Research - (2022) Volume 10, Issue 2
Correlation between Tobacco Smoking and Dental Caries
Umayal S and Deepika Rajendran*
*Correspondence: Deepika Rajendran, Department of Oral Medicine and Radiology, Saveetha Institute of Medical and Technical Sciences Saveetha University, India, Email:
Abstract
Introduction: Tobacco is detrimental to human health. Tobacco contains nicotine, which is very harmful to health. Tobacco is a very harmful chemical. Dental caries is one of the most prevalent oral diseases. The association between tobacco smoking and dental caries has become an important research topic in recent years. Materials and method: A Retrospective institution based study was conducted by evaluating and analyzing 300 patients' records, visiting a dental hospital from Dec (2018) to Jan(2021) who were smokers and had dental caries. These were documented from an online database - DIAS, from a reputed institution, Chennai. Results: The Results were discussed and evaluated with help of SPSS Software and tabulated with help of excel sheets. Mostly, 80% of the analysis showed that there is correlation between tobacco smoking and dental caries. Conclusion: There is a correlation between tobacco smoking and dental caries.
Keywords
Tobacco smoking, Dental caries, Risk factors, Mortality
Introduction
Dental caries or tooth decay, is one of the most prevalent oral diseases [1,2]. Dental caries is a multifactorial disease, chronic infection and preventable. Dental caries is the primary focus of dental health prevention as it is one of the most prevalent chronic diseases [3,4]. Dental caries remains as a major global health problem that not only affects adults and school-age children but also the preschool children [5,6]. The severity of the dental caries and odontogenic infection varies from mild buccal space infection to severe multi space infection [7,8]. If not treated on time dental caries can cause progressive destruction of tooth hard tissue perforated into pulp leads to pulpitis and other pulpal inflammation [9,10].
Tobacco smoking is the practice of burning tobacco and ingesting the smoke that is produced [11,12]. Lung diseases are mostly due to Cigarette smoking [13,14]. Tobacco smoking is responsible for Oral conditions and many oral diseases [15,16]. The World health Organisation estimates that tobacco is responsible for oral diseases like adult periodontal diseases, oral cancer, cleft lip, palate and other congenital defects in children whose mothers smoked tobacco during pregnancy [17,18]. They lead to cardiovascular diseases, cancers and other systemic diseases [19,20]. According to the world health organisation (WHO) 7 million deaths and hundreds of billions of dollars of loss is only due to tobacco smoking [21,22]. The health consequences of smoking “50 years of progress”, update the evidence of infaust effect smoking health [23]. Iit is very hard to break this habit but it's necessary [24-26].
An increasing number of studies have focused on the association between tobacco smoking and dental caries [27-29]. Early in 1998, a cross-sectional epidemiology study in Sweden concluded that there was an association between smoking and oral health [30-32]. Later more trials emerged but the conclusion has not been consistent hence further studies are needed [33,34]. In the last five years no systematic review on this topic has been conducted [35,36].
People should stop the habit of smoking in the early time so that it does not develop into a consistent habit in future [37]. Children must be educated into various social programmes which creates an awareness about tobacco smoking and it's harmful effects.
There should be various public health programmes to be conducted in colleges and schools to make the people aware more about the harmful effects of smoking and tobacco chewing [38,39].
A University setting-based retroscope study has been designed to evaluate the association between tobacco smoking and dental caries. The hypothesis is that tobacco smoking is the risk factor for dental Caries. The aim of the present study is to correlate between tobacco smoking and dental caries.
Materials and Method
A Retrospective Institution based study was conducted by evaluating and analysing 300 patient case records visiting a dental hospital from December (2018) to January ( 2021) who were smokers and had signs of dental caries. Data such as age, gender, marital status, location, habit of smoking, dental caries, consumption of any other products like gutka, paan, were collected to categorize the patient.
These were documented from the online database of Saveetha dental college, DIAS, Dental Archiving Software. Ethical approval was obtained by the institution based at Saveetha university. The data was examined by 2 examiners. The data was reviewed and subjected to statistical analysis using IBM SPSS Software version 2.0.
