection | Age | 18-30 | 6 (2.3 %) | 4 (1.5) | 10 (3.8 %) | 0.001 |
| 31-50 | 31(11.9 %) | 13 (5.0 %) | 44 (16.9 %) | |||
| Gender | Male | 5 (1.9 %) | 7 (2.7%) | 12 (4.6 %) | 0.002 | |
| Female | 32 (12.3 %) | 10 (3.9 %) | 42 (16.2 %) | |||
| Total | 37 (14.3 %) | 17 (6.5 %) | 54 (20.8 %) | |||
| Paralytic ileus | Age | 18-30 | 1 (0.4 %) | 0 (0.0 %) | 1 (0.4 %) | 0.001 |
| 31-50 | 12 (4.6 %) | 2 (0.8 %) | 14 (5.4 %) | |||
| Gender | Male | 3 (1.2 %) | 0 (0.0 %) | 3 (1.2 %) | 0.092 | |
| Female | 10 (0.8 %) | 2 (0.8 %) | 12 (4.6 %) | |||
| Total | 13 (5.0%) | 2 (0.8%) | 15 (5.8%) | |||
| Age | 18-30 | 0 (0.0 %) | 0 (0.0 %) | 0 (0.0 %) | 0.029 | |
| Abdominal abscesses | 31-50 | 5 (1.9 %) | 0 (0.0 %) | 5 (1.9 %) | ||
| Gender | Male | 1 (0.4 %) | 0 (0.0 %) | 1 (0.4 %) | 0. 340 | |
| Female | 4 (1.5 %) | 0 (0.0 %) | 4 (1.5 %) | |||
| Total | 5 (1.9 %) | 0 (0.0 %) | 5 (1.9 %) | |||
Table 4: Comparison post-operative complications by age and gender between groups.
Discussion
Since the 2000s, laparoscopic appendectomy has become increasingly popular in countries of the world, as it has proven to be more efficient than traditional open surgery [15]. However, it may be associated with a relatively increased risk of postoperative complications, especially in cases of complicated appendicitis [16]. The use of endoscopic appendectomy is mainly characterized by its effectiveness as a diagnostic tool, in addition to being a minimally invasive surgery that results in less postoperative pain, fewer problems and shorter recuperation period compared to open surgeries [17,18]. This study performed a retrospective analysis to compare the postoperative complications of both surgical methods of appendectomy. As for the operation time when comparing the two surgeries, LA was less than OA, which indicates the experience and skill of the surgeons, and that most of the surgical staff had performed advanced laparoscopic procedures [19]. Our findings are consistent with a recent study conducted by Nazir, et al. where they demonstrated that the mean operation time was (46.98 ± 2.99) minutes for laparoscopic appendectomy versus (53.02±2.88) minutes for open appendectomy [20]. In 2018, Shimoda, et al. conducted a clinical study of the results of both surgical approaches and found that the average operation time in the laparoscopic approach was less (61.5) than in the open approach (64) minutes [15]. According to our results, LA was performed for younger age groups more than older ones, and this may be explained by the fact that young ages are more susceptible to acute appendicitis [21]. This was supported by Chaitanya, et al. through their similar study, as they found that patients of the age group (21-30) years were more (42.8%) than the age group (31-40) years which reached (2.8%) in the laparoscopic appendectomy group [22]. In the same study, more female patients (57.1%) underwent appendectomy than males (42.8%), and this is similar to our result, as females were more than males. In our current study, postoperative complications (site infection, paralytic ileus, and abdominal abscesses) were significantly more observed in open appendectomy than in laparoscopic surgery, especially in older females. In a previous comparative study conducted by Kumar, et al. they demonstrated that post-operative complications in laparoscopic patients were the least and concluded that laparoscopic appendectomy is the most efficient and safe procedure and can be performed on all patients regardless of age and gender [17]. Also, a recent study conducted by Singh, et al. found that postoperative complications (wound infection and prolonged ileus) in the laparoscopic group were significantly less than the open approach [23].
Conclusion
Laparoscopic appendectomy may be adopted as the preferred approach in the treatment of acute appendicitis. It is characterized by minimal surgical intervention, as well as low complication rates depending on surgical experience. Thus, it is possible to advise patients with acute appendicitis to resort to it as a safe treatment.
References
- Van Dijk ST, Van Dijk AH, Dijkgraaf MG, et al. Meta-analysis of in-hospital delay before surgery as a risk factor for complications in patients with acute appendicitis. J Br Surg 2018; 105:933-945.
- Pattanshetti VM, Krishna KL. Conventional laparoscopic appendectomy versus double‐incision, three‐port laparoscopic appendectomy: A 1‐year randomized controlled trial. Asian J Endosc Surg 2018; 11:366-372.
