Research - (2022) Volume 10, Issue 1
Current Trends in Antibiotics Prescription Following Dental Implant Placement: A Hospital Based Assessment
Subasree Soundarajan and Priya lochana Gajendran*
*Correspondence: Priya lochana Gajendran, Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, Tamil Nadu, India, Email:
Abstract
Aim: The aim of the study is to assess the antibiotics preferred following implant placement in the hospital set up in Saveetha Institute of Medical & Technical Science (SIMATS). Materials & method: This hospital based study was carried out by retrospective analysis of the data from the patient records. Patient records from June 2019 to March 2020 were assessed. 574 patient records were studied. Parameters assessment: A) Demographic details-Patient Name, Patient Identity number (PID no.), Age, Sex, Medical history, (B) Implant parameters-Implant site, type of implant procedure (Single versus multiple implants), bone grafting procedures, (C) Antibiotic parameters - Drug of choice & dosage of antibiotics prescribed. Chi square tests were performed to assess the relationship between antibiotics with systemic status, single versus multiple implants, and bone grafting procedures. Results: A total of five hundred and seventy four patients have undergone dental implant placements. Around 1269 implants were placed. Most commonly prescribed antibiotic was Amoxicillin 500 mg (80.84%), followed by combination of amoxicillin 500 mg and metronidazole 400 mg (Flagyl) (13.94%), combination of amoxicillin & clavulanic acid 625 mg (Augmentin) (4.53%), followed by combination of Flagyl 400 mg and Augmentin 625 mg (0.7%). Chi square tests showed no statistically significant relationship between the antibiotic prescribed and systemic status of the patients, single versus multiple implants & bone grafting procedures. Conclusion: According to this hospital based study, the most commonly prescribed post-operative antibiotic following implant placement is Amoxicillin 500 mg. Based on our study observations, there is no statistically significant relationship between the type of antibiotic prescribed and systemic status of the patients, single versus multiple implants & bone grafting procedures. Clinical significance: Antibiotic resistance has become a serious threat globally. Dentists prescribe about 7-11% of all common antibiotics. Hence it is important to study the current trends in antibiotics prescription following dental implant placement, and design a protocol for the same.
Keywords
Antibiotics, Amoxicillin, Dental implants, Antibiotic prophylaxis, Infection
Introduction
After tooth loss, patients may seek tooth replacement to restore their function and esthetics. Conventional options for replacing a missing tooth include removable partial dentures, fixed partial dentures, and complete dentures. In recent days, dental implants have become an integral part of prosthetic rehabilitation [1,2]. They are considered to be an important contribution to dentistry with a high success rate. Dental implants have gained increasing popularity over the past few decades as they have the ability to restore the function to mimicking natural dentition in terms of mastication, speech and aesthetics [3,4].
The success of the dental implant is influenced by the ability of the implant to integrate with the surrounding bone [5]. Complications after implant placement can be classified as mechanical and biological complications. Biological failures include postoperative infections, accumulation of plaque, and peri implant bone loss. Biological complications are subcategorized into early and late implant failures. Early failures occur when surgical implants are placed under improper aseptic conditions and the late complications are typically peri-implantitis and infections caused by bacterial plaque [6]. Various predisposing factors play a vital role in the success and survival of dental implants. Predisposing conditions include uncontrolled diabetes mellitus, smoking, uncontrolled periodontitis, prolonged steroid therapy, radiation therapy, and chemotherapeutics. In order to prevent these biological complications, antibiotics are prescribed as prophylaxis and post-surgery.
Periodontitis occurs due to gram negative bacteria, resulting in release of pro inflammatory cytokines [7–10] and are more prone for peri implantitis. Antibiotics play a crucial role in the post-operative healing following implant placement, especially when implants are placed in medically compromised and in periodontitis patients [11–13]. A number of authors have reported that systemic antibiotics do not reduce implant failure rate [14–16]. The role of antibiotic use & its effect on implant failure & post-operative infection are still unclear. Antibiotic overuse has a negative impact on general health. Proper selection of antibiotic regimen in clinical practice is very important [17]. The use of antibiotics in implant surgery in healthy patients & it’s correlation to failure remain poorly documented in the literature. It is widely agreed by health care providers that overall use of antibiotics should be reduced, & antibiotics should be prescribed only in severe infections to reduce the emergence of resistant bacterial strains [18]. It is therefore necessary to scrutinize the concept of routine antibiotic administration following implant placement in systemically healthy patients.