The pros of this study is the available data and similar ethnicity. The cons of the study is the geographic imitation. There are two people ( 2 reviewers) involved in this study & the sample size was 300 case sheets of data from Dec (2018) to Jan (2021).
Eligibility criteria
• Original observational datas, that estimated the smokers and who all have dental caries.
• Analysed and evaluated previous related articles for better conclusion.
• Analysis and evaluation of the research statistically(statistical analysis).
Exclusion criteria
• Participants younger than 14 years of age.
• Non Smokers.
Search strategy and studies selection
The datas were collected from DIAS - software from online software belonging to The Dental College, Chennai with ethical and university approval.
Also, through electronic search was conducted in the database, PubMed, midline and google scholar to identify relevant research. The search string was (smoking or tobacco or tobacco smoking or tobacco products or cigarette smoking) and (Dental caries or Decayed tooth or caries). No data and language restrictions were applied in searching. The article was reviewed by 2 authors and were evaluated according to the inclusion and exclusion criteria. The final results were given statistically.
Data extraction
As mentioned here earlier, the data was extracted from the dental achieving software DIAS, a reputed institution Chennai. Ethical approval was obtained by the institutional ethical board at reputated insitution, Chennai. The data was analysed first with the number of smokers from December (2018) to January (2021) and who had dental caries. Among 75,000 data collected 300 were our sample size, who were smokers and had dental caries.
Excel tabulation was made, with the serial number, age, gender, clinical uses, location, reason for smoking and type of dental caries. The data was verified by 2 authors. There is no resolution of conflict and the sensor data is that there is a possibility of bias effects on the study and it was not included. The data was exported to SPSS software and there were no errors found.
Statistical analysis
The data was exported to SPSS software by IBM version 2.0. The data is coded using numbers in Excel sheet and the data is exported to SPSS software a frequency distribution was obtained. The Chi- square Test is done to compare differences between groups. The statistical analysis was done and the P value (p<0.05) was obtained. Thus obtained results, where explained in a pie chart or a Bar chart.
Independent variables : Age, Serial number, Gender, Location, Ethnicity.
Dependent Variables : Tobacco smoking, dental caries, types of dental caries.
Results
Around 700 smokers data was collected in which 300 or the patients who were smokers with dental problems were reviewed. The patients were grouped into males and females (Figure 1 to Figure 4).
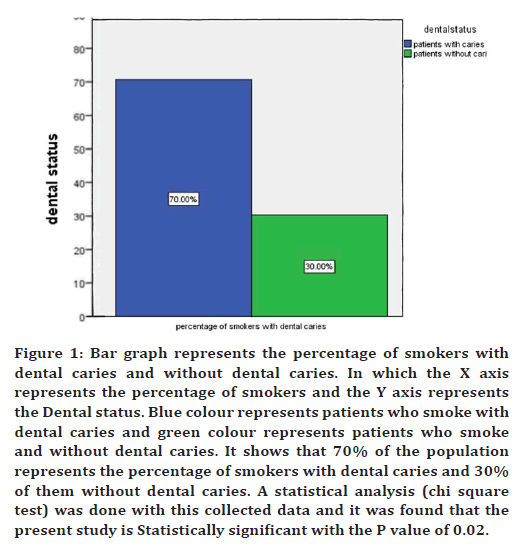
Figure 1. Bar graph represents the percentage of smokers with dental caries and without dental caries. In which the X axis represents the percentage of smokers and the Y axis represents the Dental status. Blue colour represents patients who smoke with dental caries and green colour represents patients who smoke and without dental caries. It shows that 70% of the population represents the percentage of smokers with dental caries and 30% of them without dental caries. A statistical analysis (chi square test) was done with this collected data and it was found that the present study is Statistically significant with the P value of 0.02.
