Research - (2022) Volume 10, Issue 9
Compliance with Short-Term Antibiotics in Riyadh, Saudi Arabia
Khalid A Bin Abdulrahman1*, Ali M Alaseem2, Rayan A Bahmaid1, Mohammed M Alharbi1, Mohammed N Almutairi1 and Haitham A Alghufaily1
*Correspondence: Khalid A Bin Abdulrahman, Department of medical education, College of Medicine, Imam Mohammad Ibn Saud Islamic University, Riyadh, Saudi Arabia, Email:
Abstract
Background: Short-term antibiotics (ST-AB) are commonly prescribed for treating various bacterial infections. However, adherence to ST-AB and the subsequent potential development of microbial resistance are emerging global concerns. In this research, we proposed investigating the aspects associated with commitment to ST-AB in Riyadh, Saudi Arabia. We hypothesized that multiple contributing factors such as level of education, age, and appropriate medical education are positively correlated with adherence to ST-AB. Method: A cross-sectional study was conducted in Riyadh, Saudi Arabia. An online self-administered questionnaire was provided to assess the research question. Our data were collected from adult and elderly patients who used the ST-AB for six months. Results: Out of 525 participants surveyed, 393 (75%) were eligible for the research. Around 65% of the participants completed their course of A.B. regardless of their gender, age, or education level. A statistically significant correlation was found between age and completing the antibiotic treatment ( p-value = 0.0002 ). Likewise, a positive correlation was found between gender and completing the antibiotic treatment ( p-value = 0.01 ). Meanwhile, education level has not been shown to improve ST-AB adherence. Finally, the female had a compliance rate of 38.93%, whereas the male had a 25.95% compliance rate. Conclusion: Regardless of high knowledge of antibiotic resistance, patients have the wrong concept of antibiotics. Therefore, non-compliance with antibiotic treatment was frequent in the community. The primary factor linked to the non-adherence was feeling better of the patient. The findings of our study suggest that adherence to ST-AB requires more A.B. informative patient education.
Keywords
Antibiotic treatment, Short-term antibiotics, Patient compliance, Saudi Arabia
Introduction
Antibiotics consider the most common medication used worldwide. It is an antimicrobial medication used to fight bacterial infections by killing or inhibiting the growth of the bacteria. Different families of antibiotics have other mechanisms of action; some are classified as bacteriostatic drugs, which arrest and stop bacterial growth and limit the spread of the infection [1–3]. On the other hand, Bactericidal drugstores selectively kill the bacteria through various mechanisms of action p[4]. Antibiotics have undesirable side effects such as G.I. disturbance or CNS-related complications. Such adverse effects are associated with a high rate of non-compliance with antibiotics treatment [5,6]. Antibiotics were frequently prescribed to patients with upper respiratory tract infection (URTI, followed by urinary tract infection at 36.13% and 7.63% of total participants, respectively) [7].
Adherence to antibiotics is a critical aspect of achieving optimal therapeutic benefits. Non-adherence to antibiotics could lead to bacterial resistance and increase the susceptibility to developing bacterial infection resistance [8,9]. Therefore, non-compliance to antibiotics is strongly associated with treatment failure, which may lead to deterioration of individuals' health, increased doctor visits and hospital admission, and absenteeism of the employees or students [10–13].
Feeling better or forgetting to take the antibiotics accounted for 65% of patients who had not completed the course [14]. Lack of knowledge about antibiotics and educational level were associated with non-adherence behavior [15]. Antibiotic-resistant is being highlighted as an emerging problem developed primarily by the inappropriate use of antibiotics. The devolvement of bacterial-resistant strains may put an extra financial burden on the healthcare system and individuals [16].
This study aimed to investigate and discuss the factors and prevalence associated with antibiotic nonadherence. We hypothesized that multiple contributing factors such as level of education, age, and appropriate medical education are associated with adherence to antibiotics.
Methods
Study design
A cross-sectional study was undertaken in Riyadh city, the capital of Saudi Arabia.
