Research - (2023) Volume 11, Issue 2
Correlation between the Etraction of Permanent Teeth in Children and Future Growth of Third Molar
*Correspondence: Rusul A Alsaray, Dentistry Department, Kut University College, Iraq/Kut-Wasit, Iraq, Email:
Abstract
Background: permanent molar (M3) formation, morphology, and agenesis vary greatly between individuals. This study examines how removing the lower first permanent molar affects the position and angle of the developing third molar in 7- to 10-year-olds.
Method: Radiographs of Two groups from southern Iraq were identified: those who had one or more first permanent molars extracted between ages 7 and 10 and those who did not. Both groups had panoramic radiographs taken at 8.5 and 10 years before extraction. 80 third molars were extracted, and 50 had retained first permanent molars. Comparing groups used independent sample tests.
Results: The third molar moved significantly more mesially in the group of extraction (P<0.05), and the angle righted itself significantly more in the group of extraction than it did in the group of non-extraction (P<0.05). Both of these results were significantly different from what was seen in the group of non-extraction. These two findings presented a striking contrast to the findings obtained from the control group that did not undergo extraction. When it came to the movement of the third molar downward, there's not a statistical significant difference between two groups in terms of a vertical movement of the 3rd molar.
Conclusion: An extraction of the lower first permanent molar encouraged mesial movement and up righting of the developing third molar while the dentition was still in the process of developing. Because of this, the probability of the third molar erupting in the future may increase.
Keywords
Permanent teeth, Dental extraction, Pediatric dentistry, Future growth, Third molar
Introduction
It is possible for the mandibular third permanent molar, also known as the M3, to display a great deal of variability depending on the individual in terms of its agenesis, its timing of formation, and its morphology [1]. Calcification happens between the ages of seven and ten years old in the vast majority of cases; however, in exceptional cases, it can take as long as fourteen years to take place [2]. Eruption is a natural process that typically occurs between the ages of seventeen and twenty-one and can sometimes occur earlier. The incidence of mandibular third molar impaction is reported to be 25.4% worldwide, which indicates that it is a condition that occurs quite frequently [3]. The surgical removal of third molars comes with a number of significant risks, including the possibility of bleeding, infection, alveolar osteitis, and sensory disturbances of the inferior alveolar and lingual nerves in 0.35–8.4 percent of cases. These risks can be avoided by choosing an alternative treatment, such as orthodontics, which does not require surgery [4]. By choosing an experienced oral surgeon who has extensive experience in the field, you can reduce the likelihood of experiencing any of these risks. The development of the mesio-angular occlusal surface of the M3 takes place in the superficial portion of the ramus [5].
As a result of the growth of the mandible, it moves into a position that is more upright and submerges inferiorly as it moves from the ramus to the body of the mandible [6]. This occurs as the mandible transitions from the ramus to the body of the mandible. This is because the body of the mandible expands to accommodate the growing mandible, which results in more space being available. The third molars have a better chance of erupting into position if they are angled at an upright position and there is space for them in the mouth. It is possible to remove first permanent molars (M1) with a poor prognosis as early as possible in order to encourage mesial movement of the second permanent molar. This is done by extracting the tooth as soon as possible after it has become visible. To accomplish this, the M1 must be extracted as quickly as is humanly possible [7].
