Research - (2023) Volume 11, Issue 1
Correlation between the Digital Panoramic Radiograph and DEXA Examination as Tools in the Screening of Osteoporosis in Iraqi Postmenopausal Women
Asmaa Basheer AL-Suffar1* and Nazar Ghanem Jameel2
*Correspondence: Asmaa Basheer AL-Suffar, Department of Oral and Maxillofacial Surgery, College of Dentistry, University of Mosul, Iraq, Email:
Abstract
Osteoporosis is an asymptomatic high prevalence and incidence metabolic bone disease need a low-cost prescreening method for prediction to osteoporotic risk having post-menopausal females. Aims: To find if there is any correlation between panoramic mandibular index and Dual-energy X-ray Absorptiometry (DEXA) examination as well as the strength and direction of this relation. Materials and Methods: Analytical, experimental, and descriptive study performed for 69 postmenopausal females started by DEXA scan (grouped according to T-score in to 3 groups: normal, osteopenia and osteoporosis), followed by digital panoramic radiographic imaging for all females, radio morphometric measurements of bone images in mental areas were performed and statistical analysis with SPSS (version 26.0). Pearson Correlation coefficient used to obtain correlation and prediction equation. For best osteoporotic patient predictor, inter-rater reliability using Intraclass Correlation Coefficient, the level of statistical significance was set at 5% for an alpha error of <0.05. Results: Panoramic mandibular index has a positive week Correlation with spinal bone mineral density of about 0.37 with a high significant results P=0.002 for both sides, also a high significant difference between study groups (P<0.00) were present, but there were no statistical significant differences (P=0.2) between the 3 groups regarding the age and body mass index. Conclusion: Panoramic radiograph give an idea about the density condition of skeletal bone through the panoramic mandibular index as a linear morphometric analysis of mental area through its positive correlation with spinal bone mineral density.
Keywords
Panoramic, DEXA, Osteoporosis, Diagnosis , Radiography
Introduction
Osteoporosis (OP) is an asymptomatic high prevalence and incidence metabolic bone disease [1], characterized by low bone mass or bone density and micro architectural deterioration of bone tissue [2], frequently not detected until a fracture occurs, that entails significant social and economic burdens [3]. Bone loss occurs with age in men and women, but in the latter, the rate of loss increases at menopause (post-menopausal osteoporosis) [4]. Osteoporosis has an oral implications and effect on jaw as a part of skeletal system [5], causing loss of teeth, loss in alveolar bone height, erosion of inferior mandibular cortex, and reduced mandibular inferior cortical width [6]. It has effect on dental treatment plan and clinical success of dental implants is affected to a great extent by the volume and quality of the surrounding bone [7,8].
A significant problem is present in developing countries where the availability of DEXA (the gold stand osteoporosis diagnosis method) is limited. Also due to cost, workflow, and accessibility not all eligible women are evaluated with central DEXA. Where the prescreening or filtration of DEXA exam needed patients is necessary [9]. The earlier diagnosis of osteoporosis is better for prophylaxis of bone fractures. Dentists may play an important role in the early detection of increased bone fracture risk through using of Dental radiographs [6]. So the Aims of this study are to find osteoporosis prediction tool and prediction equation as well as, assess the relationship between radio morphometric measurements made on the panoramic mandibular bone image in comparison with BMD and T-score of the lumbar spine measured using DEXA examination.
Dual-energy X-ray Absorptiometry (DEXA)
DEXA regarded as the gold standard radiographic technique which diagnose OP, usually in the lower (lumbar) spine and hips to measure bone loss, it is highly reliable and accurate [10], safe with low cost [11], but it can rarely differentiate between the cortical and trabecular spaces and is prone to errors due to differences in the intervening soft tissue [12], so DEXA has a limitations, like the effect of growth and puberty on measures of bone mineralization. DEXA calculates bone density (BD) using a two dimensional image of three dimensional space, and is therefore at risk of incorrect estimations of bone depth and measures of true volumetric BD. The precision error and least significant change are unique to each center and limit the ability to compare results across machine models. Thus, best practice is for patients to undergo follow up imaging on the same DEXA device [13].
