Research - (2022) Volume 10, Issue 2
COVID-19 Fear and Generalized Anxiety among the Doctors Working in West Bengal, India
Anupam Nath Gupta1* and Paras Nath2
*Correspondence: Anupam Nath Gupta, Department of Pharmacology, North Bengal Medical College, India, Email:
Abstract
Introduction: Anxiety is rampant among people from all walks of life as a result of the current pandemic. Aim: The purpose of this study was to assess the generalized anxiety and fear caused by COVID-19 among doctors practicing in the West Bengal Province of India. Material and Methods: This was a cross-sectional descriptive study. Data were collected as per the snowball sampling technique. We utilized the previously validated Generalized Anxiety Disorder -7 (GAD-7) scale and fear of coronavirus (FCV-19S) scale in the current study. SPSS 21 was used for data analysis. Independent sample T-test and ANOVA and Pearson's correlation test were executed for data analysis. Results: Data of 204 doctors were analyzed. Mild, moderate, or severe level of anxiety was reported in 36.28% of the doctors. Mean anxiety among males and females was calculated 3.72 ± 4.615 and 3.97 ± 4.01, respectively. The mean score of FCV-19S among the doctors was reported 18.11 ± 5.09. According to the Independent T-test there was no significant difference in GAD-7 and FCV-19S scores between males and females (P>0.05). Doctors with 11-15 years of experience reported significantly higher fear. A significant and positive correlation between generalized anxiety and fear has been recorded. Conclusion: Because of the present pandemic, generalized anxiety and fear are present in some doctors practicing in the West Bengal province of India.
Keywords
COVID-19, Generalized Anxiety, Fear, Doctors
Introduction
The current COVID-19 pandemic has resulted in a concerning global fatality rate, with one out of every thousand health-care workers infected [1]. The multiresponses of this novel virus are expected to have had a significant impact on health-care workers' mental and physical health, particularly those on the front lines. Furthermore, the rate and extent of COVID-19 transmission among health-care and non-healthcare workers are alarming, with health-care workers facing unprecedented challenges. From both a psychological and a professional standpoint, most of them may not have been adequately prepared to deal with it. Because of the high risk of infection, the fear of spreading COVID-19 to their family members, and the stress of more work, healthcare workers are particularly vulnerable to COVID-19 [2].
The daily increase in COVID-19 cases reported around the world has necessitated the hiring of more health-care workers. As a result, because health care workers are at the forefront of COVID-19 management, this pandemic poses a significant occupational risk [3]. The rapid rise in COVID-19 cases among health-care patients has been linked to environmental contamination, health-care facility overcrowding, a lack of isolated room facilities, and a scarcity of personal protective equipment [4]. Similarly, the pandemic has had a physical and psychological impact on health-care workers. Studies reported that health-care workers treating and managing COVID-19 patients reported depression, stress, and anxiety [5].
In China, Que et al. investigated the psychological effects of COVID-19 on HCWs. Psychological issues plagued 56.59 percent of HCWs [6]. A study performed in Italy reported that anxiety, depression, and insomnia were prevalent in 46.04 percent, 44.37 percent, and 28.75 percent of the health-care workers, respectively [7]. Because of their current health-care system challenges, HCWs in developing countries are at a higher risk. Concerns about their level of preparedness, insufficient supplies of Personal Protective Equipment (PPE), quality assurance of such products, insufficient testing kits, and doubts about the kits' accuracy all have psychological effects on them [8].
Nonetheless, fears of COVID-19 infection, increased workload, epidemic stress, and socio-cultural detriment have all been linked to the psychological impact of COVID-19 on health care workers, especially medical doctors. Even after the outbreak, dangerous consequences such as anxiety, burnout, traumatic stress, and depressive syndromes have been linked to healthcare workers, indicating long-term significance
To ensure adequate health care and implement psychological stability strategies, it is critical to understand the psychological impact of the COVID-19 pandemic among doctors. In the current study, the psychological impact of COVID-19 on doctors working in West Bengal is assessed.