Study population and sampling
The authors were able to acquire the contact information of people aged 18 years and older through the official government Saudi Telecom database, which clearly explained that the communication with them was purely for scientific purposes. All data on their identities would remain confidential. A systematic random sampling of randomly selected participants from different parts of Riyadh was applied using a computer generating system to ensure it represents the whole city. The sample size was estimated to be 362 with a 95% confidence level and a 5% margin of error.
Study questionnaire
The Survey Monkey program was used to have a more straightforward presentation of the questions to the participant. The researcher first started by calling each participant. Each point of the questionnaire was explained to them to ensure they had excellent comprehension and, therefore, responded accurately. A full explanation was given to each participant in detail (from the purpose of the research, consent to answer the questionnaire, and explanation of the outcome definition).
The study questionnaire was created from other questionnaires and summarized to be more specific to answer the study hypothesis. The questionnaire contained 19 closed-ended questions related to factors potentially affecting adherence to ST-AB., plus eight demographic variables.
Statistical analysis
The collected data was cleaned, entered, and analyzed using Statistical Package for the Social Sciences (SPSS) software version 23. Descriptive statistics (i.e., frequencies, percentages, and measures of central tendency and dispersion where appropriate) were calculated for each item in the survey and all demographic variables. Means with standard deviations (±SD) for continuous variables and proportions for discrete variables were utilized. A P-value less than 0.05 is considered statically significant.
Results
Out of 525 participants surveyed, 393 (75%) were eligible for the research. Table 1 shows the sociodemographic data of the study population.
| Variable | Numbers | |
|---|---|---|
| Gander | Male | 175(44.53%) |
| Female | 218 (55.47%) | |
| Age | 18-29 | 230(58.52%) |
| 30-39 | 75(19.08%) | |
| 40-54 | 71(18.07%) | |
| >55 | 17(4.33%) | |
| Social status | Single | 217(55.22%) |
| Married | 168(42.75%) | |
| Divorced | 8(2.03%)) | |
| Education level | Academic level | 281(71.50%) |
| High school | 77(19.59%) | |
| Postgraduate | 31(7.89%) | |
| Ungraduated | 4(1.02%) | |
| In medical field | Yes | 139(35.37%) |
| No | 254(64.63%) |
Table 1: Demographic data of study population (n=393).
Table 2 shows a statistically significant correlation between age and completing the antibiotic treatment as directed by prescribers. There was no significant difference between educational levels regarding compliance rates. However, a statistically significant correlation between gender and compliance. Overall, females have a compliance rate of 38.93%, whereas males have a 25.95% compliance rate.
| Variable | Completed Treatment (%) | Didn’t Complete Treatment (%) | X2 | p-value |
|---|---|---|---|---|
| Age | ||||
| 18-29 | 130(33.1) | 100(25.4) | 19.2 | <0.001** |
| 30-39 | 61(15.5) | 14(3.6) | ||
| 40-55 | 50(12.7) | 21(5.3) | ||
| >55 | 14(3.6) | 3(0.8) | ||
| Gender | ||||
| Male | 102(26.0) | 73(18.6) | 5.52 | 0.010* |
| Female | 153(38.9) | 65(16.5) | ||
| Social Status | ||||
| Single | 122(31.1) | 95(24.2) | 15.97 | <0.001** |
| Married | 127(32.3) | 41(10.4) | ||
| Divorced | 6(1.5) | 2(0.5) | ||
| Education Level | ||||
| Uneducated | 2(0.5) | 2(0.5) | 1.65 | 0.65 |
| High School | 49(12.5) | 28(7.1) | ||
| Academic Level | 181(46.1) | 100(25.4) | ||
| Postgraduate | 23(5.9) | 8(2.0) | ||
| Health Field | ||||
| Yes | 88(22.4) | 51(13) | 0.14 | 0.71 |
| No | 167(42.5) | 87(22.1) | ||
| Health Insurance | ||||
| Yes | 94(23.9) | 48(12.2) | 0.09 | 0.76 |
| No | 161(41.0) | 90(22.9) | ||
| Income | ||||
| <3,000 | 116(29.5) | 84(21.4) | 8.91 | 0.03* |
| 3,000-10,000 | 51(13) | 22(5.6) | ||
| 10,000-20,000 | 65(16.5) | 25(6.4) | ||
| >20,000 | 23(5.9) | 7(1.7) | ||
| Location | ||||
| Riyadh | 255(64.9) | 138(35.1) | NA | NA |
| Other | 0 | 0 | ||
Table 2: Correlation between age, gender, education level, and compliance with antibiotic treatment N=393 (compliance).
