Research - (2022) Volume 10, Issue 12
Competence of Cauterization of Sphenopalatine Artery for Idiopathic Refractory Posterior Epistaxis
Tunjai Namiq Faiq1 and Ozdan Akram Ghareeb2*
*Correspondence: Ozdan Akram Ghareeb, Department of Community Health, Northern Technical University, Iraq, Email:
Abstract
Refractory posterior epistaxis requires cautery of sphenopalatine artery. The current study aimed to estimate the efficiency of cautery the sphenoid artery and to observe postoperative complications. This prospective clinical study of 200 consecutive adult patients with posterior epistaxis was conducted in a private specialized hospital and clinic in Kirkuk, northern Iraq, from the period from February 2019 to September 2021. The nasal cavity of each participant was carefully examined endoscopically to find out the location of the bleeding, and then determine the necessity of surgical intervention. A total of 200 cases of epistaxis were included, posterior epistaxis accounted for 12 (6%) of all epistaxis cases, and required cauterization of the sphenoid artery. According to the results, the success rate of all surgical cases was complete, as no serious complications were observed intra and post endoscopic cauterization, except for one case of numbness of the palate, which gradually disappeared during the first three months after the operation. Thus, we concluded that better success can be achieved by cautery of the sphenopalatine artery and it can be considered as the first-line for idiopathic posterior epistaxis.
Keywords
Sphenoid surgery, Cauterization, Nasal cavity, Epistaxis
Introduction
Epistaxis represents a great challenge for emergency departments, as it is one of the important postaccident emergency situations [1]. Although it is a common otolaryngological condition [2], nevertheless, posterior epistaxis is an uncommon [3]. It can be lifethreatening due to aspiration and hypotension as well as comorbidities. A small proportion of up to 15% of them requires hospitalization and will therefore need surgical intervention [4,5]. The majorities of cases of epistaxis, up to 90%, originate in the Kiesselbach area and are relatively easy to treat using chemical cautery or packing. However the minorities of cases, up to 10%, arise from the posterior nasal region and require more antagonistic closure or other interventions including endoscopic surgery [6-9]. Thus, the management of epistaxis ranges from simple self-treatment to critical interventions in emergency departments up to urgent surgeries [10,11]. Many cases can be treated and achieve hemostasis in outpatient clinics without the need for surgical intervention. However, there are some cases of recurrent epistaxis where the bleeding site is deep and difficult to manage [12,13]. In line with recent uprising in endoscopic nasality sinus surgery, endoscopic cauterization of the sphenopalatine artery is now used for posterior epistaxis [14]. Therefore, this study came to evaluate the efficacy of this surgical procedure for a group of patients suffering from idiopathic refractory posterior epistaxis.
Methods
In this prospective clinical study, a total of 200 cases of epistaxis were participated, attended the ENT clinic and privets hospital in Kirkuk, northern Iraq, from the period from February 2019 to September 2021. All the participants underwent a thorough examination of the nasal cavity with endoscopy to find out the location of the bleeding by the consultant physician Dr. Tunjai Namiq Faiq to determine the necessity of surgical intervention. The official approval has been obtained from the local health directorate in the province. Inclusion criteria were active posterior epistaxis, both genders, aged 18–65 years old, and reported consent to participate. In contrast, patients under the age of 18 years old, refused to participate, and those suffering from anterior epistaxis were excluded from the current study.