Dental practitioners are faced with a dilemma when prescribing antibiotics for patients undergoing implant procedure. Few studies showed that antibiotic use in healthy patients as a prophylactic drug did not improve the clinical outcome [19–21]. So, practitioners should avoid antibiotic abuse. They should follow the principles of antibiotic stewardship. A proficient clinician would prescribe antibiotics after thorough examination & determine the need on a case by case basis. It is still debated whether implant failure can be reduced by antibiotics. There are concerns associated with widespread use of antibiotics, since adverse effects may occur [22]. Previously our department has published extensive research on various aspects of prosthetic dentistry [23–32]; this vast research experience has inspired us to research this topic. No previous studies have been done to assess the complete antibiotic regimen following implant placement. Thus, the aim of the study is to assess the antibiotics preferred following implant placement in the hospital set up in Saveetha Institute of Medical & Technical science (SIMATS), Chennai.
Materials and Method
This is a retrospective study, carried out by analysis of the implant patient records from June 2019 to March 2020 of Saveetha dental college. The Data from six hundred patients who underwent dental implant placement at Saveetha Institute of Medical and Technical Sciences (SIMATS) were reviewed in the study. The study design was reviewed and approved by the Ethical Committee of Saveetha Institute of Medical and Technical Sciences (Ethical approval number. DC/SIHEC/2020/ DIASDATA/069-0320).Case sheets with incomplete data were excluded from the study. A total of five hundred and seventy four patients were included in the study.
Demographic details including Patient name, Patient identity number (PID No.), Age, Sex, and systemic status were recorded. Dental implant parameters including the implant site, type of implant placement procedure (Single versus multiple implants), & bone grafting procedures were analysed. Antibiotic parameters including the drug of choice and dosage of the antibiotics prescribed were taken into account in this study.
Statistical analysis
The distribution of antibiotics after implant placement, in healthy versus systemically compromised patients, in Single versus multiple implant placement, after bone grafting procedures were expressed in terms of percentage (%). Chi square tests were performed to assess the relationship between antibiotics with systemic status, single versus multiple implants, and bone grafting procedures. Statistical significance was set at p<0.05.All analyses were conducted with a statistical software SPSS version 23.0 (Statistical Package for the Social Sciences).
Results
A total of five hundred and seventy four patients have undergone dental implant placement. Males constituted 59.4% of the study population & females constituted 40.6% of the study population (Figure 1). Around 1269 implants were placed. 279 patients had single implant placement (48%), whereas 297 patients had multiple implants placement (52%). Most commonly prescribed antibiotic was Amoxicillin 500 mg (80.84%), followed by combination of amoxicillin 500 mg and metronidazole 400 mg (Flagyl) (13.94%), combination of amoxicillin & clavulanic acid 625 mg (Augmentin) (4.53%), followed by combination of Flagyl 400 mg and Augmentin 625 mg (0.7%) (Figure 2).
Figure 1: Pie chart representing the gender distribution among patients who underwent implant placement. Red denotes males and blue denotes females. 59.41% of the study population were males and 40.59% of the study population were females.
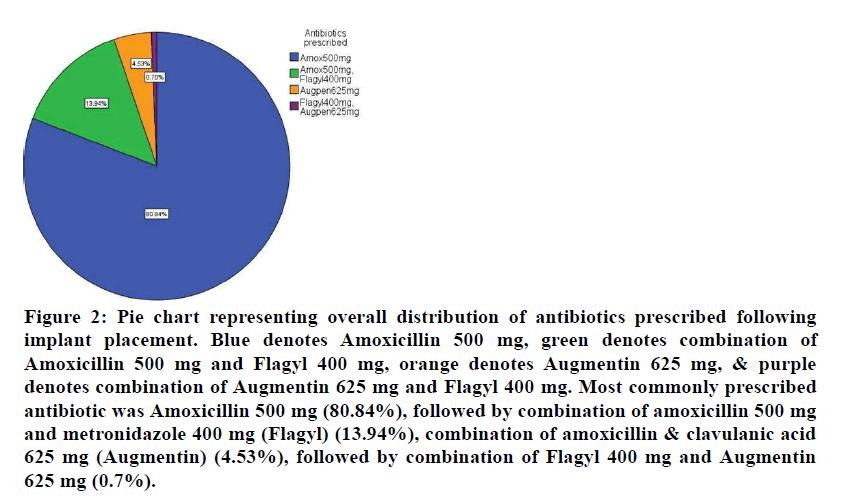
Figure 2: Pie chart representing overall distribution of antibiotics prescribed following implant placement. Blue denotes Amoxicillin 500 mg, green denotes combination of Amoxicillin 500 mg and Flagyl 400 mg, orange denotes Augmentin 625 mg, & purple denotes combination of Augmentin 625 mg and Flagyl 400 mg. Most commonly prescribed antibiotic was Amoxicillin 500 mg (80.84%), followed by combination of amoxicillin 500 mg and metronidazole 400 mg (Flagyl) (13.94%), combination of amoxicillin & clavulanic acid 625 mg (Augmentin) (4.53%), followed by combination of Flagyl 400 mg and Augmentin 625 mg (0.7%).