Out of 393 participants (138; 35.11%) did not meet their A.B. course, whereas (255; 64.89%) completed the treatment course. Improvement of the symptoms (22%) was considered the most reported cause of not completing the treatment (Table 3).
| Answer/Cause | ||
|---|---|---|
| Yes | No | |
| Feeling better | 87(22.14%) | 306(77.86%) |
| Length of the treatment plan | 15(3.82%) | 378(96.18%) |
| I take a lot of medication | 6(1.53%) | 387(98.47%) |
| I forgot to take the medication | 49(12.47%) | 344(87.53%) |
| Times of taking the drug were a lot | 21(5.34%) | 372(94.66%) |
| Side effect | 15(3.82%) | 378(96.18%) |
| Other | 6(1.53%) | 387(98.47%) |
| Completed the course | 255(64.89%) | 138(35.11%) |
Table 3: Reasons that prevented patients from completing their period mentioned for treatment?.
Regardless of the participant's educational level, more than half (53.43%) believe antibiotics might treat bacterial and viral infections (Figure 1). Almost twofifths of the participants (39.19%) did not hear or read about the bacteria resistance of A.B (Figure 2).
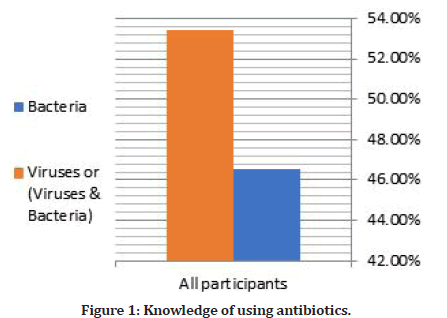
Figure 1: Knowledge of using antibiotics.
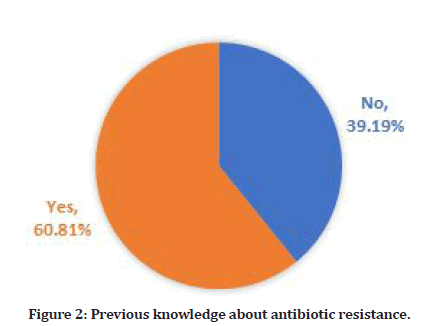
Figure 2: Previous knowledge about antibiotic resistance.
Discussion
The prevalence of short-term antibiotic compliance in Saudi Arabia information recourses is limited. Our study shows that the prevalence of short-term antibiotic compliance was moderate at 64.89%. This finding was close to (67.8%) of a previous study conducted in primary care centers in Riyadh [17]. However, the compliance was higher in our study than in the one conducted in Lisbon, Portugal, which shows only 42.3% of participants were [18].
Multiple reasons may cause non-compliance to the treatment and course of antibiotics. Feeling better got on the top of the list, followed by forgetting. Length of antibiotics treatment course has been a significant contributor to ST-AB non-compliance in our study, as every additional day gives 28% more chance to be noncompliance [13,17–22]. Inversely, our study showed that only 3.82% of the participants stopped their medication because of the long duration of the course of the treatment, which represents a small number of people whose compliance get affected by the length of the course [18]. Frequent doses for the patient can affect compliance, as those who take three doses are less compliant than patients with one or two doses a day [1,20]. In our study, around 5% of the participants attributed non-adherence to the antibiotics to the frequent times taking them.