Surgical procedures
Endoscopic sphenopalatine artery cauterization was performed (Figure 1) according to the following steps:
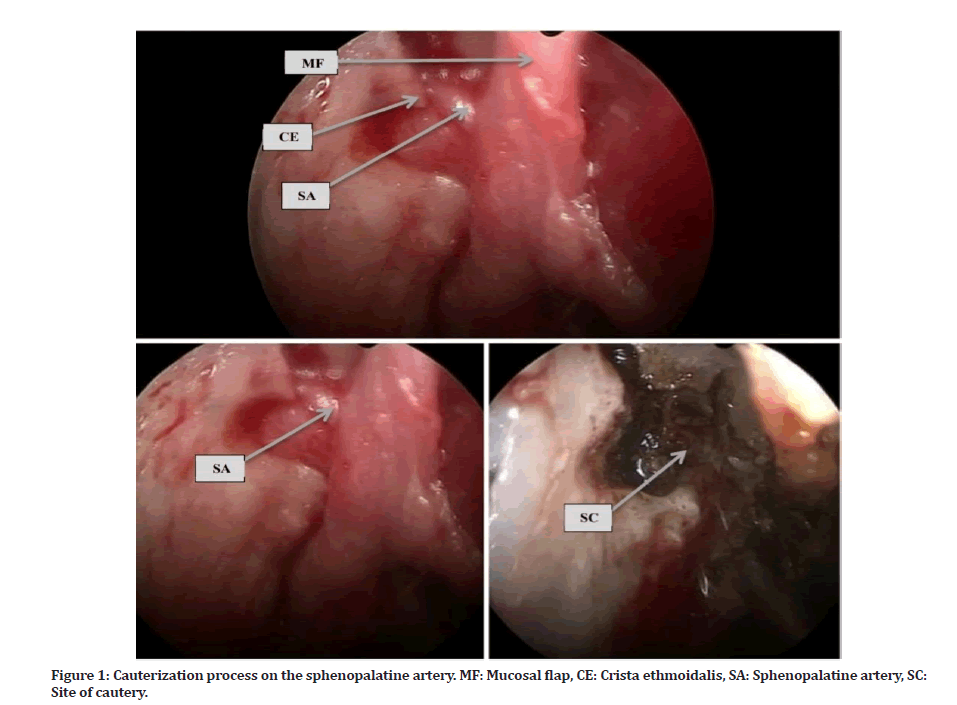
Figure 1: Cauterization process on the sphenopalatine artery. MF: Mucosal flap, CE: Crista ethmoidalis, SA: Sphenopalatine artery, SC: Site of cautery.
The procedure done under general anesthesia with cuff endotracheal tube and pharyngeal pack.
Patient should be in supine position with head elevated 15 degree and rotated towards the surgeon.
Draping must not close the eye.
Removed all nasal packs and irrigated the nasal cavity by warm normal saline solution.
Using ribbon gauze soaked in 2 ml of 1/1000 of adrenaline topical anesthesia was applied and inserted between the septum and inferior turbinate and in middle meatus.
All areas of nasal cavity were inspected to detect any bleeding point and to cauterize it.
Injected of local adrenaline 1/80000 at the attachment of middle turbinate on the lateral nasal wall.
Used Endoscope was 0 degree 18 cm ,4 ml diameter.
The middle turbinate has been gently medialized to open the field and should be gently mediated to prevent cerebrospinal fluid leakage.
The lateral nasal wall was palpated to find the posterior fontanelle, which is a mucosa-covered ostium located behind the uncinate process, under the ethmoid bullae and about 1 cm in front of where the middle turbinate attaches to the lateral nasal wall from behind. This defect must be seen clearly.
Vertical incision done the mucosa immediately posterior to this fontanelle and sub-mucosal has been dissected for about 1cm towards attachment of middle turbinate.
First structure to be encounter was crista ethmoidalis, and sphenopalatine artery located just posterior to it, we elevated mucosa to expose the foramen.
By using Kerrison punches we removed crista ethmoidalis and this step done gently in order not disrupt the artery.
After the artery was clearly identified, we cauterized the artery either by unipolar or bipolar and then the anterior branch was transect medially and superiorly to cauterize the other branches.
The mucosal flap was replaced with a surgical piece, so there was no need for anterior packing.
Each patient was observed for one day and discharged the next day.
Follow-up of these patients after endoscopic surgery continued for six months.
Data analysis
The results were statistically processed using SPSS software (IBM), version 26. The data was presented descriptively in the form of frequencies and percentages.
Results
The 200 participating patients consisted of 80 men (40%) and 120 women (60%) as shown in Figure 2, with an average age of 48.4 years old. Of the total 200 patients with epistaxis participated in the study, 12 (6%) patients with idiopathic posterior epistaxis required surgical intervention as display in Figure 3.
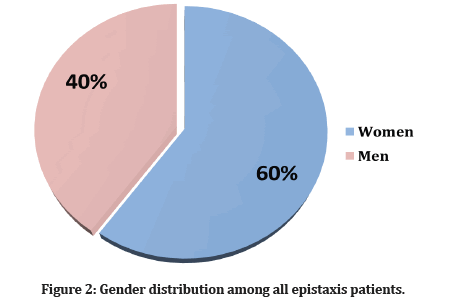
Figure 2: Gender distribution among all epistaxis patients.