Table 1 represents the distribution of antibiotics in healthy patients versus systemically compromised patients. Among systemically healthy patients, 383 patients were prescribed with amoxicillin 500 mg (66.72%), 67 patients were prescribed with a combination of amoxicillin 500 mg and Flagyl 400 mg (11.67%), 22 patients were prescribed with Augmentin 625 mg (3.83%) & 1 patient was prescribed with a combination of Augmentin 625 mg & Flagyl 400 mg (0.17%) following implant placement.
| Antibiotics prescribed | Systemic status | |
|---|---|---|
| Systemically healthy patients | Systemically compromised patients | |
| Amoxicillin 500 mg | 383 (66.72%) | 81 (14.11%) |
| Amoxicillin 500 mg + Flagyl 400 mg | 67 (11.67%) | 13 (2.26%) |
| Augmentin 625 mg | 22 (3.83%) | 4 (0.7%) |
| Augmentin 625 mg + Flagyl 400 mg | 1 (0.17%) | 3 (0.52%) |
| Pearson Chi square value | 3.24 | |
| P value for Chi square test | 0.26-not statistically significant | |
Table 1: Distribution of antibiotics in healthy versus systemically compromised patients.
Among systemically compromised patients, 81 patients were prescribed with amoxicillin 500 mg (14.11%), 13 patients were prescribed with a combination of amoxicillin 500 mg and Flagyl 400 mg (2.26%), 4 patients were prescribed with Augmentin 625 mg (0.7%) & 3 patients were prescribed with a combination.
Augmentin 625 mg & Flagyl 400 mg (0.52%) following implant placement. Chi square test showed no statistically significant relationship between antibiotics prescribed and systemic status of the patients with a p value of 0.26 (Figure 3).
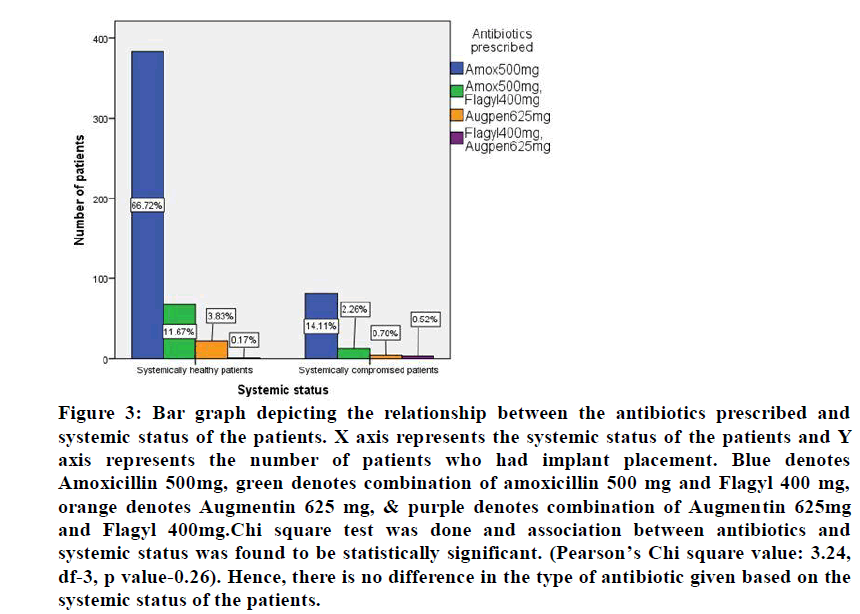
Figure 3:Bar graph depicting the relationship between the antibiotics prescribed and systemic status of the patients. X axis represents the systemic status of the patients and Y axis represents the number of patients who had implant placement. Blue denotes Amoxicillin 500mg, green denotes combination of amoxicillin 500 mg and Flagyl 400 mg, orange denotes Augmentin 625 mg, & purple denotes combination of Augmentin 625mg and Flagyl 400mg.Chi square test was done and association between antibiotics and systemic status was found to be statistically significant. (Pearson’s Chi square value: 3.24, df-3, p value-0.26). Hence, there is no difference in the type of antibiotic given based on the systemic status of the patients.