Age has been linked to the compliance rate, as increased age was associated with less risk of non-compliance to the course of treatment and less compliance with younger people [13,18]. Inversely, our study's overall compliance rate is the highest among people between 18 and 30 years old (33.08%) and decreases as they age (3.56% for people over 55 years old). There was no significant difference between educational levels regarding compliance rates in our study. However, in another study, a substantial difference has been shown in the knowledge and usage of antibiotics between patients whose educational level is lower than a university degree and whose degree is higher than [15]. It is not surprising that we found a discrepancy in the current study results compared to other studies due to the variation in the variables and disease states experienced by the participants in this study and previous studies. However, most studies have similar factors related to patients' adherence to treatment duration. The less the course and the fewer doses per day, and the absence of side effects that prevent the patient from completing his treatment make the commitment more significant according to the instructions of his treating physician [10,12,14,15,17–27].
There is an essential factor associated with the diagnosis of the disease and its effects on the patient's activity and daily life. There is no doubt that some patients who suffer from acute inflammation of the middle ear affect their daily activity, which increases their eagerness to take antibiotics and other painkillers because of their positive impact on their return to their everyday life. On the other hand, the educational level of the patient and his advanced age increase his awareness of the importance of commitment.
Conclusion
Non-compliance with antibiotic treatment was found to be frequent in the community. The primary factor linked to the non-adherence was feeling better of the patient. The findings of our study suggest that adherence to ST AB requires more A.B. informative patient education.
Limitation
We accept that the study adopted a cross-sectional design, and patients asked for recall for used A.B. in the past six months or more. However, this may lead to recall bias due to the long-time interval between using A.B. and filling the survey. Furthermore, we only focus on Short- Term AB excluding the long ones.
Author Contributions
All authors participated in the study concept and design, analysis and interpretation of data, drafting and revising the paper, and have seen and approved the final version of the manuscript.
Availability of Data and Materials
All data supporting the study findings are contained within this manuscript.
Funding
The authors report no funding.
Conflict of Interests
The authors declare that they have no conflict of interest.
Ethical Consideration
The institutional review board approved the study at Imam Mohammad Ibn Saud Islamic University (project number 42-2019; approval date, 05 March 2019). All writing is done following the ethical principles of the declaration of Helsinki. A brief description of the study was included with the survey link, with a full explanation on the survey's front page. Participants were told consent was given by filling out the survey. Throughout the study, consent of all participants and data were gathered in complete confidence.
References
- Kardas P, Devine S, Golembesky A, et al. A systematic review and meta-analysis of misuse of antibiotic therapies in the community. Int J Antimicrob Agents 2005; 26:106-113.
- Barker AK, Brown K, Ahsan M, et al. Social determinants of antibiotic misuse: A qualitative study of community members in Haryana, India. BMC Public Health 2017; 17:333.
- Nepal G, Bhatta S. Self-medication with antibiotics in WHO Southeast Asian region: A systematic review. Cureus 2018;10:e2428.
- Kohanski MA, Dwyer DJ, Collins JJ. How antibiotics kill bacteria: From targets to networks. Nat Rev Microbiol 2010; 8:423-435.
- Grill MF, Maganti RK. Neurotoxic effects associated with antibiotic use: management considerations. Br J Clin Pharmacol 2011; 72:381-393.
- Hurkacz M, Dobrek L, Wiela-Hojeńska A. Antibiotics and the nervous system—Which face of antibiotic therapy is real, Dr. Jekyll (Neurotoxicity) or Mr. Hyde (Neuroprotection)? Molecules 2021; 26:7456.
- Panasiuk L, Lukas W, Paprzycki P, et al. Antibiotics in the treatment of upper respiratory tract infections in Poland. Is there any improvement? J Clin Pharm Ther 2010; 35:665-669.
- Thomas JK, Forrest A, Bhavnani SM, et al. Pharmacodynamic evaluation of factors associated with the development of bacterial resistance in acutely ill patients during therapy. Antimicrob Agents Chemother 1998; 42:521-527.
- Pechère JC. Patients’ interviews and misuse of antibiotics. Clin Infect Dis 2001; 33: S170-S173.