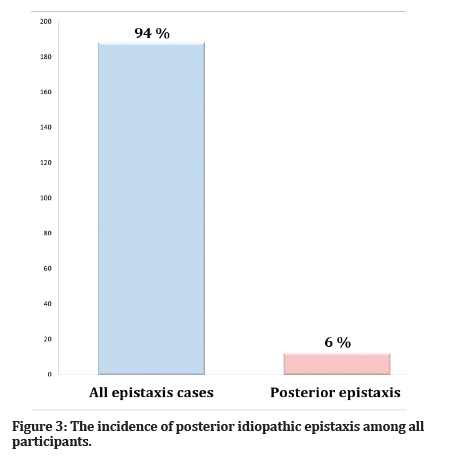
Figure 3:The incidence of posterior idiopathic epistaxis among all participants.
As shown in Table 1, the average age of patients undergoing unipolar cautery (group A) was about 48.8 years, compared to 48.2 years for the patients undergoing bipolar cauterization (group B). As for gender, the number of women in group (A) was 5 compared to 2 men. It was noted that the women in the group (B) amounted to 2 versus 3 men. The operation time lasted about 45 minutes, 7 patients needed a blood transfusion, 4 in unipolar cautery group (A) versus 3 in bipolar cautery group (B).Only 3 of the patients who underwent bipolar cautery had hypertension, and one patient had hypertension with diabetes mellitus. As for patients undergoing bipolar cautery, it was noted that only 2 of them had hypertension with diabetes. All patients had their nosebleeds controlled successfully and without noticeable complications during the six-month follow-up, except for one patient in unipolar cautery group had numbness of the palate in the first week after the operation, and it gradually improved spontaneously during the first 3 months after the operation.
| Variables | Unipolar surgical cautery Group A (N=7) | Bipolar surgical cautery Group B (N=5) | |
|---|---|---|---|
| Age (mean) | 48.8 | 48.2 | |
| Gender | Men | 2 | 3 |
| Women | 5 | 2 | |
| Require a blood transfusion | 4 | 3 | |
| Co-morbidities | Hypertension (HT) | 3 | 0 |
| Diabetes mellitus(DM) | 0 | 0 | |
| HT+ DM | 1 | 2 | |
| Non | 3 | 3 | |
| Palatal numbness | 1 | 0 | |
| Any other post-operative complications | 0 | 0 | |
Table 1: Comparison of unipolar and bipolar cautery groups of 12 patients.
Discussion
Accompanying the expansion of surgical technology, endoscopic sinus surgery has revolutionized the detection and treatment of sinus diseases [15,16]. Posterior epistaxis is generally difficult to manage, especially when it is recurring. There are non-surgical methods that have proven unsafe, unsuccessful and unsatisfactory results with detrimental complications [17,18]. Specifically in 1976, an endoscopic intranasal approach was used, in which the artery was ligated while accessing the Vidian nerve. It was found that this approach can freely access the sphenopalatine artery. This artery is the terminal branch of the internal maxillary arteriole which is the predominant exporter of caudal rhinal blood equipping [19,20]. However, the sphenopalatine artery ligation approach has proven to lead to major complications, including crusting of the nose [21]. Endoscopic cauterization of the sphenopalatine artery is a feasible technical surgical procedure that allows direct cauterization of the main vessel that supplies the posterior nasal cavity [22,23]. Our foundlings were supportive of other similar studies. In a previous study conducted by Gandomi, et al. on 27 patients underwent endoscopic cauterization in Shiraz, Iran. They found that endoscopic cauterization of the sphenopalatine artery can be considered an immediate treatment as a second alternative when conservative treatment is not successful [5].In other study conducted by Kitamura, et al. through a meta-analysis technique on 896 cases of sphenopalatine artery ligation or cautery for nose bleeding, they concluded that sphenopalatin surgery for refractory epistaxis is an effectiveness approach due to its low failure rates and less complications. The comparison between the two procedures showed that cauterization was more effective than ligation [24].
Conclusion
Endoscopic cautery of the sphenopalatin artery is a safe, rapid, and effectiveness procedure for the managing of posterior epistaxis without serious complications, thus may be recommended as a first choice for the treatment of idiopathic posterior epistaxis.
References
- Reis LR, Correia F, Castelhano L, et al. Epidemiology of epistaxis in the emergency department of a southern European tertiary care hospital. Acta Otorrinolaringologica 2018; 69:331-338.
- Iimura J, Hatano A, Ando Y, et al. Study of hemostasis procedures for posterior epistaxis. Auris Nasus Larynx 2016; 43:298-303.
- Dutta M, Haldar D. Optimizing the outcome of transnasal endoscopic sphenopalatine artery ligation in managing refractory posterior epistaxis: A case–control analysis. Auris Nasus Larynx 2017; 44:554-560.
- Krulewitz NA, Fix ML. Epistaxis. Emerg Med Clin 2019; 37:29-39.