Methodology
This cross-sectional study was conducted in the middle of 2021, following vaccination completion among medical professionals.
The current study included doctors practicing in West Bengal, India, who hold the degrees of Bachelor in Medicine and Bachelor in Surgery (MBBS). House officers, Homeopathic Doctors, and Hakeem’s were not allowed to participate.
The researchers collected data using an online Google form and contacted participants through professional and personnel contacts using the convenience snowball technique and a messaging app (WHATSAPP).
After conducting a thorough literature review, the current study's survey instrument was created. Age, gender, experience, and Coronavirus infection status were all included in the demographic variables. Two previously validated, standardized, self-reported scales were used in this study: the Generalised Anxiety Disorder (GAD-7) [9] and the Fear of Corona Virus Scale (FCV-19S) [10]. The GAD-7 is a seven-item scale with a score range of 0 to 21. It's used to figure out how anxious, worried, restless, irritable, and afraid of the unknown a patient is. FCV-19S has a cut-off value of 16.5, and scores greater than this value have a substantial predictive power on anxiety disorders, health-related anxiety disorders, and post-traumatic stress disorder [11].
The sample size was calculated using RaoSoft. The current study's minimum sample size was calculated at 200 based on a 50% response rate, a 95% confidence interval, and a 6% margin of error, with a total number of MBBS doctors 20000. (www.raosoft.com).
SPPP 21 was used to analyze the data. We used the independent sample T-test, ANOVA, and Pearson's correlation. P-values of less than 0.05 were considered significant.
Results
In the analyzed data of 204 doctors from West Bengal Province, we found that 66.7% (n=136) were males and 33.3 % (n=68) were females. In this study, 54.9% (n=112) of doctors had an experience of 21 or more years.
Doctors with experience of 15-20 years were 42, 13.7% of the doctors had 11-15 years of experience, and 10.8% of the doctors had experience of up to 5 years. In the current study, 48.8% of the participants said that they were tested positive for SARS–Cov-2 (Table 1).
| Variable | Frequency | Percentage |
|---|---|---|
| Gender | ||
| N | % | |
| Male | 136 | 66.7 |
| Female | 68 | 33.3 |
| Total | 204 | 100 |
| Experience (In Years) | ||
| 1-5 | 22 | 10.8 |
| 11-15 | 28 | 13.7 |
| 15-20 | 42 | 20.6 |
| 21+ | 112 | 54.9 |
| Infected With SARS-CoV-2 | ||
| Yes | 98 | 48 |
| No | 80 | 39.2 |
| Maybe | 26 | 12.7 |
Table 1: Demographic characteristics
As per GAD-7, we found that 130 (63.72 %) doctors were in a state of minimal anxiety, and 74 (36.28%) of the doctors were either in a mild, moderate, or severe state of anxiety (Figure 1).
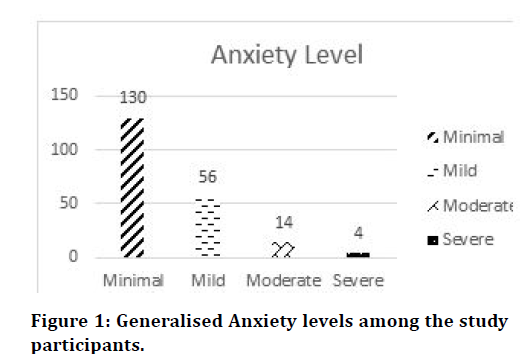
Figure 1.Generalised Anxiety levels among the study participants
The cut-off score of FCV-19 is 16.5. We have observed that 61.76 % (n=126) of the doctors are above the cut-off score. The mean score of FCV-19S is reported as 18.11 ± 5.09 (Figure 2).