The BMD is defined through the T or Z-score; based on the WHO classification published in 1994 [14]. The T-score describes the number of standard deviations (SD) by which BMD differs from the mean value expected in young healthy individuals (for healthy 30-year-old subjects [15], while Z-score describes the number of SD by which BMD differs from the mean value expected for age and sex [16]. In 2019, the International Society for Clinical Densitometry (ISCD) published updated guidelines for low BMD and osteoporosis evaluation reference databases, and reporting terminology “Low” BMD in post-menopausal females and males over 50 years of age is defined by BMD less than 1 SD below the mean of healthy adults aged 30 years (T-score <-1.0 SD), while a T-score less than or equal to −2.5 SD or history of fragility fracture (fracture following a fall from standing height or vertebral fracture) is diagnostic of OP [17].
Panoramic radiographic examination
The Panoramic radiography is a popular technique due to its simplicity of operation, low radiation dosage in comparison with conventional full mouth Intraoral survey and the wide field of projected structures appear on it [18].
Materials and Methods
Study type and sample
Analytical, experimental, and descriptive study for 69 postmenopausal women aged between 49 and 79 years (mean 60.15 ± 7.34 years) who visited the private outpatient Oral and Maxillofacial Radiological center in Mosul city from 2019 to 2021 and they give a detailed explanation of the research and provided informed consent before enrollment.
Questionnaire
Demographic data were collected using a self-completed questionnaire, Body mass index, body height and weight were acquired. Patients were also inquired about history menopausal status.
Ethical guidelines
The study design was revised and approved by the Research Ethics Committee of the Faculty of Dentistry, Mosul University, Nineveh , Iraqi. with cod number (UoM. Dent/ H.1/20) (confirmation review letter/Version 1.0/1 December 2019).
Study design
The female patients examined by DEXA for lumber spine, then undergo to Digital panoramic imaging to examine the mandible.
Exclusion criteria
Patients aged under 49 years, or patients with a lumbar vertebrae traumatic fracture, and those having edentulous mandible, all were excluded from this study.
DEXA radiographical examinations
The BMD was assessed with DEXA in Adam's radio graphical specialist medical center using PRIMUS OsteoSys DEXA machine (OsteoSys Co.,Ltd.,9F,903 JnK Digital Tower, 111 Digital-ro 26, Guro-gu, Seoul, Korea), DEXA-dedicated technicians with experience in the technique performed all exams in accordance to the ISCD official positions(17), and following the diagnostic criteria for osteoporosis recommended by the WHO 1994(14). BMD was obtained automatically as the ratio between BMC (gm) and the scanned area (cm2). The BMD was measured at the lumbar region (L1–L4) (anteroposterior spine imaging) of the all 69 females. According to the BMD ,T-score, the patients classified into three groups:
Normal bone mineral density: Group 1 (T-score >-1.0)
Osteopenia: Group 2 (−2.5 <T-score ≤ -1.0)
Osteoporosis: group 3 (T-score ≤ -2.5) (Figure 1).
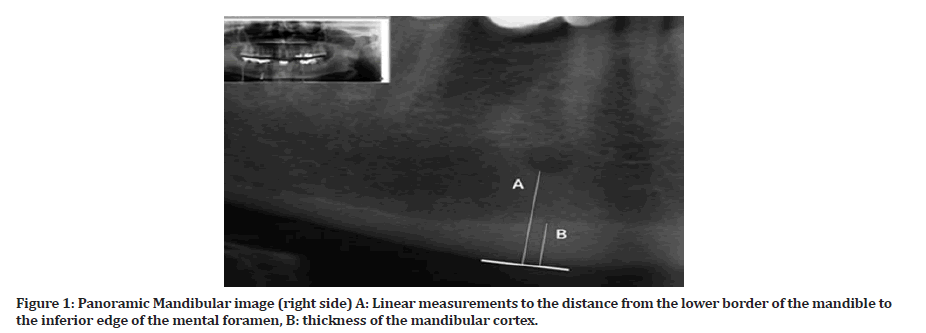
Figure 1: Panoramic Mandibular image (right side) A: Linear measurements to the distance from the lower border of the mandible to the inferior edge of the mental foramen, B: thickness of the mandibular cortex.