Distribution of antibiotics after single versus multiple implants was tabulated in Table 2. For single implant placement, 226 patients (39.4%) were prescribed with amoxicillin, 40 patients (7%) were prescribed with combination of amoxicillin 500 mg and Flagyl 400 mg, 12 patients (2.1%) were prescribed with Augmentin 625 mg, and 1 patient (0.2%) was given combination of Augmentin 625 mg and Flagyl 400 mg. For multiple implants placement, 238 patients (41.5%) were prescribed with amoxicillin, 40 patients (7%) were prescribed with combination of amoxicillin 500 mg and Flagyl 400 mg, 14 patients (2.4%) were prescribed with Augmentin 625 mg, and 3 patients (0.5%) were given combination of Augmentin 625 mg and Flagyl 400 mg.
| Antibiotics prescribed | Single versus multiple implants | |
|---|---|---|
| Single implant | Multiple implants | |
| Amoxicillin 500 mg | 226 (39.4%) | 238 (41.5%) |
| Amoxicillin 500 mg + Flagyl 400 mg | 40 (7%) | 40 (7%) |
| Augmentin 625 mg | 12 (2.1%) | 14 (2.4%) |
| Augmentin 625 mg + Flagyl 400 mg | 1 (0.2%) | 3 (0.5%) |
| Pearson Chi square value | 1.01 | |
| P value for Chi square test | 0.797 - not statistically significant | |
Table 2: Distribution of antibiotics in single versus multiple implants placement.
Chi square test showed no statistical significant relationship between antibiotics prescribed and single versus multiple implants placement, with a p value of 0.797 (Figure 4).
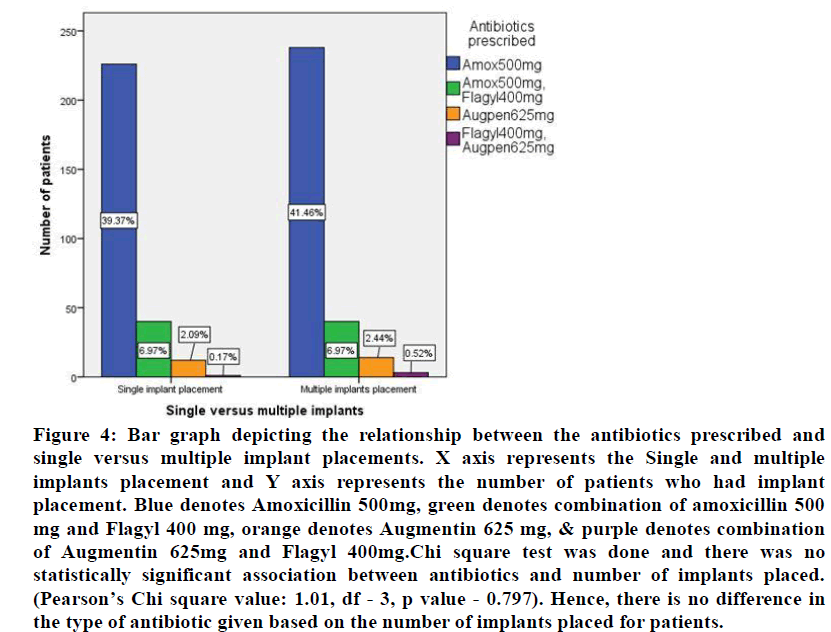
Figure 4:Bar graph depicting the relationship between the antibiotics prescribed and single versus multiple implant placements. X axis represents the Single and multiple implants placement and Y axis represents the number of patients who had implant placement. Blue denotes Amoxicillin 500mg, green denotes combination of amoxicillin 500 mg and Flagyl 400 mg, orange denotes Augmentin 625 mg, & purple denotes combination of Augmentin 625mg and Flagyl 400mg.Chi square test was done and there was no statistically significant association between antibiotics and number of implants placed. (Pearson’s Chi square value: 1.01, df - 3, p value - 0.797). Hence, there is no difference in the type of antibiotic given based on the number of implants placed for patients.