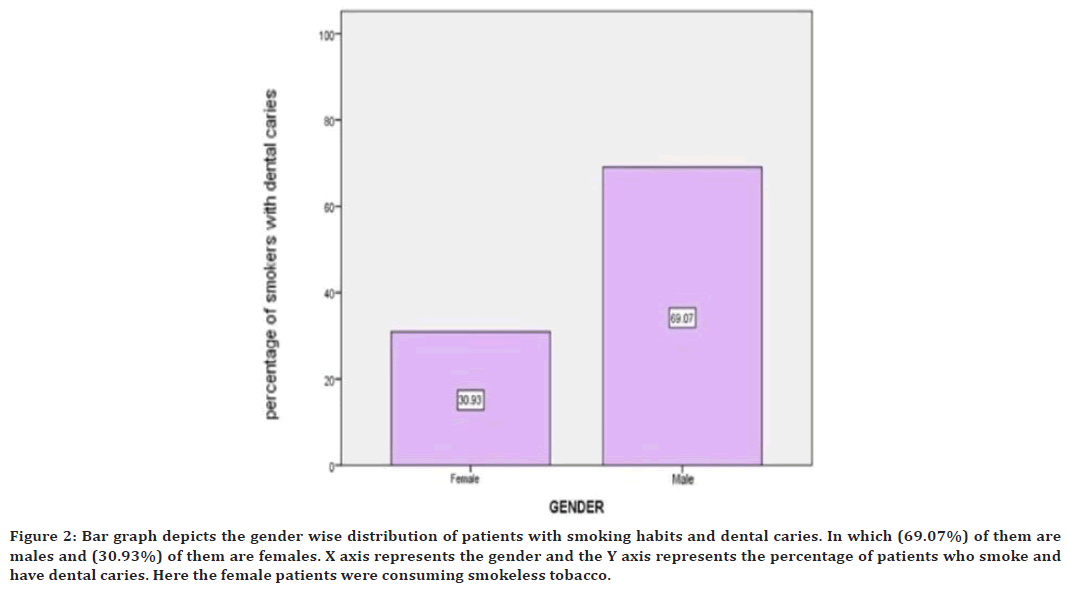
Figure 2. Bar graph depicts the gender wise distribution of patients with smoking habits and dental caries. In which (69.07%) of them are males and (30.93%) of them are females. X axis represents the gender and the Y axis represents the percentage of patients who smoke and have dental caries. Here the female patients were consuming smokeless tobacco.
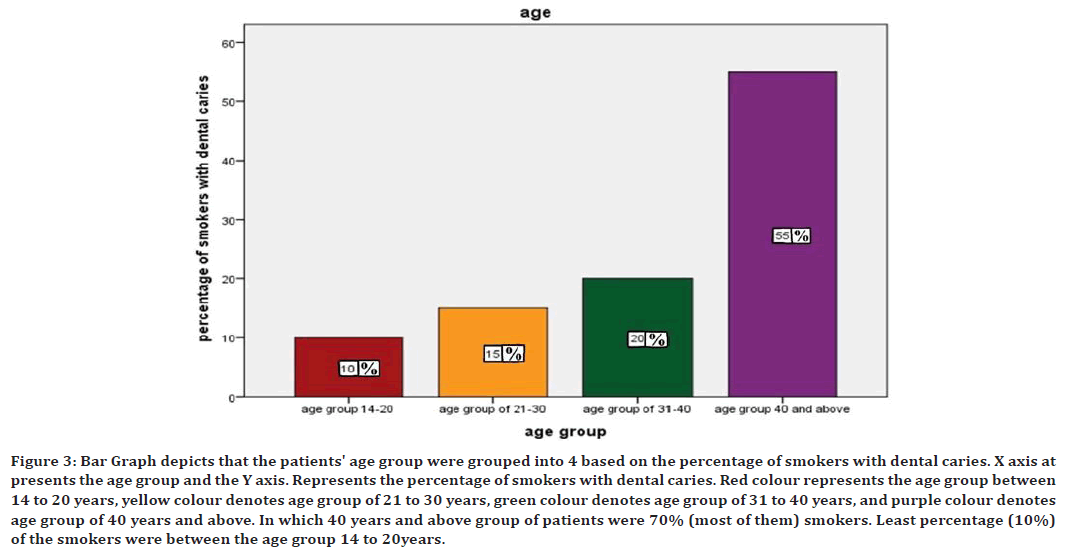
Figure 3. Bar Graph depicts that the patients' age group were grouped into 4 based on the percentage of smokers with dental caries. X axis at presents the age group and the Y axis. Represents the percentage of smokers with dental caries. Red colour represents the age group between 14 to 20 years, yellow colour denotes age group of 21 to 30 years, green colour denotes age group of 31 to 40 years, and purple colour denotes age group of 40 years and above. In which 40 years and above group of patients were 70% (most of them) smokers. Least percentage (10%) of the smokers were between the age group 14 to 20years.
