Research - (2022) Volume 10, Issue 1
Congenital Talipes Equinovarus (Club Foot): Overview, and Management Options
Masood Ahmed Qureshi1, Niaz Hussain Keerio2*, Syed Sajid Hussain3, Hassan Amir US Saqlain4, Muhammad Hamayun Hameed5, Abdul Hamid Kakar5 and Syed Shahid Noor6
*Correspondence: Niaz Hussain Keerio, Muhammad Medical College and Hospital Mirpurkhas, Saudi Arabia, Email:
Abstract
Talipes equinovarus also called clubfoot, the pes equinovarus is characterized by plantar flexion, inversion of the heel (from the midline of the leg) and adduction of the foot (medial deviation from the vertical axis of the leg). Although the clubfoot is the most common congenital skeletal deformity, along with congenital hip dislocation, and there is an immense number of publications, there is still no clarity about the optimal therapeutic approach. The value of a therapy only becomes apparent in the long term. Talipes equinovarus results from an anomaly of the talus. It occurs in 2 in 1000 live births and is bilateral in 50% of the affected children. It can appear alone or as part of a syndrome. A developmental hip dysplasia is more common in these children. Similar deformations that resulted from a sitting position in the uterus can easily be distinguished from clubfoot, as they can easily be corrected passively. The Larsen syndrome is a disorder that occurs in children with clubfoot and dislocations of hip, knee and elbow. The treatment of clubfoot requires great orthopaedic care and initially consists of repeated plaster applications, tapes or the use of a malleolar splint to bring the foot position into the correct position. If the cast is unsuccessful and the posture is severe, an operation may sometimes be necessary, which is best before the age of 12. Optimally, an operation before the age of 12 while the tarsal bones are still cartilaginous. Club feet can recur as children grow.
Keywords
Congenital talipes equinovarus, Club foot, Orthopaedic, Pediatric
Introduction
After hip dysplasia, clubfoot is the second most common congenital malformation in new-borns. About one to two babies in 1000 are born with this deformed foot. Bilateral clubfoot is found in around half of the cases, with boys more than twice as likely to be affected as girls. The severity of clubfoot in infants can vary, but the changes to healthy feet are also unmistakable for laypeople: The affected foot is turned inwards and there is often a deep crease on the sole of the foot [1]. The heel feels soft and stands up because of a shortened Achilles tendon. Especially with one-sided clubfoot, it is noticeable that the calf on the affected foot is slimmer than on the opposite side. The clubfoot is a foot deformity that the specialist recognizes by its characteristic features: The foot shows a position adjusted inwards and downwards in relation to the talus, typical characteristics are an equinus foot with a shortened Achilles tendon with a downward sloping foot (equinus), the forefoot describes a sickle shape (pes adductus), there is a hollow foot with an elevation of the longitudinal arch (Pes excavatus ), the calcaneus is in a varus position ("O position"/Pes varus) and the inner edge of the foot is raised (pes supinatus) [2].
These misalignments are caused by a displacement of the bones below the talus. In addition, the shape of the foot bones is often changed in clubfoot. The ligaments and muscles of the inner edge of the foot, especially the posterior tibial muscle (Musculus tibialis posterior), show clear structural changes and resemble scar tissue.
Foot experts differentiate the mostly congenital, primary clubfoot from the secondary clubfoot as a result of other injuries or diseases. The exact causes of primary clubfoot are still unclear and are likely due to several factors. A familial accumulation is clearly documented. The risk of clubfoot is 17 times higher if one parent also has clubfoot and 6 times higher if a grandparent was affected. With identical twins, there is a 33% risk that both children will develop clubfoot [3]. For dizygotic twins and siblings, it is 3% each. On the other hand, ethnicity also affects the likelihood of developing clubfoot. Polynesians and Aborigines have a significantly higher risk of this foot malformation than the white population. People of Asian origin, on the other hand, are less affected.
The symptoms are clearly visible in both congenital and acquired clubfoot. The person concerned walks on the outer edge of the foot or, in particularly severe cases, even on the back of the foot (as far as possible). One or both feet can be affected [4]. Usually, the clubfoot has four different characteristics: bony malformations (mostly affecting the heel bone), misalignments or dislocations in the joints (the ankle is often affected), weakened or shortened muscles (for example the calf muscles) and Limitations in the capsule-ligament apparatus (when tendons or ligaments are shortened or damaged).