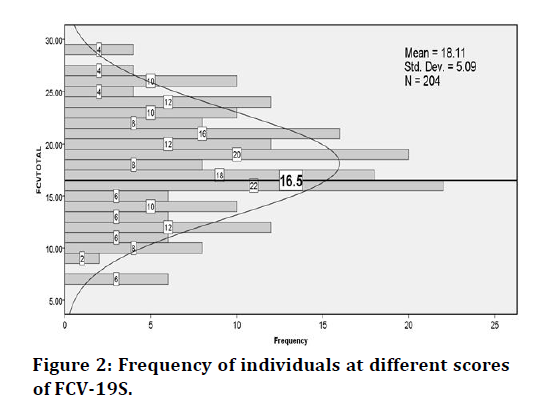
Figure 2.Frequency of individuals at different scores of FCV-19S
This fear score is higher than the cut off value that is 16.5 in both groups (Table 2).
| Male | Females | |
|---|---|---|
| Fear of Covid-19 | ||
| Mean ± SD | 17.79 ± 4.82 | 18.73 ± 5.56 |
| T-Score | -1.247 | |
| P Value | 0.214 | |
| General Anxiety Disorder | ||
| Mean ± SD | 3.72 ± 4.61 | 3.97 ± 4.01 |
| T-Score | -0.38 | |
| P Value | 0.704 | |
Table 2: Difference of fear and anxiety among males and females
As per FCV-19s, we found no significant difference between male and female doctors [t = -1.247, P=0.214]. The mean fear score of male and female doctors was reported 17.79 ± 4.827 and 18.73 ± 5.562, respectively.
As per ANOVA, we find a significant difference of fear in doctors with varied experience levels (F=2.825, P=0.040). The doctors with experience levels of 11 years to 15 years reported a mean FCV-19S score of 20.21 ±4.886, and doctors with 1-10 years of experience showed a mean score of 17.00 ± 3.491. Furthermore, we found no significant difference in GAD-7 scores among doctors with different experience levels (F=0.099, P=0.960) (Table3).
| Fear Of Covid-19 | Generalized Anxiety | ||||
|---|---|---|---|---|---|
| Experience | N | Mean ± SD | F- Score , P value | Mean ± SD | F- Score , P value |
| 1-10 Years | 22 | 17.00 ± 3.491 | 2.825, 0.040 | 3.90 ± 3.963 | 0.099, 0.960 |
| 11-15 Years | 28 | 20.21 ± 4.886 | 4.00 ± 4.586 | ||
| 15-20 Years | 42 | 18.85 ± 5.116 | 4.09 ± 3.518 | ||
| 21 Years + | 112 | 17.51 ± 5.260 | 3.69 ± 4.771 | ||
| Total | 204 | 18.10 ± 5.090 | 3.84 ± 4.404 | ||
Table 3: Difference of fear and anxiety among doctors of different experience levels
No significant difference in fear and anxiety has been observed among the previously infected doctors (P>0.05). However, we found more fear among the SARSCoV- 2 infected doctors (Table 4).
| Infected with SARS-COV-2 | Fear Of Covid-19 | Generalized Anxiety | |||
|---|---|---|---|---|---|
| N | Mean | F- Score , P value | Mean | F- Score , P value | |
| Yes | 98 | 18.53 | 1.710, 0.183 | 3.75 | 0.169 , 0.845 |
| No | 80 | 18.12 | 4.05 | ||
| May be | 26 | 16.46 | 3.53 | ||
| Total | 204 | 18.1 | 3.84 | ||
Table 4: Difference of fear and anxiety among the SARS-COV-2 Infected and non-infected doctors
Furthermore, by executing the Pearson Correlation test, we found a significant positive correlation between fear and anxiety (r=0.454, P<0.001).
Discussion
In the current study, we have evaluated the anxiety and fear among the doctors practicing in West Bengal, India. During the COVID-19 pandemic, health-care professionals around the globe suffered from severe anxiety, stress, depression, and fear [12,13].
It is reported that during the SARS-CoV-2 outbreak, excessive workload, hostile conditions, and aggravated psychological pressure, even mental illness [14].