Caries or molar incisor hypo-mineralization (also known as MIH) is typically the underlying conditions that necessitate the need for this procedure [8]. It is possible that the removal of M1 at the optimal moment in time will reduce the need for intricate restorative treatment as well as the subsequent later loss that is caused by the spacing that it causes. This is because the removal of M1 at the optimal moment in time will occur at the optimal moment in time [9]. If everything goes according to plan, the early extraction of the developing second molar should allow it to erupt in a more mesial position, thereby reducing the amount of residual spacing and the necessity for subsequent orthodontic intervention [10]. This is assuming that everything goes according to plan. This is based on the assumption that everything works out as anticipated [11]. After the M1 has been extracted, the unerupted second permanent molar and the M3 will typically produce a satisfactory occlusal position in the maxilla. This will occur after the extraction of the M1 [12]. On the other hand, the mandible is known for having frequent instances of spacing and drifting in its structure [13]. If the mandibular M1 is extracted between the ages of 7 and 10 years, which is when the second permanent molar is still un-erupted and the third molar is present, there is a significantly increased likelihood that space closure will occur spontaneously via mesial migration of the second molar [14]. This is the age range in which this phenomenon is most likely to take place. On the other hand, there is also the possibility that the second permanent molar has already emerged but that the third permanent molar has not yet done so [15]. The panoramic radiograph is utilized quite frequently in orthodontic treatment, despite the fact that it magnifies some details while distorting others [16]. This is the case in spite of the fact that it has a number of restrictions. Even though the apparent angle of each tooth on the panoramic radiograph does not match the true angulation of the teeth, this difference is almost never clinically significant [17]. This is because the apparent angle of each tooth on the panoramic radiograph does not represent the true angulation of the teeth. This is due to the fact that the apparent angle of each tooth on the panoramic radiograph does not represent the teeth's true angulation. Even though panoramic radiographs do not provide a representation that is entirely accurate, they do provide a high diagnostic yield [18].
This is because panoramic radiographs are taken from multiple angles. In the context of research, in order for the conclusion to be relied upon, the results should have a high enough level of significance and the interpretation of those results should be done with care [19]. On the other hand, if the mandibular or maxillary second permanent molar is extracted before the eruption of the M3, there is a good chance that the M3 will emerge in a position that is satisfactory [20]. There is evidence to suggest that the extraction of the premolars, followed by orthodontic treatment, results in an improvement in the angle and space for the M3 tooth. In some of the studies, patients who had asymmetric M1s extracted before the age of 10 years and were followed up to the middle of adolescence were analyzed [21]. They discovered that the development and eruption of the M3 was significantly sped up on the extraction side compared to the control side, which did not involve any extraction at all. This was discovered in comparison to the side that did not involve any extraction at all. This was determined by drawing parallels between the extraction side and the side that did not involve any sort of extraction [22]. Research methods such as correlation and causation analysis, the purpose of this study is to determine whether or not there is a connection between the early loss of permanent teeth in children and the subsequent growth of the third molar by determining whether or not there is a connection between the early loss of permanent teeth in children.
Materials and Methods
In order to fulfill the requirements of the plan for the research project, radiographic analysis was carried out in a retrospective fashion. Volunteers were chosen at random from the pediatric theatre list between the dates of March 5, 2019, and April 3, 2022 in order to take part in the study. The study ran from March 5, 2019, to April 3, 2022. The duration of the study was a complete five years. In addition to the procedures that were recorded, the records of children who had undergone extractions for M1s with a panoramic radiograph both before the extraction and at least one year after the extraction were reviewed. These children had all been given panoramic radiographs before the extraction. These children (Table 1) had all undergone M1 extraction at least once during their lifetimes. Before any of these children underwent the process of having teeth extracted, a panoramic radiograph was taken of their mouths. It was common knowledge that these kids did not have a good chance of making a full recovery from their conditions. Patients who had panoramic radiographs taken in preparation for maxillary procedures were included in the study's non-extraction group. The study was conducted on patients who did not have their teeth extracted. The name of this group was included on the theater's guest list, which made it simple to recognize them there. These procedures included the removal of maxillary teeth as well as the exposure and bonding of any ectopic maxillary teeth that were present. In addition, the maxillary teeth were prepared for bonding and then exposed. In addition, the patient's maxillary teeth had to be extracted in order to complete these procedures.
These participants, who had otherwise normal development of their mandibular teeth, were chosen to have panoramic radiographs taken between the ages of 7 and 10 and then at least one year later, just like the group that had their teeth extracted. The results of these radiographs were compared to those of the group that had their teeth extracted. These radiographs' findings were compared to those obtained by the group that had their teeth extracted earlier in the study. The results of these radiographs were analyzed and compared to the results obtained from the group that had their teeth removed. The following served as eligibility criteria for participants to be included in the study, and they were taken into consideration: M3 needs to be adequately developed with the outline of the occlusal surface visible, and panoramic radiographs need to have been taken between 7 and 10 years prior to the extraction (D1), in addition to at least one year later after the extraction itself (D2). Radiographs of the patient's D2 were taken as part of the orthodontic evaluation that was performed. Patients who met a certain set of criteria were not allowed to take part in the study.