The consequences of untreated congenital talipes equinovarus
Every clubfoot must be treated by a specialist; otherwise massive malposition will develop in adulthood. The walking and the regular function of the foot are very limited and both sides clubfoot walking is possible only with crutches.(1) As a result of the enormous improper loads on the entire skeletal system, severe bone damage occurs without exception.
Adults with clubfoot on one or both sides can only walk with great difficulty and pain. The rolling movement when running occurs mainly over the outer edge of the foot and in severe cases sometimes even over the back of the foot. As a result, thick calluses form on the affected areas of the ski [5].
The combination of a severe misalignment of the foot with the very tight, internal ligamentous apparatus and a shortened musculature causes massive restrictions in the mobility of the joints between the metatarsus and the rear foot [6]. Premature joint wear (osteoarthritis) is inevitable and in many cases, walking is only possible with orthopaedic custom-made shoes.
The best time to start the management
Therapy usually begins in the first or second week of life, when mother and child have recovered from the hardships of childbirth and feel strong enough to see a pediatric orthopaedist [7].
Pirani and dimeglio scoring systems
In a first step, the expert determines the severity of the foot deformation. With the Pirani score, the doctor evaluates three criteria for the forefoot and the rear foot with 0 points (=normal), ½ (=moderately changed) or 1 point (=abnormal) [8]. He examines the curvature of the outer edge of the foot, the depth of the wrinkles in the middle of the sole, the palpability of the outer talus or the dorsal (rear) hindfoot fold, the heel position and the mobility of the equinus (Table 1) [9].
| Deformity | Present and fixed (1) | Mild (0.5) | Absent (0) |
| Hind-foot deformities | |||
| Posterior heel crease | 1 | 0.5 | 0 |
| Empty heel | 1 | 0.5 | 0 |
| Rigidity of equinus | 1 | 0.5 | 0 |
| Mid-foot deformities | |||
| Curvature of lateral border of foot | 1 | 0.5 | 0 |
| Medial crease | 1 | 0.5 | 0 |
| lateral head of talus | 1 | 0.5 | 0 |
| Total Score | 6 | 3 | 0 |
Table 1: Pirani scoring system.
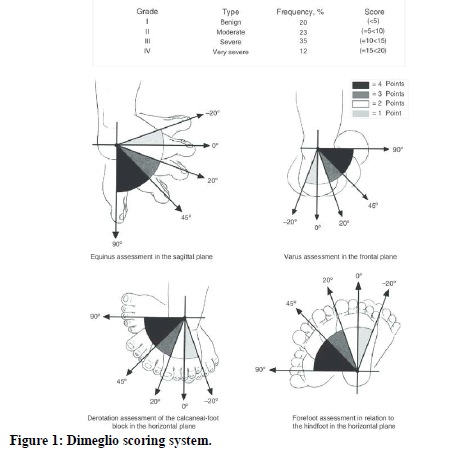
The so-called Dimeglio grid is also used, especially for club feet [10]. The orthopedic surgeon assesses the four main components of the clubfoot (equinus, internal rotation, pes varus, and pes adductus) and classifies them into four degrees of severity.
The total number of points allows an objective statement to be made as to how effective an orthopaedic treatment or an operation will be: Class 1 feet (benign or soft feet) with 0 to 5 points can be corrected better by orthopaedic treatment than class 4 feet (very heavy club feet) with 15 to 20 points (Figure 1) [11].
Figure 1: Dimeglio scoring system.
The more serious the specialist classifies the child's clubfoot, the longer the subsequent plaster treatment is likely to take. There is also a greater risk of the disease getting worse during treatment (relapse or “rebellious” clubfoot). Treatment is particularly difficult in the case of secondary clubfoot caused by a different disease.
History of ponseti method
Since clubfoot is the second most common orthopedic malformation in newborns, its treatment concept is of great importance [12]. The modern clubfoot treatment according to Ponseti is characterized by a significantly shorter treatment time of a far less complex surgical method compared to conventional techniques and the fact that the technique is proven with long-term results.
The orthopedist Ignacio Ponseti, born in Menorca in 1914, fled the Spanish Civil War and immigrated to the USA. He became a faculty member and practicing physician at the University of Iowa. In the 1950s he developed a method for the non-surgical treatment of congenital clubfoot [13]. The potential of his technology was misunderstood for many years, after all, the Internet spread the success stories of satisfied mothers and thus helped the Ponseti method to gain great attention in many countries.