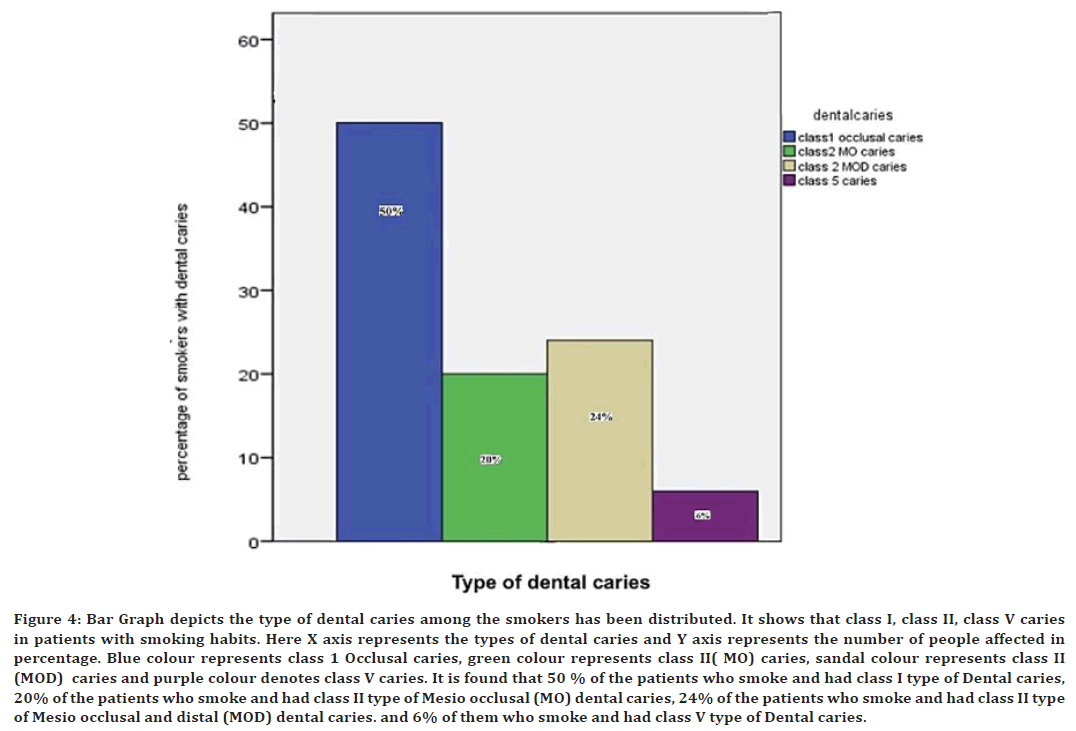
Figure 4. Bar Graph depicts the type of dental caries among the smokers has been distributed. It shows that class I, class II, class V caries in patients with smoking habits. Here X axis represents the types of dental caries and Y axis represents the number of people affected in percentage. Blue colour represents class 1 Occlusal caries, green colour represents class II( MO) caries, sandal colour represents class II (MOD) caries and purple colour denotes class V caries. It is found that 50 % of the patients who smoke and had class I type of Dental caries, 20% of the patients who smoke and had class II type of Mesio occlusal (MO) dental caries, 24% of the patients who smoke and had class II type of Mesio occlusal and distal (MOD) dental caries. and 6% of them who smoke and had class V type of Dental caries.