These criteria included craniofacial syndromes, eruption anomalies, hypodontia, extraction of other permanent mandibular teeth, patients who had orthodontic treatment between D1 and D2, and patients with poor-quality radiographs. In addition, patients with craniofacial syndromes were more likely to have poor quality radiographs. Plain film radiographs were the only type of radiographs that were examined for this research; as a consequence, the primary investigator scanned all of the radiographs from those types of radiographs at a resolution of 1200 DPI from those plain film radiographs. In order to develop a program that is capable of performing radiograph analysis, the medical physics department utilized the open-source software known as "ImageJ." This was done in order to fulfill the requirements set forth by the division. The division that you are currently working in was the one that came up with the basic idea for this program. On the panoramic radiograph, the landmarks, lines, linear and angular measurements, and positional measurements of the mandibular M3 bone have all been recalculated as a consequence of the findings of earlier studies that investigated the movement of the bone in its previous location. The purpose of these studies was to determine how the position of the mandibular M3 bone changed over the course of time (Figures 1 to Figure 3).
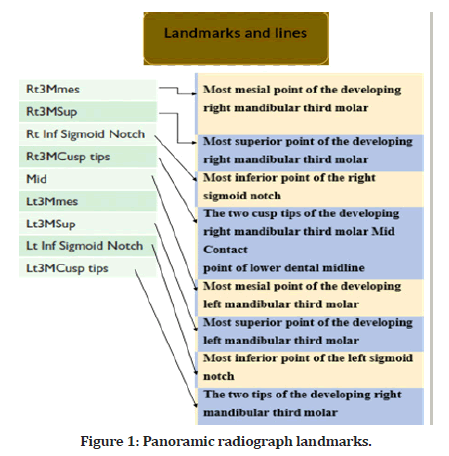
Figure 1: Panoramic radiograph landmarks.
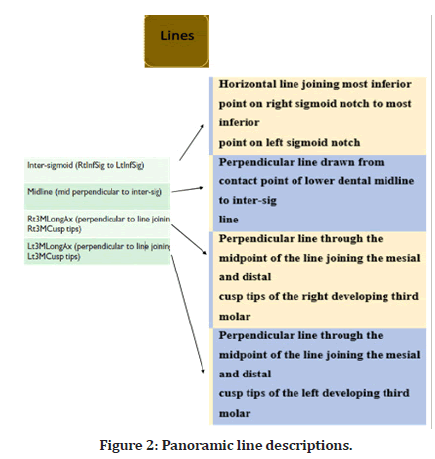
Figure 2: Panoramic line descriptions.
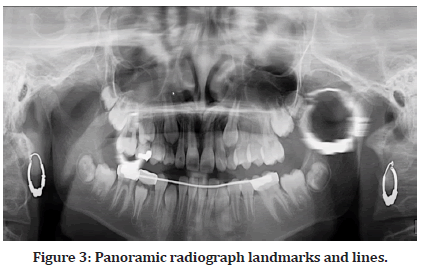
Figure 3: Panoramic radiograph landmarks and lines.
Finidings to Investigate
It was decided that the dental midline ought to function as the vertical reference midline, and that the horizontal movement of the M3 ought to be evaluated in relation to the dental midline. A recording was made in order to determine the distance between the most distal point of the developing M3 and the midline of the body. This distance was determined by listening to the recording. This was done in order to obtain a measurement that was as accurate as possible. The number of pixels that are present on the D1 and the D2 are contrasted with one another and compared to one another for the purpose of the measurement. The vertical movement of the developing M3 was measured as the distance in pixels between the most superior point of the M3 and the horizontal reference plane, which was the intersigmoid line, between D1 and D2. This provided a measurement of the vertical movement of the developing M3. This allowed for an accurate measurement of the developing M3's vertical movement. Because of this, an accurate measurement of the vertical movement of the developing M3 was able to be obtained. It was determined how far this distance was by using it as a point of reference, and then the vertical movement of the developing M3 was calculated. We were able to measure the angular change that was taking place during the development of the M3 by utilizing the long axes of the M3 and situating them in relation to the intersigmoid line. This allowed us to determine how the M3 was evolving. The angle of the M3 can be calculated by using the angle that is formed by the longitudinal axis of the developing M3 in relation to the horizontal reference line. Following that, the degree reading is obtained by starting at this angle.