The treatment of choice; Ponseti technique
In the past few decades, the Ponseti treatment has established itself as the gold standard in clubfoot therapy [14]. The gentle, globally recognized and highly effective method consists of three components that build on each other: (1) Plaster of paris redression treatment with weekly change for about 4 to 6 weeks: In a repressive treatment without surgery, a change is brought about using only a plaster of Paris; (2) Minimally invasive cutting of the Achilles tendon, this is necessary in 9 out of 10 children; (3) Final splint treatment: the child wears the splint for three months for 24 hours a day, then until the age of 4 only during bedtime.
The prerequisite for the impressive results of a Ponseti treatment is the consistent adherence to the individual therapy steps, precise knowledge of the manual correction grips (repression grips) and the unrestricted cooperation of the parents [15]. Regular check-ups by the orthopaedic surgeon up to school age are also an integral part of the treatment plan.
Plaster treatment of congenital talipes equinovarus according to ponseti
With the first cast, the first metatarsal bone is raised in the child in order to bring the forefoot and the rear foot into the same alignment and level [16]. This measure corrects the hollow foot component of the clubfoot.
Due to the coupling between the forefoot and the rear foot, further spreading the forefoot normalizes the heel position.
Finally, the orthopaedic surgeon tries to correct the equinus foot position with careful redression grips. He must not press too forcefully so that there is no secondary rocking foot (ink eraser foot). Excessive force during dorsiflexion (manual movement of the back of the foot towards the shin) can damage the ankle bone (talus). Since the ankle joint with the tibia and fibula form the upper ankle, this joint would be restricted in its mobility for life (flat-top talus). X-ray controls help identify other foot malposition such as a parallel position of the ankle and heel bones and severe rotational malposition of the exclude ankle for [16].
The foot is continuously redressed during the plaster treatment and fixed weekly in a padded plaster cast. In this way, the foot slowly turns a little further in the right direction over the course of several weeks of treatment.
Approximately 4 to 6 different plasters with a 90-degree knee flexion are required to achieve an almost complete correction. The plasters extend from the thigh over the lower leg and enclose the entire foot of the child.
In the Ponseti treatment, the orthopaedic surgeons use plasters that enclose the thigh. In this way, the plasters can hardly slip and keep the foot in a stable position. Another advantage is the fixed 90-degree knee flexion [17]. This position relaxes the two-headed calf muscle, which originates from the lower back of the thigh on the side of the shortened Achilles tendon.
Severing the achilles tendon
In 90% of children with clubfoot disease, a tenotomy of the Achilles tendon is necessary on the affected foot [18]. With them, the orthopaedic surgeon cannot flex the foot in the direction of the shin (dorsiflexion) by 15°.
In cases with a dorsiflexion over 15°, a lateral x-ray ensures the assessment of the actual correction of the hindfoot and helps to prevent a possible tendency towards the rocking foot (ink eraser foot).
Under short anesthesia, the orthopaedic surgeon cuts the Achilles tendon in a minimally invasive manner about 1 cm above the tendon insertion with a length of 1 cm. As part of the healing phase, the last cast remains in place for three weeks and should be applied with maximum splaying and overstretching of the foot. During this time, the bodies own tissue closes the gap in the Achilles tendon completely and in a straight line [19].
Final splint treatment for long-term success
In the case of a one-sided clubfoot, the diseased foot is fixed on the splint with an external rotation of 60 °, while the healthy foot is set to 40° in a one-sided clubfoot. The splint is adjusted to the width of the child's shoulder [20]. A click mechanism securely attaches the special shoes to the rail in a corrective position.
The splint has to be worn day and night for the first 3 months, with increasing improvement up to the age of 4; the child only wears the splint at night when sleeping. Experience has shown that the risk of a relapse (renewed deterioration) is greatest up to this age and children at this age usually tolerate the splint without any problems. The feet are slowly and carefully turned in the right direction with the splint orthosis.
The good and consistent cooperation of the parents during the entire clubfoot treatment is the prerequisite for a good result. The parents apply learned redression exercises on the child's foot and regularly attend appointments with the physiotherapist [21]. In particular, the parents must not be negligent with the splint therapy: Even a completely corrected clubfoot can worsen if the therapy plan is not adhered to and ruin the previous success. The regular check-ups by the orthopaedic surgeon up to school age guarantee that deterioration (relapses) is recognized at an early stage.