Digital Panoramic Radiography (DPR) recordings
The DPR taken by using Carestream extra oral Imaging System (CS 9000C, complies with Directive 93/42/EEC relating to medical equipment), this machine, made in France, with CS Imaging Version 7, exposure settings range 60 to 70 kVp and tube current of 10 to 15 mA and 13.1 sec. The position of the patient’s head was standardized following the manufacturing instructions. In order to achieve a standard, DPR were obtained, assessed and all measurements done by a single dentomaxillofacial radiologist with about 17 years of experience in presence of a reference metal object as a caliber to obtain most correct real linear measurements without magnification.
Measurements and analysis on DPR
The Linear quantitative measurements on DPR made using an analytical software (CS Imaging Software -7.0.3 Care Stream Health) after correcting the magnification factor by using the calibration panel option in that software and a metal reference object (with known real length). Measurements done on right and left side of the mandible image after localizing the mental regions areas, as different sides of the mandible may be influenced by different occlusal forces and thus could have the asymmetric signs in topographic anatomy [19].
Panoramic Mandibular Index (PMI)
The PMI on right and left panoramic side (PMI-R, PMI-L) represent the ratio between cortical thickness in the base of the mandible (line B) perfectly under the mental foramen and the distance from the center of the mental foramen to lower border of the base of the mandible (line A), (Figure 1). Mandibular cortical thickness represents the distance or measure between the inferior border of the mandible and the superior border of the base of mandible under the mental foramen. The data are expressed in millimeters:
PMI=(Thickness of the mandibular cortex)/(distance from the center of mental foramen to the lower border of mandible base)
Statistical analysis and reliability test
SPSS statistical software was used to analyze the data (version 26.0). The Kolmagrov-Simirnov test was used to determine the kind of distribution. For bivariate analysis Student’s t-test for means in normal distribution variables (using the Levene test for variance equality) and non-parametric tests such as the U Mann–Whitney test (independent samples) for variables showing nonnormal distribution were used. Pearson Correlation coefficient used to obtain correlation and prediction equations. For best osteoporotic patient predictor, interrater reliability using Intraclass Correlation Coefficient (ICC), The level of statistical significance was set at 5% for an alpha error of <0.05.
Results
Reliability test
The correlation coefficient (R) show a very strong correlation between both raters P<0.0001. The intraclass correlation in between both raters were for PMI–L (0.906), and for PMI-R about (0.898).
Descriptive analysis of the total sample
The total sample's demographic characteristics present in Table 1 in which they were with mean age of 60.15 ± 7.34 years. The age distribution deviates considerably from normal distribution (p= 0.002). Participants' BMIs mean of 30.51 ± 4.76 kg/m2 , and it was within normal distribution (p=0.1).
| Variable | Min-Max | Mean | Skewness | Kurtosis | Normality test |
|---|---|---|---|---|---|
| Age, year | 49-79 | 60.15 ± 7.34 | 0.75 | -0.196- | 0.002 |
| BMI, kg/m2 | 19.70 -45.50 | 30.51 ± 4.76 | -0.03 | 0.624 | 0.1 |
| Fat% | 11 – 48 | 34.48 ± 6.84 | -0.89 | 1.329 | 0.01 |
| Spinal-BMD | 0.578 -1.277 | 0.93 ± 0.17 | 0.13 | 0-.834- | 0.1 |
| Spinal T-score | -5.9 | -1.38 ± 1.43 | 0.13 | -0.815- | 0.1 |
| Spinal Z-score | -6.5 | -0.50 ± 1.41 | 0.01 | -0.696- | 0.4 |
| PMI –R (Right) | 0.057 -0.625 | 0.34 ± 0.11 | 0.25 | 0.709 | 0.1 |
| PMI-L ( left) | 0.117 -0.552 | 0.34 ± 0.09 | 0.004 | -0.473- | 0.8 |
| Body mass index (BMI), Bone mineral density (BMD), Panoramic mandibular index (PMI) | |||||
Table 1: escriptive analysis of total study sample.