Doctors are always in close contact with the patient and are associated with infection prevention, infection control, disease management, isolation, take care, containment, and public health [15].
In such a situation, health-care professionals are the frontline, and they risk their as well the lives of their loved ones. Being isolated, working in high-risk positions, and having contact with infected people are common causes of stress and trauma [16].
In the current study, we found that majority of the doctors reported minimal anxiety. And only 2% of doctors reported severe anxiety. Previous studies reported higher levels of anxiety among health-care professionals [17,18].
This study is performed when the majority of the health-care professionals in India have been vaccinated. In our opinion, vaccination could be the cause of less anxiety among the doctors. A recent study also supports our observation [19].
According to the results of the current study, fear among doctors is still prevalent. We observed that more than 60% of the doctors are above the cut-off values of FCV-19s. Previous studies reported a much higher rate of fear among doctors [20,21]. Recent studies also reported a reduction of fear among the health-care workers but still, this fear is affecting the lives of Healthcare professionals [22].
We found that Fear and Anxiety is more common among females. Other studies also reported higher fear and anxiety among females [23,24].
Furthermore, doctors with 11-15 years of experience reported more fear. In our opinion, these doctors are in their mid-thirties and have small children and old parents. Moreover, the workload on them is particularly higher as compared to fresh graduates and seniors.
In the current study, nearly 50% of the doctors mentioned that they were tested positive for coronavirus. Studies have also reported a high prevalence of infection among doctors and health-care professionals [9,25].
Doctors are always in close contact with the patient and are associated with infection prevention, infection control, disease management, isolation, take care, containment, and public health [15].
This study is only addressing the doctors of the West Bengal province of India. Studies on larger scales should be performed to find out the mental health of the doctors working in India.
Conclusion
The doctors are the backbone of the health-care system. After vaccination, their anxiety and level of fear have been reduced but still considerable. Proper psychological sessions should be organized, and where required psychiatric help is provided.
Acknowledgment
We want to Acknowledge Dr. Sibasis Bandhopadyay, Consultant Psychiatrist, Basirhat District Hospital, West Bengal, India, for his support and guidance for this project. We want to thank all the doctors who participated in this study.
References
- Bandyopadhyay S, Baticulon RE, Kadhum M, et al. Infection and mortality of health-care workers worldwide from COVID-19: A systematic review. BMJ Global Health 2020; 5:e003097.
- Cabarkapa S, Nadjidai SE, Murgier J, et al. The psychological impact of COVID-19 and other viral epidemics on frontline health-care workers and ways to address it: A rapid systematic review. Brain Behav Immunity Health 2020; 100144.
- Mhango M, Dzobo M, Chitungo I, et al. COVID-19 risk factors among health workers: A rapid review. Safety Health Work 2020; 11:262-265.
- Itodo GE, Enitan SS, Oyekale AO, et al. COVID-19 among health-care workers: risk of exposure, impacts and biosafety measuresâ??A review. Int J Health Safety Environ 2020; 6:534-548.
- Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by health-care workers due to the COVID-19 pandemicâ??A review. Asian J Psychiatr 2020; 51:102119.
- Que J, Le Shi JD, Liu J, et al. Psychological impact of the COVID-19 pandemic on health-care workers: A cross-sectional study in China. General Psychiatr 2020; 33.
- Lasalvia A, Bonetto C, Porru S, et al. Psychological impact of COVID-19 pandemic on health-care workers in a highly burdened area of north-east Italy. Epidemiol Psychiatr Sci 2021; 30.
- Chandra A, Vanjare H. Coping by the health-care workers during COVID-19 pandemic in developing countries-A review. Anaesthesia, Pain Intensive Care 2020; 24:346-53.
- Morgantini LA, Naha U, Wang H, et al. Factors contributing to health-care professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PloS One 2020; 15:e0238217.