Distribution of antibiotics after bone grafting procedures was tabulated in Table 3. A total of 18 patients had simultaneous bone grafting done during implant placement.
| Antibiotics prescribed | Bone grafting procedures | |
|---|---|---|
| Implant placement without bone grafting | Implant placement with bone grafting | |
| Amoxicillin 500 mg | 447 (77.9%) | 17(3%) |
| Amoxicillin 500 mg + Flagyl 400 mg | 79 (13.8%) | 1 (0.2%) |
| Augmentin 625 mg | 26 (4.5%) | 0 |
| Augmentin 625 mg + Flagyl 400 mg | 4 (0.7%) | 0 |
| Pearson Chi square value | 2.33 | |
| P value for Chi square test | 0.506-not statistically significant | |
Table 3: Distribution of antibiotics in bone grafting procedure.
Amoxicillin 500 mg was prescribed for 17 patients (3%) and 1 patient (0.2%) was given a combination of amoxicillin 500 mg & Flagyl 400 mg. Chi square test showed no statistical significant relationship between antibiotics prescribed and bone grafting procedures with a p value of 0.506 (Figure 5).
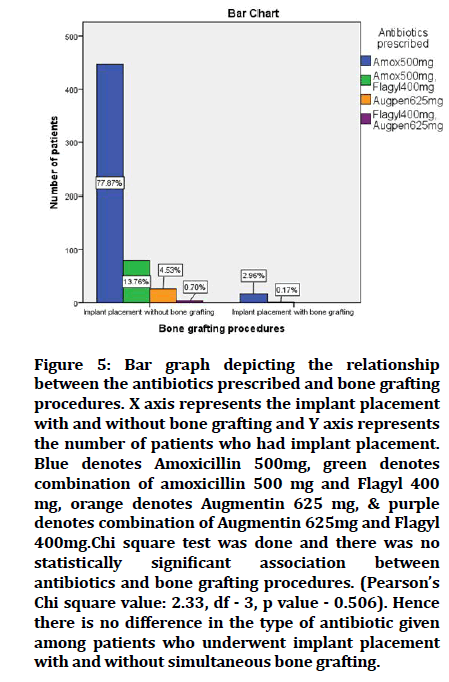
Figure 5: Bar graph depicting the relationship between the antibiotics prescribed and bone grafting procedures. X axis represents the implant placement with and without bone grafting and Y axis represents the number of patients who had implant placement. Blue denotes Amoxicillin 500mg, green denotes combination of amoxicillin 500 mg and Flagyl 400 mg, orange denotes Augmentin 625 mg, & purple denotes combination of Augmentin 625mg and Flagyl 400mg.Chi square test was done and there was no statistically significant association between antibiotics and bone grafting procedures. (Pearson’s Chi square value: 2.33, df - 3, p value - 0.506). Hence there is no difference in the type of antibiotic given among patients who underwent implant placement with and without simultaneous bone grafting.
Discussion
In the current study, the most common drug prescribed after implant placement was amoxicillin 500 mg. This is in accordance with Soung et al. where amoxicillin 500 mg was prescribed thrice daily for 5 days [33]. In the present study, for diabetic patients, the most common drug prescribed was amoxicillin 500 mg. This finding was opposed to the results of the study done by Turkyilmaz et al. in 2010, where the antibiotic regimen prescribed for type 2 diabetes patients was a combination of Amoxicillin & Potassium Clavulanate 500 mg twice daily for 5 days.
Dental implants have become one of the most common procedures practiced to replace missing teeth. There are several reasons for dental implant failure one of which is the development of bacteraemia around implants. In patients with periodontitis, due to exaggerated host immune response, the chances of development of bacteraemia is higher [34]. Most previous studies assessed the prophylactic antibiotic regimen for implant placement. A systematic review on “Antibiotic prophylaxis for Implant Surgery” by Esposito M et al, recommended amoxicillin 2 grams, 1 hour prior to surgery. Prophylactic antibiotics were prescribed for patients a) at high & moderate risk for endocarditis, b) patients with immunodeficiencies, c) metabolic diseases, d) patients irradiated in the head & neck region, e) when extensive or prolonged surgeries were anticipated. Prophylactic antibiotics proved to reduce post-operative complications & implant failures [35].
