Research - (2022) Volume 10, Issue 9
Cytokine Storm Assessment in Initial Stages ofCOVID-19 Along with Recent Emerging Therapeutic Modalities
Rohan Somani and Sonali Choudhary*
*Correspondence: Sonali Choudhary, Department of Community Medicine, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi (Meghe), Wardha, Maharashtra, India, Email:
Abstract
The recently spreading SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) causing coronavirus disease 2019 (COVID-19) pandemic put the practice of medicine at verge of overlooking a new & different era. Still the world is struggling to minimize the spread of this devastating disease; several strategies are actively deployed to develop therapeutic interventions to prevent the surge. This pandemic is reminding us of the crucial role of effective host immune response and also the life-threatening effect of disturbed immune regulation. There is a budding concept of covid-19 cytokine release syndrome (COVID-19 CRS), also known as cytokine storm (CS). These patients are critically ill and has worse prognosis with increased fatality rate. Cytokine storm is believed to be the at most reason of pathophysiology of many lethal manifestations of COVID-19 such as acute respiratory distress syndrome (ARDS), thromboembolism diseases like acute ischemic stroke caused by big vessels obstruction and myocardial ischemia, acute renal injury (AKI), encephalitis, and vasculitis (“Kawasaki-like” syndrome and “renal vasculitis” in children and adults respectively). So, to unravel the pathogenesis and risk factor of CS, this review article provides critical understanding from prognostic, therapeutic and diagnostic standpoint and reviews the phenomena of mechanism and to study various treatment modalities of the COVID-19 virus causing inflammatory storm in a way to give valuable medical knowledge for research and clinical cure.
Keywords
COVID-19, Cytokine storm, Immuno-dysregulation, Thromboembolism, Treatment strategies, ARDS
Introduction
In December 2019, a mass outbreak of cases of pneumonia seen in Wuhan, a place in China. A new virus called novel-CoV 2019 (n-CoV) was first isolated in 7th January 2020 and marked as cause of this outbreak. Soon, it spreads rapidly across whole China and then to other countries resulting in a global outbreak. Since then, WHO named this pandemic as COVID-19 (coronavirus 2019) disease? The mean incubation period is 5-6 days. More than 50% patients are asymptomatic or with mild symptoms of fever, cough, loss of taste and loss of smell, etc. But further research says that severity of COVID-19 disease is linked with marked high level of inflammatory mediators which includes chemokine’s, cytokines such as IL6, IL2, IL7, IL8, IL9, IL10 , TNF-alpha, granulocyte colony stimulating factors (G-CSF), GM-CSF, Interferon gamma, monocytes chemo attractant protein – 1 (mcp- 1), macrophages inflammatory protein 1-alpha ( mip- 1alpha) , CXC chemokine ligand 10 (CXCL-10), CRP, plasma ferritin, IP-10, MIP-1beta and D-dimer in blood [1]. Among all these, high levels of IL-6 in blood is highly associated with disease severity. A case study of 82 survivors and 68 non survivors of COVID –19 is done with high levels of IL-6 marker in their blood samples and their prognosis in compared to those of having COVID-19 with normal blood picture [2].
Cytokine storm also known as Cytokine Release Syndrome (CRS) is characterized by clinical presentation of enormous systemic inflammations, hyper-ferritenemia, and hemo-dynamic instability and if left untreated will lead to death in all cases. Several biological agents targeting cytokines like IL-1 receptors antagonists (ANAKINRA) also used in RA (rheumatoid arthritis), TOCILIZUMAB (a recombinant IL-6 receptors antagonists interferes in IL-6 binging and blocks further signaling) have been also proven of great value in treatment of CS caused by CAR-T cell therapy, downstream inhibitors of cytokine like JAK inhibitors are also under exploration.
Objective
The main objectives of this review article is critical evaluation of existing methodological approach and unique insights of cytokine release syndrome in COVID-19 and develop conceptual frameworks on early intervention to prevent mortality in this widespread global pandemic and to fill existing gaps and future research directions in COVID-19 and CRS field.
Results and Discussion
The phrase "cytokine storm" refers to a group of immune dysregulation illnesses marked by systemic inflammation, constitutional symptoms and multiple organ system dysregulation, which can progress to multiple organ failure if not treated properly. Depending on the etiology and treatment used, the onset and time span of cytokine storm changes [3].