Descriptive analysis of sample according diseases status
Based on spinal BMD(S-BMD) values, studied sample (69) was subdivided into a normal subjects in 28 (40.6%), osteopenic patients in 20 (29.0%), and osteoporotic patients in 21 (30.4%). The distribution of demographic, DEXA characteristics, and PMI indices parameters according to health status are shown in Table 2. ANOVA tests with the post hoc Duncan contrast technique were used to determine mean homogeneity among the three research groups. If the variable is not normally distributed, the non-parametric Kruskall- Wallis test was performed instead. According to values of PMI. there were a highly significant difference (p<0.00) between normal females and osteopenia females, also between normal and osteoporotic females, as well as the values of (S-BMD, T, and Z-score) were a highly significant difference between osteopenia and osteoporosis females.
| Variable | Normal | Osteopenia | Osteoporosis | P-value |
|---|---|---|---|---|
| Age, year | 58.61 ± 7.22 | 62.30 ± 7.52 | 60.15 ± 7.17 | 0.2 |
| BMI, kg/m2 | 31.43 ± 3.86 | 31.33 ± 5.48 | 28.67 ± 4.93 | 0.09 |
| Fat% | 34.61 ± 4.97 | 35.69 ± 7.02 | 33.20 ± 8.72 | 0.5 |
| Spinal-BMD | 1.11 ± 0.085 a, b | 0.89 ± 0.03c | 0.74 ± 0.06 | <0.0001 |
| Spinal T-score | 0.09 ± 0.701a,b | -1.73 ± 0.317c | -3.01 ± 0.542 | <0.0001 |
| Spinal Z-score | 0.88 ± 0.740a,b | -0.72 ± 0.427c | -2.15 ± 0.592 | <0.0001 |
| PM I –R (Right) | 0.39 ± 0.104a,b | 0.29 ± 0.084 | 0.32 ± 0.119 | 0.004 |
| PM I-L ( left) | 0.38 ± 0.090a,b | 0.30 ± 0.099 | 0.32 ± 0.094 | 0.009 |
| Body mass index (BMI), Bone mineral density (BMD), Panoramic mandibular index (PMI),Statistically not significant (P = 0.05), a (normal-osteopenia), b (normal-osteoporosis), Confidence interval (CI). | ||||
Table 2: Descriptive analysis of total sample according diseases status.
Descriptive analysis relating to PMI-R and PMI-L according diseases status
For normal females, the PMI-R mean SD was 0.39 ± 0.10; and for PMI-L mean SD of 0.38 ± 0.09, PMI-R in osteopenia females was with mean SD 0.29 ± 0.08 and in PMI-L with mean SD 0.30 ± 0.09, Lastly, in osteoporosis females, PMI-R was with mean SD of 0.32 ± 0.11 and nearly similar of 0.32 ± 0.0 for PMI-L with a high significant difference between study groups (P<0.00) for both sides. A post hoc analysis was performed and reveals that the three subgroups were non-homogenous and differences were statistically significant (Table 3).
| Normal | Osteopenia | Osteoporosis | P-value | |||||
|---|---|---|---|---|---|---|---|---|
| PMI-R | PMI-L | PMI-R | PMI-L | PMI-R | PMI-L | PMI-R | PMI-L | |
| Range | 0.21-0.62 | 0.21-0.54 | 0.08-0.43 | 0.13-0.55 | 0.05-0.60 | 0.11-0.48 | 0.004 | 0.009 |
| Median | 0.37 | 0.38 | 0.31 | 0.29 | 0.32 | 0.34 | ||
| Mean ± SD | 0.39 ± 0.104a,b | 0.38 ± 0.090a,b | 0.29 ± 0.084 | 0.30 ± 0.099 | 0.32 ± 0.119 | 0.32 ± 0.094 | ||
| 95% CI for mean |
0.35-0.43 | 0.35-0.42 | 0.25-0.3 | 0.26-0.35 | 0.26-0.37 | 0.28-0.36 | ||
| Statistically not significant (P = 0.05), a (normal-osteopenia), b (normal-osteoporosis), Confidence interval (CI). Panoramic mandibular index (PMI) | ||||||||
Table 3: Descriptive analysis of PMI-R and PMI-L according diseases status.
Direction and strength of PMI and BMD of lumber vertebrae
The PMI has a positive week Correlation (R) with BMD of about 0.37 for right and left sides, the regression (R2: determine the degree of variation in BMD that explained by radiological indices) were 0.13 for right and 0.14 for left side with a high significant results P=0.002 for both sides, predicting equations for S BMD (Y) based on recorded radiological index (X), it was: Y= 0.71+0.65* (X) for PMI-R, and for PMI-L was Y=0.74+0.57* (X) (Table 4 and Figure 2).