Linear measurements
Because a panoramic radiograph does not have a ruler like a lateral cephalogram does, the linear measurements had to be done in pixels. This is in contrast to the lateral cephalogram, which does have a ruler. In contrast to this, the lateral cephalogram will have a ruler to measure the patient's head. This step was necessary because the measurements needed to be converted to a millimeter scale for accuracy purposes. Even though each panoramic radiograph was produced with the same piece of equipment and in accordance with the same set of standard operating procedures, the magnification of each radiograph is not always the same from one to the next (SOPs). This is frequently the result of extremely minute shifts in technique that took place while the radiograph was being acquired. These shifts can have a significant impact on the appearance of the radiograph. This has an effect on linear measurements, but the effect that it has on angle measurements is much more muted. Measurements were taken of the mesio-distal widths of the lower central incisor, as well as the left and right mandibular second molars on both sides of the mouth. This was done so that a calibration factor could be generated between D1 and D2. This was done in an effort to reduce the amount of error that was present and calibrate the two panoramic radiographs that were taken of the same individual. Both of these radiographs were taken of the same person. Both of these have been accomplished in times gone by. These teeth were chosen because they, in order, represent the right side of the image, the left side of the image, and the center of the image.
Calibration of radiographic measurements
During the process of calculating the size of the sample, the angulation result from an earlier study that was connected to this one was utilized. Along with this, 88 percent power, a level of significance of 7 percent, and a clinically significant difference of 15 degrees in the M3 angulation were the other factors that were taken into consideration. It was decided that there would need to be a total of 48 mandibular M3s in each group, which would mean that there would need to be a total of 25 people in each group. This decision was reached after much deliberation.
Sampling
The angulation result from an earlier study that was connected to this one was utilized in the process of calculating the size of the sample. In addition to this, the other factors that were taken into consideration were an agreed-upon clinically significant difference of 15 degrees in the M3 angulation, 88 percent power, and a level of significance of 7 percent. It was decided that each group would need to have a total of 48 mandibular M3s, which would imply that there would need to be a total of 25 people in each group. This decision was made after much deliberation.
Data analysis
The angulation result from a related study was used in the calculation of the sample size, along with an agreedupon clinically significant difference of 15 degrees in the M3 angulation, a level of significance of 5 percent, and a power of 90 percent. It was decided that each group would need 20 individuals, which would result in each group having a total of 40 mandibular M3s. This decision was reached after much deliberation. Test known as the t-test or the Mann–Whitney U-test, according to whether or not the data follows a normal distribution. Multiple linear regressions were used to determine the factors that had an influence. These factors included ethnicity, the amount of time that had passed since the previous radiograph, the gender of the patient, whether the left or right side was being investigated, and whether or not the M1 had been removed.
Results
Sample flow
In order for the researchers to determine whether or not M1 was present in the bodies of the 33 participants who took part in the study, M1 had to be removed from their systems. The mandibular M1s of both of these patients, in addition to an associated developing M3, were simultaneously extracted from each of the 28 patients who were being researched. Both M1s were extracted from separate participants, but one of the sides did not have an associated M3; consequently, the side that did not have an associated M3 was omitted from the analysis. Both M1s were taken from different participants. Both M1s were taken from individuals who were not related to one another. Both M1s were obtained from separate participants in the study in order to isolate them. While one side of the equation kept both of its M1s, the other side of the equation had one M1 taken away from each of its three participants. In each of these three people's cases, the side that was extracted was counted as a member of the extraction group, while the side