According to Arduino et al, high concentration - single dose antibiotic (amoxicillin 2 grams prior to surgery) was more favoured than 2 day postoperative course [36]. Whereas, Abdulwassie et al prescribed amoxicillin 500 mg thrice daily for 1 day prior to surgery, continued for 10 days after surgery [37]. In a retrospective study, 1 gram of phenoxymethyl penicillin was prescribed 1 hour before surgery as a prophylactic antibiotic, and 1 gram for every 8 hours after implant placement for 10 days. This group was compared with a group of patients who did not receive any antibiotics in terms of implant survival rates. There was no statistically significant difference between the two groups [38]. A double blinded randomized controlled trial was done by Lindeboom et al, to compare 2 grams penicillin pheneticillin versus 600 mg of clindamycin as a single dose in patients. No differences were observed between two groups in relation to postoperative infection. Single administration of antibiotics did not show any side effects [39].
Guided bone regeneration procedures are frequently done during implant placement. Delivery of growth factors from autologous platelet concentrates are considered as an adjunct to bone grafts during implant placements [40-43]. In the current study, amoxicillin 500 mg was the most commonly prescribed antibiotic for implant cases with simultaneously bone grafting procedures. In a study done by Froum et al, the most used antibiotic when bone regenerative procedure was done during implant placement was the penicillin family (69.5%), followed by doxycycline (24.2%). About 48% of the dentists prescribed antibiotics on the day of surgery, 3.1% of them prescribed several days after surgery, 18.4% 1 day before surgery and 30.6% after surgery [44].
Antibiotic resistance has become a serious threat globally. Dentists prescribe about 7- 11% of all common antibiotics including Beta Lactams, Clindamycin, macrolides, metronidazole and tetracyclines [45]. Dentists play an essential role in the appropriate usage of antibiotics, which is significant for providing good quality patient care, reducing the risk of adverse effects and narrowing down the chances of development of antibiotic resistant bacteria. Clinicians must think about the potential consequence of their choice of antibiotic prescription on both the individuals and the larger community. Each time an antibiotic is prescribed, there is an increased risk of antibiotic-resistance in both the patient and the entire community that come into contact with the patient. There are several fatal pathogens for which only few antibiotics are effective. Hence, treating the infections associated with these bacteria is more expensive and has a low success rate [46]. Apart from antibiotic resistance, overuse of antibiotics are also associated with some life threatening adverse effects like hepatotoxicity, allergic reactions, gastro intestinal, neurologic & psychiatric disorders [47]. Considering all these adverse effects of antibiotic overuse, dentists should assess the benefit versus risk ratio of antibiotic prescription, for all clinical circumstances before prescribing antibiotics.
Conclusion
According to this hospital based study, amoxicillin is still the most widely accepted and effective antibiotic used in implant therapy. A combination of amoxicillin and metronidazole is the second most preferred antibiotic regimen for various implant surgical procedures. Based on our study observations, there is no statistically significant relationship between the type of antibiotic prescribed and systemic status of the patients, single versus multiple implants & bone grafting procedures. However, further longitudinal studies have to be carried out to assess the duration of antibiotics prescribed following implant placement and its role in minimizing postoperative complications which might provide more definitive guidelines for the use of antibiotics in implant surgery.
Clinical Significance
Antibiotic resistance has become a serious threat globally. Dentists prescribe about 7- 11% of all common antibiotics. Thus determining the current trends in antibiotics prescription following dental implant placement is essential.
Acknowledgement
Nil.
References
- Karoussis IK, Kotsovilis S, Fourmousis I. A comprehensive and critical review of dental implant prognosis in periodontally compromised partially edentulous patients. Clin Oral Implants Res 2007; 18:669-679.
- Schou S. Implant treatment in periodontitis‐susceptible patients: A systematic review. J. Oral Rehabil 2008; 35:9-22.
- Thamaraiselvan M, Elavarasu S, Thangakumaran S, et al. Comparative clinical evaluation of coronally advanced flap with or without platelet rich fibrin membrane in the treatment of isolated gingival recession. J Indian Soc Periodontol 2015; 19:66.
- Ramesh A, Ravi S, Kaarthikeyan G. Comprehensive rehabilitation using dental implants in generalized aggressive periodontitis. J Indian Soc Periodontol 2017; 21:160.
- Kavarthapu A, Thamaraiselvan M. Assessing the variation in course and position of inferior alveolar nerve among south Indian population: A cone beam computed tomographic study. Indian J Dent Res 2018; 29:405.