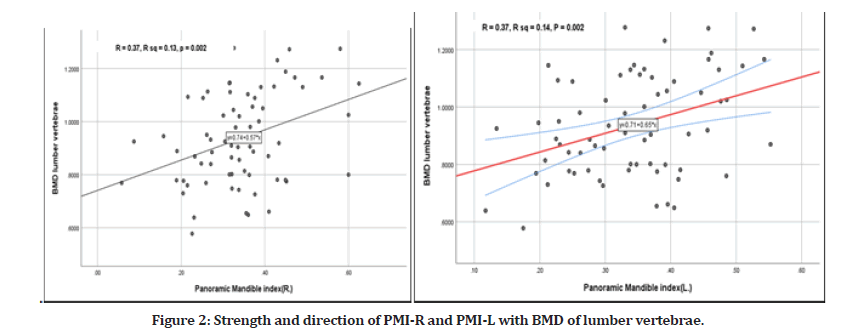
Figure 2: Strength and direction of PMI-R and PMI-L with BMD of lumber vertebrae.
| BMD | T-score | Z-score | ||||||
|---|---|---|---|---|---|---|---|---|
| Test | R | R2 | P | Prediction equation | R | P | R | P |
| PMI-R (right) | 0.37 | 0.13 | 0.002 | Y=0.74+0.57*(X) | 0.37 | 0.002 | 0.31 | 0.009 |
| PMI-L ( left) | 0.37 | 0.14 | 0.002 | Y=0.71+0.65*(X) | 0.38 | 0.001 | 0.35 | 0.003 |
| Statistically not significant (P = 0.05), Regression (R2), Correlation (R). Panoramic mandibular index (PMI) | ||||||||
Table 4: Strength and direction of PMI-R and PMI-L with BMD, T and Z-Scors of lumber vertebrae.
Discussion
Studies on various anatomic sites and via various imaging modalities to predict osteoporosis indicate it is a disease that affects the entire skeleton, thereby allowing for global screening of bone quality from individual sites [10], so this study tends to reflect and predict the skeletal bone status in dental clinic and osteoporosis for post-menopausal women above 50 years as the mean age of menopause occurred was 50 years. According to this study results, the dentists who use panoramic radiographs may play a vital role in screening patients with osteoporosis, mainly postmenopausal women; this is because, it is most often advised as a part of a routine investigation and as it is also less expensive than DEXA scan [20].
The mean PMI value of total sample was 0.34, nearly similar in its value with Grocholewicz, et al. [6] study=0.33. The results of this study, relating to PMI show a highly significant difference (p<0.00) between DEXA groups, BMD, and T- score, so when the value of S-BMD decreased, the PMI diminished to a point of statistical significance, it means that when the level of PMI decreases, it indicates lowing of S-BMD, this in coordination with Bilgili, et al. [21] who found that PMI was lower in value in patients with OP than in healthy individuals.
In this study, a weak positive linear correlation of PMI (R =0.37, p =0.002) with S-BMD. This coordinated with Mansour, et al. [19] study's in which the Pearson’s correlation coefficient showed a statistically significant positive correlation between T- score and PMI [R= 0.36], also Gaur et al. [20] who also found a correlation between the low bone mass density in post-menopausal women and the PMI, these previous studies, show similar evaluation to that performed by Benson, et al. [22], who present and used PMI to compensate for the vertical magnification that differs among various panoramic machines, but found a very weak correlation between the PMI and BMD. A stronger relation in Yagmur, et al. [23] study who proven that there is a good correlation between PMI and BMD values and can be used as a preliminary diagnosis in evaluating osteoporotic changes.
In controversy, Stagraczynski, et al. [24] mentioned that no correlations were found between PMI and BMD in postmenopausal women relating that to PMI is not adequate radiological marker of vertebral bone loss in postmenopausal women. Also PMI proved to be ineffective in the screening of osteopenia/osteoporosis in women in the study of Grocholewicz , et al. [6]. This disagreement between studies including the present study may be due to PMI limitations that are mainly related to the agreement/experience between different operators and the quality of different images, magnification, distortion, differences in settings between different equipment and exposure parameters, the same machine may produce a different magnification in relation to the patient position, magnification change between different panoramic parts of the same radiographs [25]. Only 14% and 13% of variation in skeletal BMD is explained by PMI-L and PMI-R respectively known through regression test.