Unlike early-stage clinical indications of cytokine storm, late-stages manifestations of cytokine storm are similar and frequently overlay. Patient with cytokine storm is mostly febrile, and in extreme case, the fever is usually high. In addition, patients also experienced fatigue, anorexia, migraine, rashes, diarrhea, arthralgia and various neuropsychiatric findings. These signs and symptoms are caused by cytokine-mediated tissue damage or acute-phase changes, or they could be the outcome of immune-cell-mediated responses. Disseminated intravascular coagulation can develop quickly, resulting in arterial obstruction or multiple haemorrhage, dyspnea, hypoxemia, low blood pressure, hemostatic disturbance, shock, and mortality. A lot of patients experience respiratory symptom such as cough, fever and tachypnea, which can cause acute respiratory distress syndrome (ARDS) and hypoxemia, which may need the use of mechanical ventilation. Patients with cytokine storm are at increased risk of spontaneous bleeding due to a combination of hyper-inflammation, coagulopathy, and low platelet counts [4].
Renal failure, abrupt liver damage or cholestasis, and a stress causing cardiomyopathy can all occur in morbid cases of cytokine storm. Capillary leak syndrome and anasarca can result from a combination of renal dysfunction, endothelial cell injury, and acute phase of hypoalbuminemia, alterations that are comparable to those seen in cancer patients treated with large doses of interleukin-2. Immune effector cell–leading neurotoxic syndrome or cytokines release syndrome– causing encephalopathy are terms used to describe the neurologic side effects of T-cell immunotherapy. The neurotoxic consequences of the cytokine storm are frequently delayed, appearing few days after the commencement of the cytokine storm [5].
Risk Factors for development of cytokine storm in COVID-19: Male gender, lactate dehydrogenase level, age above 40 years, positive test result for replicative SARSCoV-2 RNA, absolute lymphocyte count, D-dimer and ferritin levels, dynamics in the NEWS score, and plasma IL-6 concentration are the basic risk factors for cytokine storms in COVID-19 patients. Few hereditary diseases, such as familial hemophagocytic lymphohistiocytosis (HLH), are predisposed to cytokine storm in response to infections, typically within the first few months of life [6]. The cytokine storm caused by the influenza A virus is one of the most widely researched forms (the virus that causes the common flu). Infections with more severe strains of influenza may be more likely to result in a cytokine storm. Still's disease, systemic juvenile idiopathic arthritis (JIA), and lupus are all examples of autoimmune diseases usually progressing to cytokine storm. The term "macrophage activation syndrome" is often used to describe cytokine storm in these scenarios [7].
Cytokine storm can also occur as a result of some medical treatments. For example, it has developed after CAR-T immunotherapy (chimeric antigen receptor T cells) for leukemia. Cytokine storm can also happen in other medical conditions, such as following a stem cell or organ transplant. Cytokine storm syndrome can be caused by certain types of malignancies, as in immunesystem disorder such as AIDS. Sepsis, a life-threatening immunological reaction to infection, and is sometimes referred to as a form of cytokine storm syndrome [8].
Role of cytokine storm in pathogenesis and in further progression of COVID-19 pneumonia: Inflammation is a combination of physiological processes in which multicellular organisms have evolved to control invading infections and repair damage by activating innate and adaptive immune response. The immune system should be able to detect foreign attackers, respond appropriately, and then turn back to homeostasis. This reaction necessitates striking a balance between producing enough cytokines to kill the pathogen while avoiding a hyper inflammatory response, in which an excess of cytokine produces most significant damages. Excess immune activation in cytokine storm can be caused by incorrect triggering or threat perception, with a response beginning in absent of a pathogen. A cytokine storm is an immunological state marked by rapid activation and proliferation of T cell, macrophage, and natural killer cell, and the production of as much as 150 inflammatory cytokines along with chemicals mediators formed by both immune and non-immune cells [9]. These abnormal leaks of pro-inflammatory factors in viral infections cause lung epithelial and endothelial cells death, causing disruption to the lung microvascular and epithelial alveolar cell barrier, resulting in microvascular leak, alveolar oedema, and hypoxia. Various manifestations of cytokine storm in COVID-19 pneumonia are seen in Figure 1.