that was not extracted was counted as a member of the non-extraction group. In other words, the side that was extracted was considered a member of the extraction group. This distinction was made as a result of the fact that the part that was removed was utilized in the process of determining which group each individual belonged to. This distinction was made as a consequence of the fact that membership in the extraction group was determined based on the side that was extracted. As a consequence of this, this distinction was made. It was discovered that there were a total of 25 people who had never once in their lives had any of their mandibular first permanent molars extracted for any reason. This was the case despite the fact that all of these people had experienced tooth loss at some point in their lives. This was the case irrespective of the time period in these people's lives during which they had their teeth extracted. It was irrelevant at what point in their lives the extractions were performed because this was always the case. Even though they were supposed to be connected to one of these M1s, there was no indication of the M3s that were supposed to be there even though they should have been. There were a total of 60 M3s that were a part of the non-extraction group and had an M1 that was maintained, while there were 59 M3s that were a part of the extraction group and had an M1 that was eliminated. In the end, an M1 was isolated from one of 59 different M3s, bringing the total number of M3s utilized in this process up to 59 altogether. In the following table, the demographics of both the group that did extract their data and the group that did not extract their data are presented, in addition to the baseline data for each respective group (Tables 1 and 2). According to the results of the calibration, both the inter-rater and the intra-rater comparisons fell within a band that is considered to be clinically acceptable. This was the case regardless of which comparison was performed first. This was the situation with regard to comparisons that were carried out both internally and between the various raters. The total amount of the differences in the results that were obtained when the conditions were horizontal, vertical, and at an angle is able to be expressed as the following formula. The M3 began to go through the process of mesialization in the group that was extracted, and as a direct result of this, the angle increased by a significantly greater amount. There was no discernible difference in the horizontal and angle of M3 outcome between D1 and D2 in the group that did not undergo extraction. This was the case for the group that did not go through extraction. This was the situation for the population that did not undergo extraction procedures. This was the predicament that those members of the population were in who did not go through the extraction procedures. Those members of the population who did not go through the extraction procedures found themselves in this difficult situation. Despite the fact that this movement was seen in both D1 and D2 groups, there was no discernible difference between the groups in terms of the movement of the M3 from the ramus to the body of the mandible between D1 and D2 (Figures 4 to 6).
| Characteristics | Types | n. Percentages (%) |
|---|---|---|
| Groups | Total | 59 (100%) |
| Group of extraction | D1 | 34 (57.62%) |
| Group of non-extraction | D2 | 25 (42.37%) |
| Gender of Group of extraction | Male | 19 (52.94%) |
| Female | 16 (47.05%) | |
| Gender Group of non-extraction | Male | 14 (56%) |
| Female | 11 (44%) |
Table 1: Demographic data of study.
| Times of steps | Group of Extraction | Group of Non-extraction | P value |
|---|---|---|---|
| Radiographic age at the D1 level (years) | 8.35 ± 0.16 | 9.64 ± 0.85 | 0.761 |
| Age at the time of extraction (years) | 10.16 ± 1.2 | 9.12±0.21 | 0.654 |
| Age determined by the D2 radiograph (years) | 13.34 ± 1.33 | 12.17 ± 1.23 | 0.546 |
| The amount of time between radiographs D1 and D2. | 2.46 ± 1.21 | 3.19 ± 1.42 | 0.345 |
| The amount of time between radiograph D1 and extraction (months) | 5.45 ± 4.23 | 6.21 ± 2.22 | 0.123 |
| The amount of time between the extraction and the radiograph D1 (years) | 2.15 ± 1.05 | 3.25 ± 1.11 | 0.123 |
| The angle formed by the third molar and the intersigmoid line is denoted by D1. | 33.31± 11.71 | 32.12 ± 11.12 | 0.234 |
| The distance from the third molar to the horizontal midline, D1 | 1422.14 ± 342.24 | 1221.93 ± 393.21 | 0.465 |
| D1 is the vertical distance in pixels from the third molar to the intersigmoid line. | 505.17 ± 123.77 | 430.35 ± 175.18 | 0.353 |
Table 2: comparison between D1 and D2.
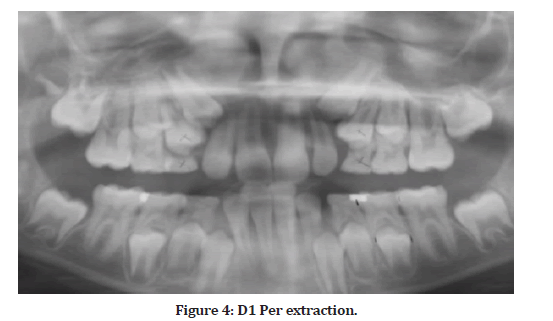
Figure 4: D1 Per extraction.