- Ahorsu DK, Lin CY, Imani V, et al. The Fear of COVID-19 scale: Development and Initial Validation. Int J Mental Health Addiction 2020; 1-9.
- Nikopoulou V, Holeva V, Parlapani E, et al. Mental health screening for COVID-19: A proposed cut off score for the Greek version of the fear of COVID-19 scale (FCV-19S). Int J Mental Health Addic 2020; 1-14.
- Alwani SS, Majeed MM, Ramzan Z, et al. Evaluation of knowledge, practices, attitude, and anxiety of nurses towards COVID-19 during the current outbreak in Karachi, Pakistan. Pakistan J Public Health 2020; 10:82-90.
- Repon MAU, Pakhe SA, Quaiyum S, et al. Effect of COVID-19 pandemic on mental health among Bangladeshi health-care professionals: A cross-sectional study. Sci Progress 2021; 104:00368504211026409.
- Verma S, Mythily S, Chan Y, et al. Post-SARS psychological morbidity and stigma among general practitioners and traditional Chinese medicine practitioners in Singapore. Ann Acad Med Singapore 2004; 33:743-748.
- Smith GD, Ng F, Li WHC. COVID-19: Emerging compassion, courage and resilience in the face of misinformation and adversity. J Clin Nurs 2020; 29:1425.
- Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav Immunity 2020.
- Bansal A, Jain S, Sharma L, et al. A cross-sectional study to assess the psychosocial impact of COVID-19 pandemic on health-care workers at a tertiary care hospital in India. Int J Academic Med 2020; 6:197.
- Mishra S, Singh S, Tiwari V, et al. Assessment of level of perceived stress and sources of stress among dental professionals before and during the COVID-19 outbreak. J Int Society Preven Community Dent 2020; 10:794.
- Karayürek F, �ebi AT, Gülses A, et al. The Impact of COVID-19 vaccination on anxiety levels of turkish dental professionals and their attitude in clinical care: A cross-sectional study. Int J Environ Res Public Health 2021; 18:10373.
- George CE, Inbaraj LR, Rajukutty S, et al. Challenges, experience and coping of health professionals in delivering health-care in an urban slum in India during the first 40 days of COVID-19 crisis: A mixed method study. BMJ Open 2020; 10:e042171.
- Nanjundaswamy MH, Pathak H, Chaturvedi SK. Perceived stress and anxiety during COVID-19 among psychiatry trainees. Asian J Psychiatr 2020; 54:102282.
- Bener A, Bhugra D, Ventriglio A. Mental health and quality of life of frontline health care workers after one year of Covid-19 pandemic. Acta Medica Transilvanica 2021; 26:6-11.
- Reizer A, Koslowsky M, Geffen L. Living in fear: The relationship between fear of COVID-19, distress, health, and marital satisfaction among Israeli women. Health Care Women Int 2020; 41:1273-1293.
- Gupta S, Prasad AS, Dixit PK, et al. Survey of prevalence of anxiety and depressive symptoms among 1124 health-care workers during the coronavirus disease 2019 pandemic across India. Med J Armed Forces India 2021; 77:S404-S12.
- Crespo J, Fernández Carrillo C, Iruzubieta P, et al. Massive impact of coronavirus disease 2019 pandemic on gastroenterology and hepatology departments and doctors in Spain. J Gastroenterol Hepatol 2021; 36:1627-33.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Anupam Nath Gupta1* and Paras Nath2
1Department of Pharmacology, North Bengal Medical College, India2Medical Officer, Siliguri District Hospital, India
Received: 03-Jan-2022, Manuscript No. JRMDS-22-49106; , Pre QC No. JRMDS-22-49106 (PQ); Editor assigned: 05-Jan-2022, Pre QC No. JRMDS-22-49106 (PQ); Reviewed: 19-Jan-2022, QC No. JRMDS-22-49106; Revised: 25-Jan-2022, Manuscript No. JRMDS-22-49106 (R); Published: 01-Feb-2022