Immunopathology
Lymphopenia: Lymphopenia was prevalent in COVID-19 sufferer, and it was founded to be directly linked with the severity of the condition. COVID-19 patients had lower numbers and percentage of lymphocytes, including CD4 + T cell , CD8 + cytotoxics cell, natural killers (NK) cells, and B cell, according to laboratory findings [10]. The participation of lymphopenia was validated to the greatest extent possible using single-cell sequencing and flow cytometry.
Antibody-dependent enhancement
In COVID-19 infections, B cells are probably protective because they produce neutralizing antibodies against the ACE2 receptor, which block viral entrance [11]. However, depending on the viruses elements targeted and the antibody's Fc region, neutralizing antibodies generated by B cells are not always protective. Antibody dependent enhancement is a phenomenon in which preexisting neutralizing antibodies target only one serotype of virus and increase the arrival of that virus with also another viral serotypes into leucocytes by interacting with Fc binding receptors and complement activation receptors on these cells. These antibodies against viral spike (S) glycoprotein mediate virus uptake via Fc receptors into immune cells such as B cells, monocytes and macrophages. Antibody dependent enhancement is being observed in a variety of viral infections such as Dengue virus, HIV, Influenza virus, Respiratory syncytial virus and Ebola virus along with recent SARSCoronavirus family (Figure 1) [12].
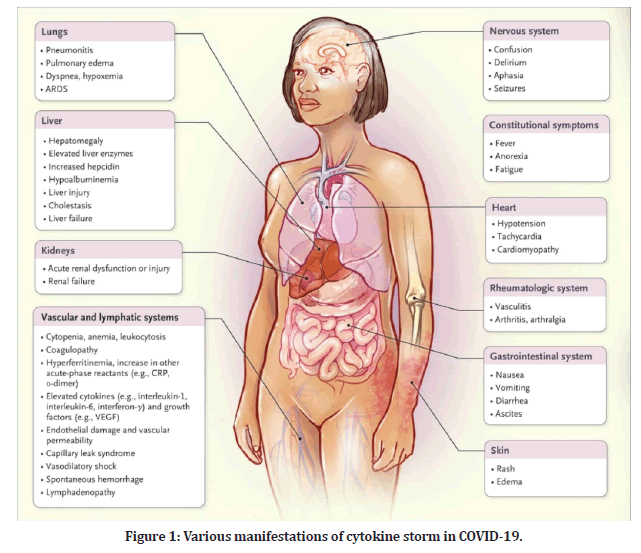
Figure 1: Various manifestations of cytokine storm in COVID-19.
Neutrophils
The presence of a marked raised in neutrophils count in SARS-CoV infected sufferers is well known. The neutrophils protect against infections under normal circumstances by generating neutrophil extracellular traps (NETs) that kill pathogens extracellularly; nonetheless, excessive neutrophils activations can harm nearby cells and causes cascade of unfavorable reactions like antibody production against host DNA (autoimmunization), disintegrate connective tissues, and can cause thromboembolic events [13].
Cell types that are mostly involved in cytokine storm: The innate of immune system's cells are the body's first line of defense against all invading pathogens whether it is bacteria, viruses or parasites. Few examples are enzymes in tears and saliva, cough reflex, skin, gastric acid. Viruses are recognized by neutrophils, monocytes, and macrophages, which generate cytokines and phagocytose viruses and cells.
T effector cells: B cells and T cells constitute the adaptive immune system. T-cells differentiate into several sub sets, each with specific effector-cell capabilities that could be involved in cytokine storm. The host response against viral infections is predominantly mediated by type 1 helpers T (Th1) cells and cytotoxic T lymphocytes (CTLs). An increased Th1-type inflammatory response is commonly seen in cytokine storm. After the virus enter into human’s body, the Th1 cells release a lot of interferon, causing delayed type 4 hypersensitivity reactions, thus, they are crucial for intracellular pathogen defense. The capacity of charged T cells to start a cytokines storm has been linked to iatrogenic etiology of cytokine storm including massive T-cell activation. Impaired granules related killing of infected cells by cytotoxic T lymphocytes is seen in some types of cytokine storm which triggers Macrophage activating system (MAS) [14] as shown in Figure 2.