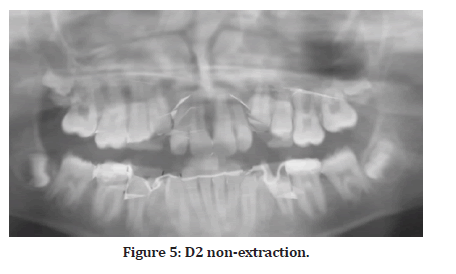
Figure 5: D2 non-extraction.
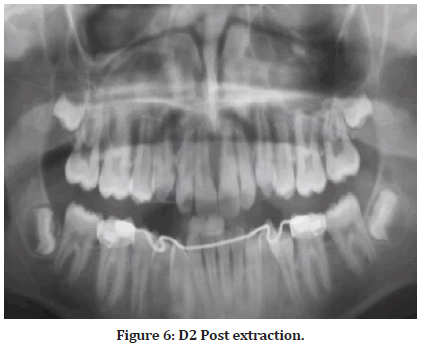
Figure 6: D2 Post extraction.
Discussion
This study found that removing the M1 from the developing mandible at age 7–10 medializes and uprights the developing M3 tooth. The study confirmed this effect. This change in M3 location may improve impaction pathology and subsequent eruption. Pathology may improve. Examining extraction and nonextraction cases illustrates this movement. The M3 has more mesial movement and stands upright than other extraction group members. Despite positive results, this study had flaws that needed to be fixed. Because this was a retrospective study, crowding or skeletal pattern could not be assessed. We couldn't get this information, which would have given us more about the participants' dental development. We regret any inconvenience. Multiple linear regressions showed no significant difference between the groups, but they were not exact matches. The study Given that the proportion of males and females, as well as people of different ages, was not the same, prospective research could have resolved this issue. Even with that design, exposing participants to additional graphical for research may have been difficult. Using a prospective method would have improved these results. This study's precision could have been improved by following patients until M3 eruption. This was an option. The results of this study suggest that it may be worthwhile to incur the costs of a similar longitudinal study [23]. Randomized controlled trials (RCTs) have not been conducted in this industry due to recruitment, ethics, and follow-up time. An earlier randomized controlled trial (RCT) failed to recruit enough participants [24]. Conventional radiographs can't provide the same level of radiographic analysis as panoramic radiographs, and panoramic radiographs can vary in magnification [25]. Panoramic radiographs can't be viewed like traditional ones. This differs from traditional radiographs [26]. However, they are often used to evaluate developing dentition, so their use in orthodontic assessment is justified [27]. These methods analyze developing teeth. Evaluating developing dentition. When determining significance, we think it's best to err on the side of caution [28]. This will eliminate the possibility of making a mistake and allow us to confirm any significant changes [29]. Because a tomography only produces a two-dimensional representation of a threedimensional object, measuring linear distances with it can be difficult. Tomography creates cross-sectional images of solids. Because panoramic radiographs lack a ruler, pixels are used to measure linear distances. Pixels are preciser than rulers. Both radiographs D1 and D2 will be magnification calibrated to ensure comparability and eliminate discrepancies. The inclusion of a magnification control and statistical analysis showed that the study's methodology was reliable. Example Despite including a magnification control, the magnification calibration used in this study was not accurate. In the non-extraction group, the horizontal distance between the M3 and midline shrunk by 0.85%, but it shrunk by 11.1% in the extraction group. The results show a significant difference. These differences were statistically clear [30]. Despite this, the finding suggests that the extraction mesializes M3 in its formative stages, which is consistent with the hypothesis [31]. A difference of 11.1% in M3 mesialization after M1 extraction may not be clinically significant may be a problem throughout product development [32]. Both the extraction and non-extraction groups showed a significant downward movement in the M3 vertical change. This went against expectations. Since the M3 moves from the ramus to the mandible during its formative stages, an early developing M3 exhibits this behavior. M3 migrates from the mandible's ramus. The M3 angle increased by 9.2 degrees in the extraction group, but only by 0.4 degrees in the control group. 14-degree difference was used to calculate sample size. Observing a significant angulation change over a short period of time may not be clinically significant at this stage. The study's design reflected this. This lends credibility to the evidence that M3s tend to stand upright and, with enough space, erupt without complications. In a prospective study with more participants, the disparity between the groups may grow over time. If a child's lower first permanent molar is extracted, the child's third permanent molar is less likely to become impacted in the future. Extraction makes room for the third permanent molar. The extraction makes room for the third molar. The article's findings support this conclusion [33]. In a patient with a poor prognosis, removing the first permanent molar could relieve the patient of long-term restorative work and prevent third permanent molar extraction pathology[34]. This could help patient and dentist. This alone wouldn't be enough to remove the first permanent molar. Despite that, treatment planning may take this into account [35].