The age and BMI differences between the 3 groups was not statistically significant [P=0.2], this supported by Holmberg, et al. [26] [P= 0.91] regarding to age but significant regarding to BMI, also according to value of [S-BMD, T and Z-score], there were a high significant difference [p<0.0001], among the study groups, also this supported by the study of Holmberg et al. [26]. According to Sghaireen, et al. [27], panoramic radiography plays a vital role in the diagnosis of OP among postmenopausal women. Munhoz, et al. [28] mentioned that, the radio morphometric PMI is valuable as auxiliary tools in the identification of postmenopausal females at risk of osteoporosis, as they also correlate with BMD similar to Calciolari, et al. [16] who concluded that the panoramic mandibular indices is useful tool that potentially could be used by dentists to screen for low BMD, so these studies support this study's results and conclusions.
Conclusion
Panoramic radiograph give an idea about the condition of skeletal bone through the PMI as a linear morphometric analysis of mental area through its positive correlation with DEXA spinal BMD.
Consent to Participate
We, the authors, guarantee that we participated in the completion of the manuscript. The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Consent for Publication
We, the authors agree to publish the manuscript in your journal.
Competing Interests
There are no competing interests for this work.
Funding
There is no funding.
Author's Contributions
The research is a part of Ph.D. thesis related to 1st author, who supervised by the 2nd author, the writing of the research for both authors.
Acknowledgements
To my college of dentistry, university of Mosul.
References
- Ulivieri FM, Rinaudo L, Piodi LP, et al. Bone strain index as a predictor of further vertebral fracture in osteoporotic women: An artificial intelligence-based analysis. PLoS One 2021; 16:e0245967.
- Nakamoto T, Taguchi A, Verdonschot RG, et al. Improvement of region of interest extraction and scanning method of computer-aided diagnosis system for osteoporosis using panoramic radiographs. Oral Radiol 2019; 35:143-151.
- Löffler MT, Jacob A, Scharr A, et al. Automatic opportunistic osteoporosis screening in routine CT: improved prediction of patients with prevalent vertebral fractures compared to DXA. Eur Radiol 2021; 31:6069-6077.
- Agarwal SC. Understanding bone aging, loss, and osteoporosis in the past. Biol Anthropol Hum Skel 2018; 385-414.
- Miliuniene E, Alekna V, Peciuliene V, et al. Evaluation of bone mineral density in postmenopausal women with alterations of the mandible cortical bone. Stomatologija 2016; 18:86-91.
- Grocholewicz K, Janiszewska-Olszowska J, Aniko-Włodarczyk M, et al. Panoramic radiographs and quantitative ultrasound of the radius and phalanx III to assess bone mineral status in postmenopausal women. BMC Oral Health 2018; 18:127.
- Wang SH, Shen YW, Fuh LJ, et al. Relationship between cortical bone thickness and cancellous bone density at dental implant sites in the jawbone. Diagnostics 2020; 10:710.
- Kim OS, Shin MH, Song IH, et al. Digital panoramic radiographs are useful for diagnosis of osteoporosis in Korean postmenopausal women. Gerodontology 2016; 33:185-192.
- Nguyen HG, Lieu KB, Ho-Le TP, et al. Discordance between quantitative ultrasound and dual-energy X-ray absorptiometry in bone mineral density: The Vietnam osteoporosis study. Osteoporos Sarcopenia 2021; 7:6-10.
- Schreiber JJ, Kamal RN, Yao J. Simple assessment of global bone density and osteoporosis screening using standard radiographs of the hand. J Hand Surg Am 2017; 42:244-249.
- Williams KM, Darukhanavala A, Hicks R, et al. An update on methods for assessing bone quality and health in Cystic fibrosis. J Clin Transl Endocrinol 2022; 6:100281.
- Kerkettaa SR, and Ghoshb D. Microwave sensing for human bone health evaluation. Int J Elect Commun 2020; 127:153469.
- Zemel BS, Wasserman H, Kelly A, et al. Intermachine differences in DXA measurements vary by skeletal site, and impact the assessment of low bone density in children. Bone 2020; 141:115581.