Discussion
The findings from the study indicate the existence of a relation between tobacco smoking and dental caries. For, most of the other studies reviewed the results that were consistent with the positive association [40]. Conflict to the study by Bernate, et.al [41] most of them were crosssectional and thus does not allow inferences to be made on casual relations. Affirmation of the aetiology of tobacco smoking was not possible. Therefore, there was insufficient evidence to confirm the hypothesis that tobacco is a factor and it's involved in the dental caries process [42].
The study conducted by Vellapathy et al. [43] assessed that the amount of smokers and non-smokers were not due to class I caries (MO). They concluded that there was no correlation between smoking and dental caries. However many studies proved that it is due to dental caries. Study conducted by, Rweyoni et al. [44] found that smoking adhesive was significantly enhanced in the presence of nicotine [45,46]. Have examined the effect of nicotine on how old are Microorganisms and human tissues. There is enough evidence of a link between smoking and caries.
Further, more research is needed to confirm the association between smoking and cariss of any bacteria growth [47]. Other studies have concluded with DMFS and DMFT analysis to prove the correlation between smoking and tobacco smoking [48]. As the research is done the author Jiing et al. [49,50] concluded the correlation between tobacco smoking and dental caries.
Conclusion
The present study reveals that there is correlation between tobacco smoking and dental caries. Within the limitations of this study, it is concluded that 80% of the smokers had dental caries. To further perspective, statistics and analysis value for this correlation between smoking and dental caries for significant P value was less than (>0.05) i.e., (0.02). Thus suggesting that tobacco smoking can lead to development of dental caries. Furthermore studies with a larger sample size are needed to find an association between types of dental caries and tobacco smoking.
References
- Health and Human Services Department. Let’s make the next generation tobacco-free: Your guide to the 50th anniversary surgeon general's report on smoking and health. Government Printing Office 2014; 24.
- PradeepKumar AR, Shemesh H, Nivedhitha MS, et al. Diagnosis of vertical root fractures by cone-beam computed tomography in root-filled teeth with confirmation by direct visualization: A systematic review and meta-analysis. J Endod 2021; 47:1198-1214.
- Raja M, Garg A, Yadav P, et al. Diagnostic methods for detection of cotinine level in tobacco users: A review. J Clin Diagn Res 2016; 10:ZE04.
- Mainali P, Pant S, Rodriguez AP, et al. Tobacco and cardiovascular health. Cardiovasc Toxicol 2015; 15:107-116.
- Petersen PE. The World Oral Health Report 2003: Continuous improvement of oral health in the 21st century–the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 2003; 31:3-24.
- Rajakumari R, Volova T, Oluwafemi OS, et al. Nano formulated proanthocyanidins as an effective wound healing component. Mater Sci Eng 2020; 106:110056.
- Rodgman A, Perfetti TA. The alphabetical index to components identified in tobacco, tobacco smoke, and tobacco substitute smoke. The Chemical Components of Tobacco and Tobacco Smoke, 2nd Edn. CRC Press: Boca Raton, FL 2013; 1713-2064.
- Mehta M, Dhanjal DS, Paudel KR, et al. Cellular signalling pathways mediating the pathogenesis of chronic inflammatory respiratory diseases: An update. Inflammopharmacol 2020; 28:795-817.
- Islam B, Khan SN, Khan AU. Dental caries: From infection to prevention. Med Sci Monit 2007; 13:RA196–203.
- Kaewkamnerdpong I, Krisdapong S. The associations of school oral health-related environments with oral health behaviours and dental caries in children. Caries Res 2018; 52:166-75.
- Laskin DM. Anatomie considerations in diagnosis and treatment of odontogenic infections. J Am Dent Assoc 1964; 69:308-316.
- Jayasree R, Kumar PS, Saravanan A, et al. Sequestration of toxic Pb (II) ions using ultrasonic modified agro waste: Adsorption mechanism and modelling study. Chemosphere 2021; 285:131502.