- Dajani AS. Adherence to physicians’ instructions as a factor in managing streptococcal pharyngitis. Pediatr 1996; 97:976-980.
- Pechère JC. Parameters important in short antibiotic courses. J Int Med Res 2000; 28:3A-12A.
- Sclar DA, Tartaglione TA, Fine MJ. Overview of issues related to medical compliance with implications for the outpatient management of infectious diseases. Infect Agents Dis 1994; 3:266-273.
- Pechère JC, Hughes D, Kardas P,et al. Non-compliance with antibiotic therapy for acute community infections: A global survey. Int J Antimicrob Agents 2007; 29:245-253.
- McNulty CAM, Boyle P, Nichols T, et al. The public’s attitudes to and compliance with antibiotics. J Antimicrob Chemother 2007; 60:63-68.
- Pavydė E, Veikutis V, Mačiulienė A, et al. Public knowledge, beliefs and behavior on antibiotic use and self-medication in lithuania. Int J Environ Res Public Health 2015; 12:7002-7016.
- Zowawi HM. Antimicrobial resistance in Saudi Arabia. An urgent call for immediate action. Saudi Med J 2016; 37:935-940.
- Al-Shammari SA, Khoja T, al-Yamani MJ. Compliance with short-term antibiotic therapy among patients attending primary health centers in Riyadh, Saudi Arabia. J R Soc Health 1995; 115:231-234.
- Fernandes M, Leite A, Basto M, et al. Non-adherence to antibiotic therapy in patients visiting community pharmacies. Int J Clin Pharm 2014; 36:86-91.
- McNulty CAM, Boyle P, Nichols T, et al. The public’s attitudes to and compliance with antibiotics. J Antimicrob Chemother 2007; 60:63-68.
- Kardas P. Patient compliance with antibiotic treatment for respiratory tract infections. J Antimicrob Chemother 2002; 49:897-903.
- Tong S, Pan J, Lu S, et al. Patient compliance with antimicrobial drugs: A Chinese survey. Am J Infect Control 2018; 46:e25-e29.
- Patel DV, Acharya UK, Shinde MK, et al. Compliance to antibiotic therapy at paediatric out-patient clinic. J Family Med Prim Care 2022; 11:1012-1018.
- Niaz Q, Godman B, Campbell S, et al. Compliance to prescribing guidelines among public health care facilities in Namibia; findings and implications. Int J Clin Pharm 2020; 42:1227-1236.
- Nakwatumbah S, Kibuule D, Godman B, et al. Compliance to guidelines for the prescribing of antibiotics in acute infections at Namibia’s national referral hospital: A pilot study and the implications. Expert Rev Anti Infect Ther 2017; 15:713-721.
- Sanson-Fisher R, Bowman J, Armstrong S. Factors affecting non-adherence with antibiotics. Diagn Microbiol Infect Dis 1992; 15:103-109.
- Brown MT, Bussell JK. Medication adherence: WHO Cares? Mayo Clin Proc 2011; 86:304-314.
- Llor C, Bjerrum L. Antimicrobial resistance: Risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf 2014; 5:229-241.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Khalid A Bin Abdulrahman1*, Ali M Alaseem2, Rayan A Bahmaid1, Mohammed M Alharbi1, Mohammed N Almutairi1 and Haitham A Alghufaily1
1Department of medical education, College of Medicine, Imam Mohammad Ibn Saud Islamic University, Riyadh, Saudi Arabia2Department of Pharmacology, College of Medicine, Imam Mohammad Ibn Saud Islamic University, Riyadh, Saudi Arabia
Received: 26-Aug-2022, Manuscript No. jrmds-22-73036; , Pre QC No. jrmds-22-73036(PQ); Editor assigned: 29-Aug-2022, Pre QC No. jrmds-22-73036(PQ); Reviewed: 13-Sep-2022, QC No. jrmds-22-73036(Q); Revised: 16-Sep-2022, Manuscript No. jrmds-22-73036(R); Published: 23-Sep-2022