- Kanis JA. WHO Study Group. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. Osteoporos Int 1994; 4:368–381.
- Kim E, Cho HE, Jung JH, et al. Can radial bone mineral density predict spinal bone mineral density in patients with advanced Duchenne muscular dystrophy? Medicine 2018; 97:e12303.
- Calciolari E, Donos N, Park JC, et al. Panoramic measures for oral bone mass in detecting osteoporosis: a systematic review and meta-analysis. J Dent Res 2015; 94:17S-27S.
- Shuhart CR, Yeap SS, Anderson PA, et al. Executive summary of the 2019 ISCD position development conference on monitoring treatment, DXA cross-calibration and least significant change, spinal cord injury, peri-prosthetic and orthopedic bone health, transgender medicine, and pediatrics. J Clin Densitom 2019; 22:453-471.
- Srivastava A, Raghav P, Pradhan S. Effectiveness of orthopantomograph in vertical mandibular measurements: A systematic review. J Oral Maxillofac Radiol 2021; 9:45-51.
- Mansour S, AlGhamdi AS, Javed F, et al. Panoramic radiomorphometric indices as reliable parameters in predicting osteoporosis. Am J Med Sci 2013; 346:473-478.
- Gaur B, Chaudhary A, Wanjari PV, et al. Evaluation of panoramic radiographs as a screening tool of osteoporosis in post-menopausal women: A cross sectional study. J Clin Diagn Res 2013; 7:2051-2055.
- Bilgili E. Evaluation of the effect of osteoporosis on mandible with mandibular indexes using panoramic radiography and cone beam computed tomography. EADS 2021; 48:13–17.
- Benson BW, Prihoda TJ, Glass BJ. Variations in adult cortical bone mass as measured by a panoramic mandibular index. Oral Surg Oral Med Oral Pathol 1991; 71:349-356.
- Yagmur B, Tercanli-Alkis H, Tayfun-Kupesiz F, et al. Alterations of panoramic radiomorphometric indices in children and adolescents with beta-thalassemia major: A fractal analysis study. Med Oral Patol Oral Cir Bucal 2022; 27:e10-e17.
- Stagraczyński M, Kulczyk T, Podfigurna A, et al. Estimation of mandibular bone status and lumbar bone mineral density in postmenopausal women. Pol Merkur Lekarski 2016; 41:79-83.
- Pfeiffer P, Bewersdorf S, Schmage P. The effect of changes in head position on enlargement of structures during panoramic radiography. Int J Oral Maxillofac Implant 2012; 27.
- Holmberg T, Bech M, Gram J, et al. Point-of-care phalangeal bone mineral density measurement can reduce the need of dual-energy x-ray absorptiometry scanning in danish women at risk of fracture. Calcif Tissue Int 2016; 98:244-252.
- Sghaireen MG, Alam MK, Patil SR, et al. Morphometric analysis of panoramic mandibular index, mental index, and antegonial index. J Int Med Res 2020; 48:300060520912138.
- Munhoz L, Morita L, Nagai AY, et al. Mandibular cortical index in the screening of postmenopausal at low mineral density risk: A systematic review. Dentomaxillofac Radiol 2021; 50:20200514.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Asmaa Basheer AL-Suffar1* and Nazar Ghanem Jameel2
1Department of Oral and Maxillofacial Surgery, College of Dentistry, University of Mosul, Iraq2Department of Dentistry, AL-Hadbaa University College, Iraq
Citation: Asmaa Basheer AL-Suffar, Nazar Ghanem Jameel, Correlation between the Digital Panoramic Radiograph and DEXA Examination as Tools in the Screening of Osteoporosis in Iraqi Postmenopausal Women, J Res Med Dent Sci, 2023, 11 (1):69-75.
Received: 05-Dec-2022, Manuscript No. jrmds-22-85595; , Pre QC No. jrmds-22-85595(PQ); Editor assigned: 07-Dec-2022, Pre QC No. jrmds-22-85595(PQ); Reviewed: 22-Dec-2022, QC No. jrmds-22-85595(Q); Revised: 27-Dec-2022, Manuscript No. jrmds-22-85595(R); Published: 03-Jan-2023