Conclusion
In this particular experiment, removing the M1 from the growing dentition of the mandible between the ages of 7 and 10 resulted in a considerable medializing and up righting influence on the developing M3. Because of this, the future eruption may have a higher chance of being successful, and any pathology that was brought on by the impaction may no longer be required any longer. As a result of this, the second eruption may have a better chance of being successful.
References
- Roulias P, Kalantzis N, Doukaki D, et al. Teeth eruption disorders: A critical review. Children 2022; 9:771.
- Matsuda S, Yoshimura H. Maxillary third molars with horizontal impaction: A cross-sectional study using computed tomography in young Japanese patients. J Int Med Res 2022; 50.
- Saraiva Amaral J, Marto CM, Farias J, et al. A pilot randomized controlled clinical trial comparing piezo versus conventional rotary surgery for removal of impacted mandibular third molars. Bioengineering 2022; 9:276.
- Alwan AM, Afshari JT. In vivo growth inhibition of human caucasian prostate adenocarcinoma in nude mice induced by amygdalin with metabolic enzyme combinations. Biomed Res Int 2022.
- Alwan AM, Afzaljavan F, Tavakol Afshari J, et al. The impact of CYP19A1 variants and haplotypes on breast cancer risk, clinicopathological features and prognosis. Mol Genet Genomic Med 2021; 9:e1705.
- AlWadiyah M, Athanasiou AE, Makrygiannakis MA, et al. Does interceptive extraction of multiple primary teeth increase the chances of spontaneous eruption of permanent maxillary canines positioned palatally or centrally in the alveolar crest? A Systematic review. Int Orthod 2022; 20:100638.
- Philip L, D'Silva J, Martis E, et al. Alternate management of an anterior maxillary dentigerous cyst in a paediatric patient. Afr J Paediatr Surg 2022; 19:186.
- Siotou K, Kouskouki MP, Christopoulou I, et al. Frequency and local etiological factors of impaction of permanent teeth among 1400 patients in a greek population. Dent J 2022; 10:150.
- Salem MB, Chouchene F, Masmoudi F, et al. Are molar-incisor hypomineralization and hypomineralized second primary molars predictive of dental caries?: A systematic review. Eur J Dent 2022.
- Sbricoli L, Ricci S, Cattozzo A, et al. Mandibular molar uprighting using skeletal anchorage: A novel approach. J Clin Med 2022; 11:3565.
- Ng A, Ong D, Goh P. Management of a patient with a severely infraoccluded primary molar and hypodontia. Clin Case Rep 2022; 10:e6482.
- Azab M, Ibrahim S, Li A, et al. Efficacy of secondary vs primary closure techniques for the prevention of postoperative complications after impacted mandibular third molar extractions: A systematic review update and meta-analysis. J Am Dent Assoc 2022.
- Hong HR, Lee NK, Park JH, et al. Long-term cbct evaluation of mandibular third molar changes after distalization in adolescents. Appl Sci 2022; 12:4613.
- Davies S. Good occlusal practice in children’s dentistry. InA Guide to Good Occlusal Practice 2022. Cham: Springer International Publishing.
- Dhar S, Singh G, Mishra M, et al. A prospective study on autotransplantation of mandibular third molars with complete root formation. Craniomaxillofac Trauma Reconstr 2022; 15:340-349.
- Kuśnierek W, Brzezińska K, Nijakowski K, et al. Smoking as a risk factor for dry socket: A systematic review. Dent J 2022; 10:121.
- Ma Y, Mu D, Li X. Risk factors for root resorption of second molars with impacted third molars: a meta-analysis of CBCT studies. Acta Odontol Scand 2022; 1-1.