- Esposito M, Hirsch JM, Lekholm U, et al. Biological factors contributing to failures of osseointegrated oral implants (I). Success criteria and epidemiology. Eur J Oral Sci 1998; 106:527-551.
- Mootha A, Malaiappan S, Jayakumar ND, et al. The effect of periodontitis on expression of interleukin-21: A systematic review. Int J Inflam 2016.
- Priyanka S, Kaarthikeyan G, Nadathur JD, et al. Detection of cytomegalovirus, epstein–barr virus, and torque teno virus in subgingival and atheromatous plaques of cardiac patients with chronic periodontitis. J Indian Soc Periodontol 2017; 21:456.
- Ramesh A, Varghese SS, Jayakumar ND, et al. Chronic obstructive pulmonary disease and periodontitis–unwinding their linking mechanisms. J Oral Biosci 2016; 58:23-26.
- Varghese SS, Thomas H, Jayakumar ND, et al. Estimation of salivary tumor necrosis factor-alpha in chronic and aggressive periodontitis patients. Contem Clin Dent 2015; 6:S152.
- Avinash K, Malaippan S, Dooraiswamy JN. Methods of isolation and characterization of stem cells from different regions of oral cavity using markers: A systematic review. Int J Stem Cells 2017; 10:12.
- Ramesh A, Vellayappan R, Ravi S, et al. Esthetic lip repositioning: A cosmetic approach for correction of gummy smile–A case series. J Indian Soc Periodontol 2019; 23:290.
- Ramamurthy JA, Mg V. Comparison of effect of hiora mouthwash versus chlorhexidine mouthwash in gingivitis patients: A clinical trial. Asian J Pharm Clin Res 2018; 11:84-88.
- Esposito M, Cannizzaro G, Bozzoli P, et al. Effectiveness of prophylactic antibiotics at placement of dental implants: A pragmatic multicentre placebo-controlled randomised clinical trial. Eur J Oral Implantol 2010; 3:135-43.
- Morris HF, Ochi S, Plezia R, et al. AICRG, Part III: The influence of antibiotic use on the survival of a new implant design. J Oral Implantol 2004; 30:144-151.
- Coulthard P, Esposito M, Jokstad A, et al. Interventions for replacing missing teeth: Surgical techniques for placing dental implants. Cochrane Database Systematic Rev 2003.
- Adell R. Tissue integrated prostheses in clinical dentistry. Int Dent J 1985; 35:259-265.
- Esposito M, Hirsch JM, Lekholm U, et al. Biological factors contributing to failures of osseointegrated oral implants (II). Etiopathogenesis. Eur J Oral Sci 1998; 106:721-764.
- Ahmad N, Saad N. Effects of antibiotics on dental implants: A review. J Clin Med Res 2012; 4:1.
- Chrcanovic BR, Kisch J, Albrektsson T, et al. Intake of proton pump inhibitors is associated with an increased risk of dental implant failure. Int J Oral Maxillofac Implants 2017; 32.
- Lund B, Hultin M, Tranaeus S, et al. Complex systematic review‐perioperative antibiotics in conjunction with dental implant placement. Clin Oral Implants Res 2015; 26:1-4.
- Flemmig TF, Beikler T. Decision making in implant dentistry: An evidence‐based and decision‐analysis approach. Periodontol 2009; 50:154-172.
- Anbu RT, Suresh V, Gounder R, et al. Comparison of the efficacy of three different bone regeneration materials: An animal study. Eur J Dent 2019; 13:022-8.
- Ashok V, Ganapathy D. A geometrical method to classify face forms. J Oral Biol Craniofac Res 2019; 9:232-5.
- Ganapathy DM, Kannan A, Venugopalan S. Effect of coated surfaces influencing screw loosening in implants: A systematic review and meta-analysis. World J Dent 2017; 8:496-502.
- Jain AR. Clinical and functional outcomes of implant prostheses in fibula free flaps. World J Dent 2017; 8:171-6.
- Jain AR, Nallaswamy D, Ariga P, et al. Determination of correlation of width of maxillary anterior teeth using extraoral and intraoral factors in Indian population: A systematic review. World J Dent 2018; 9:68-75.
- Ranganathan H, Ganapathy DM, Jain AR. Cervical and incisal marginal discrepancy in ceramic laminate veneering materials: A SEM analysis. Contemp Clin Dent 2017; 8:272.
- Jain AR. Prevalence of partial edentulousness and treatment needs in rural population of South India. World J Dent 2017; 8:213-217.