Surgical correction options for older children
From around the age of 4, mere soft tissue interventions on tendons, capsules and ligaments are often no longer sufficient to correct clubfoot [22]. In older children and adults, additional bony corrections are often necessary.
Surgical intervention on the heel bone (Dwyer osteotomy) corrects a malalignment of the rear foot. By means of a displacement (osteotomy) of the heel bone and fixation with screws, foot deformations can be treated that cannot be remedied conventionally [23]. If, on the other hand, the sickle foot component of the club foot predominates, a wedge removal from the cuboid bone on the outside of the foot, combined with the use of a wedge on the inside edge of the foot, makes sense [24].
Chances of management success
If a toddler wears the splints reliably and consistently after successful plaster treatment, the Ponseti method gives very good results in the long term [25]. In particular, it is clearly superior to the complex, classic surgical procedure (Parietal arthrolysis) and the treated feet show better mobility.
In most cases, the children's feet are fully functional after successful clubfoot therapy. With a one-sided clubfoot, the affected foot remains a little smaller and the calf muscles a little thinner (clubfoot calf).
Regular check-ups every 3 to 4 months by the orthopaedic surgeon serve in the first four years to ensure the success of the treatment and to tackle recurrences at an early stage. From the age of 4 until at least the child starts school, experts recommend halfyearly appointments.
Conclusion
Ignacio Ponseti (1914-2009) described the Ponseti method for idiopathic clubfoot in the 1950s. It took about four decades for this to be accepted worldwide as the method with the most successful results.
The clubfoot is a complex malalignment that consists of four components: (1) equinus, (2) hindfoot varus, (3) forefoot adductus and (4) cavus.
With his method, the clubfoot is corrected with two hands. The thumb of one hand serves as an abutment for the talus and the other hand is used to gradually move the foot under the talus. First, the forefoot is turned 90 ° outwards, which corrects the cavus. In the next few sessions, the forefoot is shifted outwards under the talus. The calcaneus moves into the correct position, the forefoot adductus and hindfoot varus components are corrected. As a rule, about six redression sessions are required to reach the final position (70 ° abduction). Ultimately, the equinus component is corrected by severing the Achilles tendon with a small incision under local anesthesia (percutaneous Achilles tenotomy). After this procedure, the foot is put in a cast in a slight equinus foot position.
The total duration of the treatment is approx. 8 weeks. Afterwards, the patient is switched to an abduction splint (Denis-Browne splint) during the day and night for three months. In order to ensure the success of the therapy, the splint must be worn at night until the end of the fourth year of life.
References
- Dobbs MB, Gurnett CA. Update on clubfoot: Etiology and treatment. Clin Orthop Relat Res 2009; 467:1146–53.
- Gibbons PJ, Gray K. Update on clubfoot. J Paediatr Child Health 2013; 49:e434-7.
- Alsiddiky A, Alrwibaah S, Alqahtani A, et al. Assessing public awareness of clubfoot and knowledge about the importance of early childhood treatment: A cross-sectional survey. BMC Pediatr 2019; 19:358.
- McCahill JL, Stebbins J, Harlaar J, et al. Foot function during gait and parental perceived outcome in older children with symptomatic club foot deformity. Bone Jt Open 2020; 1:384–91.
- Shtofmakher G, Kilfoil RL, Rozenstrauch A, et al. Talipes equinovarus (clubfoot): Neglected for 47 years and subsequent treatment. BMJ Case Rep 2014; 2014:bcr2014205395.
- Walling AK. The adult clubfoot (congenital pes cavus). Foot Ankle Clin 2008; 13:307–14.
- Liu YB, Li SJ, Zhao L, et al. Timing for ponseti clubfoot management: does the age matter? 90 children (131 feet) with a mean follow-up of 5 years. Acta Orthop 2018; 89:662–667.
- Dyer PJ, Davis N. The role of the Pirani scoring system in the management of club foot by the Ponseti method. J Bone Joint Surg Br 2006; 88:1082–4.
- Khan MA, Chinoy MA, Moosa R, et al. Significance of pirani score at bracing-implications for recognizing a corrected clubfoot. Iowa Orthop J 2017; 37:151–156.