- Gupta P, Gupta N, Singh HP. Prevalence of dental caries in relation to body mass index, daily sugar intake, and oral hygiene status in 12-year-old school children in Mathura city: A pilot study. Int J Pediatr 2014; 2014.
- Sivakumar A, Nalabothu P, Thanh HN, et al. A comparison of craniofacial characteristics between two different adult populations with class II malocclusion—A cross-sectional retrospective study. Biology 2021; 10:438.
- Kaur P. Monitoring tobacco use and implementation of prevention policies is vital for strengthening tobacco control: An Indian perspective. Int J Public Health 2010; 55:229-30.
- Uma Maheswari TN, Nivedhitha MS, Ramani P. Expression profile of salivary micro RNA-21 and 31 in oral potentially malignant disorders. Brazilian Oral Res 2020; 34.
- Axelsson P, Paulartder J, Lindhe J. Relationship between smoking and dental status in 35‐, 50‐, 65‐, and 75‐year‐old individuals. J Clin Periodont 1998; 25:297-305.
- Sarode SC, Gondivkar S, Sarode GS, et al. Hybrid oral potentially malignant disorder: A neglected fact in oral submucous fibrosis. Oral Oncol 2021; 121:105390.
- Levi-Belz Y, Gvion Y, Apter A. The psychology of suicide: From research understandings to intervention and treatment. Frontiers Media SA 2019.
- Chaitanya NC, Muthukrishnan A, Rao KP, et al. Oral mucositis severity assessment by supplementation of high dose ascorbic acid during chemo and/or radiotherapy of oro-pharyngeal cancers: A pilot project. Indian J Pharm Educ Res 2018; 52:532–539.
- Stang A. Critical evaluation of the newcastle-ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25:603-605.
- Tejasvi MA, Maragathavalli G, Putcha UK, et al. Impact of ERCC1 gene polymorphisms on response to cisplatin based therapy in oral squamous cell carcinoma (OSCC) patients. Indian J Pathol Microbiol 2020; 63:538.
- Leite FR, Nascimento GG, Scheutz F, et al. Effect of smoking on periodontitis: A systematic review and meta-regression. Am J Preventive Med 2018; 54:831-841.
- Aguilar-Zinser V, Irigoyen ME, Rivera G, et al. Cigarette smoking and dental caries among professional truck drivers in Mexico. Caries Res 2008; 42:255-262.
- Kavarthapu A, Gurumoorthy K. Linking chronic periodontitis and oral cancer: A review. Oral Oncol 2021; 121:105375.
- Ezhilarasan D, Lakshmi T, Subha M, et al. The ambiguous role of sirtuins in head and neck squamous cell carcinoma. Oral Diseases 2021.
- Arheiam A, Omar S. Dental caries experience and periodontal treatment needs of 10-to 15-year old children with type 1 diabetes mellitus. Int Dent J 2014; 64:150-154.
- Rajeshkumar S, Menon S, Venkat Kumar S, et al. Antibacterial and antioxidant potential of biosynthesized copper nanoparticles mediated through Cissus arnotiana plant extract. J Photochem Photobiol 2019; 197:111531.
- Perumalsamy H, Sankarapandian K, Veerappan K, et al. In silico and in vitro analysis of coumarin derivative induced anticancer effects by undergoing intrinsic pathway mediated apoptosis in human stomach cancer. Phytomed 2018; 46:119-30.
- Shetty S, Nyamati SB, Mannava P, et al. Correlation between respiratory health and periodontal diseases in chhatisgarh population-a prospective cross-sectional study. J Adv Med Dent Sci Res 2016; 4:115.
- Gudipaneni RK, Alam MK, Patil SR, et al. Measurement of the maximum occlusal bite force and its relation to the caries spectrum of first permanent molars in early permanent dentition. J Clin Pediatr Dent 2020; 44:423-428.
- Chaturvedula BB, Muthukrishnan A, Bhuvaraghan A, et al. Dens invaginatus: A review and orthodontic implications. Br Dent J 2021; 345–50.