- Takahashi M, Tabuchi M, Sato T, et al. A modified hyrax-type expander is effective for distal bodily movement of the maxillary first molar. Appl Sci 2022; 12:7620.
- Eşian D, Bica CI, Stoica et al. Prevalence and Manifestations of Dental Ankylosis in Primary Molars Using Panoramic X-rays: A Cross-Sectional Study. Children 2022; 9:1188.
- Almarghlani A. Prevalence, predictors, and reasons for permanent tooth extraction among high school students in Saudi Arabia: a national cross-sectional study. Cureus 2022; 14.
- Shukla D, Bhola ND, Bhola RD, et al. Efficacy of preoperative piroxicam, diclofenac, paracetamol with tramadol and placebo tablets for relief of postoperative pain after the removal of impacted mandibular third molars: A randomised controlled trial. Cureus 2022; 14.
- Monaco G, Gatto MR, Pelliccioni GA. Incidence of delayed infections after lower third molar extraction. Int J Environ Res Public Health 2022 Mar; 19:4028.
- Küchler EC, Henklein SD, Proff P, et al. Single nucleotide polymorphisms in cox2 is associated with persistent primary tooth and delayed permanent tooth eruption. Int J Environ Res Public Health 2022; 19:10047.
- de Souza BB, da Silveira ML, Dantas WR, et al. Does the presence of third molars during sagittal split mandibular ramus osteotomy favour complications? Systematic review and meta-analysis. Int J Oral Maxillofac Surg 2022.
- Lenaker DC. Evaluation of Predictors of Spontaneous Space Closure and Supereruption after the Loss of First Permanent Molars.
- Murphy I, Noar J, Parekh S, et al. The effect of extraction of the lower first permanent molar on the developing third molar in children. J Orthod 2022; 49:480-487.
- Okawa R, Hamada M, Takagi M, et al. A case of x-linked hypophosphatemic rickets with dentin dysplasia in mandibular third molars. Children 2022; 9:1304.
- Lam PP, Chua H, Ekambaram M, et al. Does early childhood caries increase caries development among school children and adolescents? a systematic review and meta-analysis. Int J Environ Res Public Health 2022; 19:13459.
- Mahanta Sr P, Das K, Deka H, et al. Relationship between the eruption of third molar teeth and the growing status of the assamese inhabitants of a north-eastern state of india. Cureus 2022; 14.
- Ahmed AM, Jalil AT. Investigating the Protective Role of Rhodanese Enzyme Against Cyanide, the Cytotoxic by-product of Amygdalin. HDF and L929 Cell Lines. Lett Drug Des Discov 2022; 19.
- Alwan M, Afzaljavan F. Significance of the Estrogen Hormone and Single Nucleotide Polymorphisms in the Progression of Breast Cancer among Female. Arch Razi Inst 2022; 77:943.
- Enache AM, Feștilă D, Boboc F, et al. Root dilaceration and dentigerous cyst—a cause–effect relationship?—“case-series study”. Appl Sci 2022; 12:9854.
- Saraiva Amaral J, Marto CM, Farias J, et al. A pilot randomized controlled clinical trial comparing piezo versus conventional rotary surgery for removal of impacted mandibular third molars. Bioengineering 2022; 9:276.
- Castagna V, Pardo A, Lanaro L, et al. Periodontal healing after lower third molars extraction: A clinical evaluation of different flap designs. InHealthcare 2022.
- Chang CH, Chang CH, Lai JP, et al. Prevalence of dental anomalies in taiwanese children with cleft lip and cleft palate. J Pers Med 2022; 12:1708.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Dentistry Department, Kut University College, Iraq/Kut-Wasit, IraqCitation: Rusul A Alsaray, Correlation between the Extraction of Permanent Teeth in Children and Future Growth of Third Molar. J Res Med Dent Sci, 2023, 11(2):63-70.
Received: 01-Feb-2023, Manuscript No. jrmds-23-88716; Accepted: 03-Feb-2023, Pre QC No. jrmds-23-88716; Editor assigned: 03-Feb-2023, Pre QC No. jrmds-23-88716; Reviewed: 17-Feb-2023, QC No. jrmds-23-88716; Revised: 21-Feb-2023, Manuscript No. jrmds-23-88716; Published: 28-Feb-2023