- Fan H, Liu Y, Zhao L, et al. The correlation of pirani and dimeglio scoring systems for ponseti management at different levels of deformity severity. Sci Rep 2017; 7:14578.
- Andriesse H, Roos EM, Hägglund G, et al. Validity and responsiveness of the clubfoot assessment protocol (CAP). A methodological study. BMC Musculoskelet Disord 2006; 7:28.
- Shabtai L, Specht SC, Herzenberg JE. Worldwide spread of the ponseti method for clubfoot. World J Orthop 2014; 5:585–90.
- Dobbs MB, Khan SA. The life and legacy of Ignacio Ponseti. Indian J Orthop 2010; 44:114.
- Radler C. The Ponseti method for the treatment of congenital club foot: Review of the current literature and treatment recommendations. Int Orthop 2013; 37:1747–53.
- Dietz FR. What is the best treatment for idiopathic clubfoot? Evidence-Based Orthop Best Answers Clin Quest 2009; 264–72.
- Aydin BK, Sofu H, Senaran H, et al. Treatment of clubfoot with ponseti method using semirigid synthetic softcast. Med 2015; 94:e2072–e2072.
- Pulak S, Swamy M. Treatment of idiopathic clubfoot by ponseti technique of manipulation and serial plaster casting and its critical evaluation. Ethiop J Health Sci 2012; 22:77–84.
- Patwardhan S, Shyam A, Sancheti P. Prcutaneous needle tenotomy for tendo-achillis release in clubfoot -technical note. J Orthop Case Reports 2012; 2:35–6.
- Rahman MS, Alam MK, Shahiduzzaman M, et al. Percutaneous needle tenotomy for Ponseti technique in the management of congenital talipes equinovarus (CTEV). J Dhaka Med Coll 2015; 23:55–9. ‘
- Ošťádal M, Chomiak J, Dungl P, et al. Comparison of the short-term and long-term results of the Ponseti method in the treatment of idiopathic pes equinovarus. Int Orthop 2013; 37:1821–5.
- Zhao D, Liu J, Zhao L, et al. Relapse of clubfoot after treatment with the Ponseti method and the function of the foot abduction orthosis. Clin Orthop Surg 2014; 6:245–52.
- Dierauer S, Schäfer D, Hefti F. Osteotomies of the mid- and back-foot in recurrent club foot. Orthopade 1999; 28:117–24.
- Radler C, Mindler GT. Treatment of severe recurrent clubfoot. Foot Ankle Clin 2015; 20:563–86.
- Brihault J. Calcaneal osteotomy for hindfoot deformity. Orthop Traumatol Surg Res 2021; 103121.
- Smythe T, Mudariki D, Kuper H, et al. Assessment of success of the Ponseti method of clubfoot management in sub-Saharan Africa: A systematic review. BMC Musculoskelet Disord 2017; 18:453.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Masood Ahmed Qureshi1, Niaz Hussain Keerio2*, Syed Sajid Hussain3, Hassan Amir US Saqlain4, Muhammad Hamayun Hameed5, Abdul Hamid Kakar5 and Syed Shahid Noor6
1King Abdul Aziz Hospital, Makkah, Saudi Arabia2Muhammad Medical College and Hospital Mirpurkhas, Saudi Arabia
3Al Qassimi Hospital Sharjah, United Arab Emirates
4Al Qassimi Hospital Sharjah, United Arab Emirates
5Bolan Medical Complex Hospital Quetta, United Arab Emirates
6Orthopedic Department, Liaquat National Hospital and medical College Karachi, Pakistan
Citation: Masood Ahmed Qureshi, Niaz Hussain Keerio, Syed Sajid Hussain, Hassan Amir US Saqlain, Muhammad Hamayun Hameed, Abdul Hamid Kakar, Syed Shahid Noor, Congenital Talipes Equinovarus (Club Foot): Overview, and Management Options , J Res Med Dent Sci, 2022, 10(1): 47-51
Received: 12-Dec-2021, Manuscript No. JRMDS-21-47260; , Pre QC No. JRMDS-21-47260 (PQ); Editor assigned: 14-Dec-2021, Pre QC No. JRMDS-21-47260 (PQ); Reviewed: 28-Dec-2021, QC No. JRMDS-21-47260; Revised: 03-Dec-2021, Manuscript No. JRMDS-21-47260 (R); Published: 07-Jan-2022