- McBurney C. IV. The incision made in the abdominal wall in cases of appendicitis, with a description of a new method of operating. Ann Surg 1894; 20:38-43.
- Kliuchanok K, Keßler W, Partecke I, et al. A comparison of non-absorbable polymeric clips and staplers for laparoscopic appendiceal stump closure: Analysis of 618 adult patients. Langenbeck's Arch Surg 2019; 404:711-716.
- Sultan AI, Ali SH, Ghareeb OA. Port site consequences after laparoscopic cholecystectomy using an open versus closed approach of pneumoperitoneum. Cureus 2022; 14.
- Li Z, Zhao Q, Bai B, et al. Enhanced recovery after surgery programs for laparoscopic abdominal surgery: A systematic review and meta-analysis. World J Surg 2018; 42:3463-3473.
- Swank HA, Eshuis EJ, van Berge Henegouwen MI, et al. Short-and long-term results of open versus laparoscopic appendectomy. World J Surg 2011; 35:1221-1226.
- Kostov K. Analysis and evaluation of advantages from laparoscopic appendectomy. J IMAB 2022; 28:4183-4185.
- Chaitanya BV, Mallapragada RC. Comparative evaluation of laparoscopic with open appendectomy among patients of appendectomy-A prospective study. Int J Contemp Med Surg Radiol 2019; 4:18-22.
- Malhotra L, Pontarelli EM, Grinberg GG, et al. Cost analysis of laparoscopic appendectomy in a large integrated healthcare system. Surg Endosc 2022; 36:800-807.
- Wang D, Dong T, Shao Y, et al. Laparoscopy versus open appendectomy for elderly patients, a meta-analysis and systematic review. BMC Surg 2019; 19:1.
- Lee SH, Lee JY, Choi YY, et al. Laparoscopic appendectomy versus open appendectomy for suspected appendicitis during pregnancy: A systematic review and updated meta-analysis. BMC Surg 2019; 19:1-2.
- Poprom N, Wilasrusmee C, Attia J, et al. Comparison of postoperative complications between open and laparoscopic appendectomy: An umbrella review of systematic reviews and meta-analyses. J Trauma Acute Care Surg 2020; 89:813-820.
- Çelik Y, Erbil OA. Comparison of complications of open and laparoscopic appendectomy. LESS 2019; 26:5-10.
- Shimoda M, Maruyama T, Nishida K, et al. Comparison of clinical outcome of laparoscopic versus open appendectomy, single center experience. Heliyon 2018; 4:e00635.
- Pokala N, Sadhasivam S, Kiran R, et al. Complicated appendicitis–is the laparoscopic approach appropriate? A comparative study with the open approach: Outcome in a community hospital setting. Am Surg 2007; 73:737-742.
- Kumar GS, Lekkala S. Comparison of the complications between laparoscopic and open appendectomy: A study in a teaching hospital in Telangana, India. Int Surg J 2016; 3:1096-100.
- Shaikh AR, Sangrasi AK, Shaikh GA. Clinical outcomes of laparoscopic versus open appendectomy. JSLS 2009; 13:574.
- Maeda Y, Oiwa K, Matsumoto S, et al. Years of experience is more effective in defining experts in the gaze analysis of laparoscopic suturing task than task duration. Applied Ergon 2021; 96:103474.
- Nazir A, Farooqi SA, Chaudhary NA, et al. Comparison of open appendectomy and laparoscopic appendectomy in perforated appendicitis. Cureus 2019; 11.
- Spirt MJ. Complicated intra-abdominal infections: a focus on appendicitis and diverticulitis. Postgraduate Med 2010; 122:39-51.
- Chaitanya BV, Mallapragada RC. Comparative evaluation of laparoscopic with open appendectomy among patients of appendectomy-A prospective study. Int J Contemp Med Surg Radiol 2019; 4:18-22.
- Singh A, Sharma M, Abbas M. Laparoscopic versus open appendectomy: A comparative study. Int J Surg 2021; 5:325-330.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Awni Ismail Sultan1*, Sami Hassoon Ali2 and Mohammed Mohammud Habash3
1Department of surgery, College of Medicine, Tikrit University, Iraq2Jalawla General Hospital, Diyala Health Directorate, Iraq
3Department of Surgery, College of medicine, university of diyala, Iraq
Received: 21-Jun-2022, Manuscript No. JRMDS-22-69823; , Pre QC No. JRMDS-22-69823 (PQ); Editor assigned: 23-Jun-2022, Pre QC No. JRMDS-22-69823 (PQ); Reviewed: 08-Jul-2022, QC No. JRMDS-22-69823; Revised: 13-Jul-2022, Manuscript No. JRMDS-22-69823 (R); Published: 20-Jul-2022