- Gandomi B, Arzaghi MH, Khademi B, et al. Endoscopic cauterization of the sphenopalatine artery to control severe and recurrent posterior epistaxis. Iranian J Otorhinolaryngol 2013; 25:147.
- Hamlett KE, Yaneza MM, Grimmond N. Epistaxis. Surgery 2021; 39:577-90.
- Schmidtman DC, Blaseg NA, Likness MM. Recurrent epistaxis throughout the lifespan: A clinical review. South Dakota Med 2022; 75.
- Durmuş K, Altuntaş EE, Milkov M. Management of epistaxis. In all around the nose. Springer 2020; 415-429.
- McGarry GW. Epistaxis. In Scott-Brown’s otorhinolaryngology head and neck surgery. CRC Press 2018; 1169-1182.
- Tunkel DE, Anne S, Payne SC, et al. Clinical practice guideline: nosebleed (epistaxis). Otolaryngol Head Neck Surg 2020; 162:1-38.
- Buchs SR. 10 Epistaxis removal and nasal foreign body. Essential Clin Procedures E-Book 2020; 105.
- Yaneza MM, Amiraraghi N. Epistaxis. Surgery 2018; 36:543-552.
- Lou ZC. Hemostasis of idiopathic recurrent epistaxis in children with microwave ablation: A prospective pilot case series. J Otolaryngol Head Neck Surg 2019; 48:1-5.
- Meccariello G, Georgalas C, Montevecchi F, et al. Management of idiopathic epistaxis in adults: what’s new?. Acta Otorhinolaryngol Italica 2019; 39:211.
- Faiq TN, Ghareeb OA. Endoscopic management of orbital diseases of sinus origin: A case series. Ann Rom Soc Cell Biol 2021; 25:8755- 8761.
- Kim SD, Jeon H, Choi HY, et al. Successful treatment of optic neuropathy associated with sphenoid sinus aspergillosis. Ocul Immunol Inflamm 2022; 1-3.
- McClurg SW, Carrau R. Endoscopic management of posterior epistaxis: A review. ACTA Otorhinolaryngol Italica 2014; 34:1.
- McGarry GW. Epistaxis. In scott-brown’s otorhinolaryngology head and neck surgery. CRC Press 2018; 1169-1182.
- Almeida JP, de Andrade E, Reghin-Neto M, et al. From above and below: The microsurgical anatomy of endoscopic endonasal and transcranial microsurgical approaches to the parasellar region. World Neurosurg 2022; 159:e139-e160.
- Odat H, Al-Qudah M. Endoscopic monopolar cauterization of the sphenopalatine artery: A single surgeon’s experience. Ann Saudi Med 2016; 36:422-426.
- Eladl HM, Elmorsy SM, Khafagy YW. Endoscopic devascularisation of sphenopalatine bundle in intractable posterior epistaxis: Technique, efficacy and safety. J Laryngol Otol 2011; 125:1136-1140.
- Chitsuthipakorn W, Seresirikachorn K, Kanjanawasee D, et al. Endoscopic sphenopalatine foramen cauterization is an effective treatment modification of endoscopic sphenopalatine artery ligation for intractable posterior epistaxis. Eur Arch Oto Rhino Laryngol 2020; 277:2463.
- Karthik S. A study of management of recurrent and refractory posterior epistaxis by transnasal endoscopic sphenopalatine artery cauterization. Doctoral dissertation, Stanley Medical College, Chennai.
- Kitamura T, Takenaka Y, Takeda K, et al. Sphenopalatine artery surgery for refractory idiopathic epistaxis: Systematic review and meta‐analysis. Laryngoscope 2019; 129:1731-1736.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Tunjai Namiq Faiq1 and Ozdan Akram Ghareeb2*
1Department of Otolaryngology, Kirkuk General Hospital, Iraq2Department of Community Health, Northern Technical University, Iraq
Citation: Tunjai Namiq Faiq, Ozdan Akram Ghareeb, Competence of Cauterization of Sphenopalatine Artery for Idiopathic Refractory Posterior Epistaxis, J Res Med Dent Sci, 2022, 10 (12):24-27.
Received: 10-Nov-2022, Manuscript No. jrmds-22-76826; , Pre QC No. jrmds-22-76826(PQ); Editor assigned: 14-Nov-2022, Pre QC No. jrmds-22-76826(PQ); Reviewed: 28-Nov-2022, QC No. jrmds-22-76826(Q); Revised: 02-Dec-2022, Manuscript No. jrmds-22-76826(R); Published: 09-Dec-2022