- Duraisamy R, Krishnan CS, Ramasubramanian H, et al. Compatibility of nonoriginal abutments with implants: Evaluation of microgap at the implant–abutment interface, with original and nonoriginal abutments. Implant Dent 2019; 28:289-295.
- Gupta P, Ariga P, Deogade SC. Effect of monopoly-coating agent on the surface roughness of a tissue conditioner subjected to cleansing and disinfection: A Contact Profilometric In vitro study. Contemp Clin Dent 2018; 9:S122.
- Varghese SS, Ramesh A, Veeraiyan DN. Blended Module‐Based Teaching in Biostatistics and Research Methodology: A Retrospective Study with Postgraduate Dental Students. J. Dent. Educ.. 2019;83:445-50.
- Deeb GR, Soung GY, Best AM, et al. Antibiotic prescribing habits of oral and maxillofacial surgeons in conjunction with routine dental implant placement. J Oral Maxillofac Surg 2015; 73:1926-9131.
- Ramesh A, Varghese SS, Doraiswamy JN, et al. Herbs as an antioxidant arsenal for periodontal diseases. J Intercult Ethnopharmacol 2016; 5:92.
- Esposito M, Grusovin MG, Willings M, et al. The effectiveness of immediate, early, and conventional loading of dental implants: A cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants 2007; 22.
- Arduino PG, Tirone F, Schiorlin E, et al. Single preoperative dose of prophylactic amoxicillin versus a 2-day postoperative course in dental implant surgery: A two-centre randomised controlled trial. Eur J Oral Implantol 2015; 8:143-9.
- Abdulwassie H, Dhanrajani PJ. Diabetes mellitus and dental implants: a clinical study. Implant Dent 2002; 11:83-6.
- Gynther GW, Köndell PÅ, Moberg LE, et al. Dental implant installation without antibiotic prophylaxis. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 1998; 85:509-11.
- Lindeboom JA, Tuk JG, Kroon FH, et al. A randomized prospective controlled trial of antibiotic prophylaxis in intraoral bone grafting procedures: single-dose clindamycin versus 24-hour clindamycin prophylaxis. Mund-, Kiefer-und Gesichtschirurgie. 2005; 9:384-8.
- Panda S, Jayakumar ND, Sankari M, et al. Platelet rich fibrin and xenograft in treatment of intrabony defect. Contemp Clin Dent 2014; 5:550.
- Ravi S, Malaiappan S, Varghese S, et al. Additive effect of plasma rich in growth factors with guided tissue regeneration in treatment of intrabony defects in patients with chronic periodontitis: A split‐mouth randomized controlled clinical trial. J Periodontol 2017; 88:839-45.
- Khalid W, Vargheese SS, Lakshmanan R, et al. Role of endothelin-1 in periodontal diseases: A structured review. Indian J Dent Res 2016; 27:323.
- Khalid W, Varghese SS, Sankari M, et al. Comparison of serum levels of endothelin-1 in chronic periodontitis patients before and after treatment. J Clin Diagnost Res 2017; 11:ZC78.
- Froum SJ, Weinberg MA. An evaluation of antibiotic use in periodontal and implant practices. Int J Periodontics Restorative Dent 2015; 35.
- Giubilini A. Antimicrobial resistance and antimicrobial stewardship programmes: Benefiting the patient or the population?. J Med Ethics 2017; 43:653-654.
- Centers for Disease Control and Prevention. Antibiotic resistance threats in the United States, 2019. US Department of Health and Human Services, Centres for Disease Control and Prevention 2019.
- Lode H. Safety and tolerability of commonly prescribed oral antibiotics for the treatment of respiratory tract infections. Am J Med 2010; 123:S26-38.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Subasree Soundarajan and Priya lochana Gajendran*
Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University, Chennai, Tamil Nadu, IndiaCitation: Subasree Soundarajan, Priya lochana Gajendran, Current Trends in Antibiotics Prescription Following Dental Implant Placement: A Hospital Based Assessment, J Res Med Dent Sci, 2022, 10(1): 454-460
Received: 19-Dec-2021, Manuscript No. JRMDS-22-50241; , Pre QC No. JRMDS-22-50241 (PQ); Editor assigned: 21-Dec-2021, Pre QC No. JRMDS-22-50241 (PQ); Reviewed: 04-Jan-2022, QC No. JRMDS-22-50241; Revised: 07-Jan-2022, Manuscript No. JRMDS-22-50241 (R); Published: 14-Jan-2022