- Tanner T, Kämppi A, Päkkilä J, et al. Association of smoking and snuffing with dental caries occurrence in a young male population in Finland: A cross-sectional study. Acta Odont Scandinavica 2014; 72:1017-24.
- Sharma P, Mehta M, Dhanjal DS, et al. Emerging trends in the novel drug delivery approaches for the treatment of lung cancer. Chem Biol Interactions 2019; 309:108720.
- Tanner T, Päkkilä J, Karjalainen K, et al. Smoking, alcohol use, socioeconomic background and oral health among young Finnish adults. Community Dent Oral Epidemiol 2015; 43:406-414.
- Ezhilarasan D, Apoorva VS, Ashok Vardhan N. Syzygium cumini extract induced reactive oxygen species‐mediated apoptosis in human oral squamous carcinoma cells. J Oral Pathol Med 2019; 48:115-121.
- Preethi KA, Lakshmanan G, Sekar D. Antagomir technology in the treatment of different types of cancer. Epigenomics 2021; 13:481-484.
- Umayal S. Smoking prevalence and behaviour among college students in Chennai-A survey based study. Int J Pharm Res 2020; 12.
- Patil SR, Maragathavalli G, Ramesh DN, et al. Assessment of maximum bite force in pre-treatment and post treatment patients of oral submucous fibrosis: A prospective clinical study. J Hard Tissue Biol 2021; 30:211-216.
- Nakonieczna-Rudnicka M, Bachanek T. Number of Streptococcus mutansand Lactobacillus in saliva versus the status of cigarette smoking, considering duration of smoking and number of cigarettes smoked daily. Ann Agric Environ Med 2017; 24:396-400.
- Smoking O, Centers for Disease Control and Prevention. How tobacco smoke causes disease: The biology and behavioral basis for smoking-attributable disease: A report of the surgeon general. 2010; 704.
- Campus G, Cagetti MG, Senna A, et al. Does smoking increase risk for caries? A cross-sectional study in an Italian military academy. Caries Res 2011; 45:40-46.
- Vellappally S, Jacob V, Smejkalová J, et al. Tobacco habits and oral health status in selected Indian population. Central Eur J Public Health 2008; 16.
- Rwenyonyi CM, Muwazi LM, Buwembo W. Assessment of factors associated with dental caries in rural communities in Rakai District, Uganda. Clin Oral Investig 2011; 15:75-80.
- Alzayer YM, Gomez GF, Eckert GJ, et al. The impact of nicotine and cigarette smoke condensate on metabolic activity and biofilm formation of Candida albicans on acrylic denture material. J Prosthod 2020; 29:173-8.
- Wagenknecht DR, BalHaddad AA, Gregory RL. Effects of nicotine on oral microorganisms, human tissues, and the interactions between them. Curr Oral Health Rep 2018; 5:78-87.
- Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 2019; 10(ED000142).
- Jiang X, Jiang X, Wang Y, et al. Correlation between tobacco smoking and dental caries: A systematic review and meta-analysis. Tob Induc Dis 2019; 17:34.
- Zitterbart PA, Matranga LF, Christen AG, et al. Association between cigarette smoking and the prevalence of dental caries in adult males. General Dent 1990; 38:426-31.
- Golpasand Hagh L, Zakavi F, Ansarifar S, et al. Association of dental caries and salivary sIgA with tobacco smoking. Aust Dent J 2013; 58:219–223.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Umayal S and Deepika Rajendran*
Department of Oral Medicine and Radiology, Saveetha Institute of Medical and Technical Sciences Saveetha University, Chennai, IndiaReceived: 02-Jan-2022, Manuscript No. JRMDS-22-51092; , Pre QC No. JRMDS-22-51092 (PQ); Editor assigned: 04-Jan-2022, Pre QC No. JRMDS-22-51092 (PQ); Reviewed: 18-Jan-2022, QC No. JRMDS-22-51092; Revised: 25-Jan-2022, Manuscript No. JRMDS-22-51092 (R); Published: 01-Feb-2022