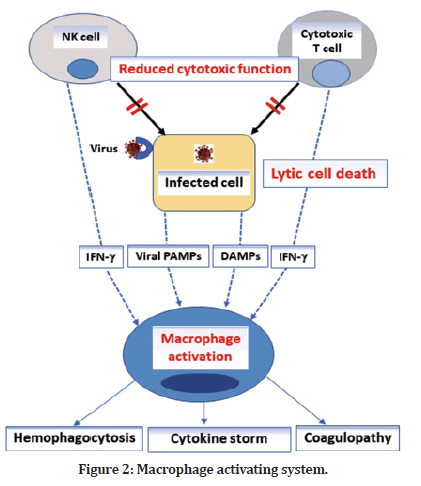
Figure 2: Macrophage activating system.
Cytokines in Cytokine Storm
IL-6: Interleukin-6 (IL-6) is a multi-acting cytokine that regulates everything from hematopoiesis and metabolism to inflammation, autoimmune, and the acute phase response. IL-6 involves in control of monocyte and their development into macrophage, enhances B cells to IgG production [15], and encouragement of Th2 response by blocking Th1 polarization. Several investigations showed the correlation between serum IL-6 level and onset of respiratory failure. Even mild rise of IL-6 levels over 80 pg/mL were found to be enough for identifying covid-19 infected sufferers at high risk of going into respiratory arrest. Furthermore, detectable SARS-CoV-2 nucleic acid in blood , is tightly linked to extraordinarily high IL-6 plasma levels. It was also hypothesized that orderly measurements of circulating IL-6 could be useful in detecting progression of COVID-19 or, if done soon after a COVID-19 diagnosis, could forecast a respiratory failure [16].
TNF: Tumor necrotic factor (TNF) is a pro-inflammatory cytokine with several properties that consists to the TNF– TNF receptor super families. TNF alpha can cause cellular death and control immunity in addition to producing fevers, increasing systemic infection, and signal anti-pathogenic actions like IL-6. TNF along with other TNF– TNF receptor super families are powerful NF-B inducing agents, resulting in the production of several proinflammatory genes. TNF-alpha is the cytokine that causes the super-antigens driven cytokine storm in experimental mouse models of toxic shock [17]. The efficacy of anti-TNF medicines in some autoinflammatory- driven cytokine storm circumstances suggests that these anti -TNF medicines may have a role in cytokine storm treatment.
IL-18: Interleukin-18 (IL-18) is a representative of the vast IL-1 pedigree, which is being linked to cytokine storm syndromes in recent years. Inflammasomes (inflammatory caspases) activates interleukin-18 and interleukin-1 from their precursors by recognizing pathogenic microbes and sterile stimuli and activates caspase-1 during pyroptosis, causing the dormant precursor versions of interleukin-1 and interleukin-18 to become active [18]. The principal sources of bioactive interleukin-18, which has a number of pro-inflammatory effects, are macrophages and dendritic cells. Most importantly; it enhances Th1-type inflammatory responses by synergizing with IL-12 or IL-15 to increase interferon-secretion from T cells. The interleukin-18 receptor are present on NK cells most of the time and is upregulated in most T cells when they are activated. IL-18 is also powerful inducer of interleukin-6 (IL-6) production in macrophages, like IL-1 [18].
Chemokines: Chemokines are a type of cytokine that helps immune cells perform a number of tasks, including leukocyte recruitment and trafficking. Hyperinflammation may be caused by dysregulated trafficking during inflammation. Several cytokines, such as IL-10 and IL-1 receptor antagonists , act as buffers to minimize systemic effects that are off-target. TNF, IL-1, IL-6, and IL- 12 are all inhibited by IL-10, which also inhibits antigen presentation. In addition, infection causes a cytokine storm in mice missing IL-10. Ana-kinra is a remedial drug that copies the immunomodulatory effects of IL- 1RA [19].
Remedial techniques to target cytokine storm in COVID-19
Immunoremedial techniques in COVID-19 pneumonia: Being a doctor, we have to pay our attention to the effects of immunological inflammatory factor release has on SARS-CoV-2 infected sufferers, and numerous acting cytokines blockers and diagnostic techniques is reported. There is a 5–7-day gap between the diagnosis of COVID-19 pneumonia and the beginning of multiple organ dysfunction syndromes (MODS) in the clinical phase. After this time period, large number of patients (about 80%) shows improvement , but about 20% of them develop severe pneumonia, with a 2% death rate [20].To improve the prognosis, patients should be given immunotherapy when they are diagnosed, to prevent a cytokine storm later on and to minimize mortality in the most severe cases.
Cytokine based interventions
IFN-I: Recombinant Interferon-1 (IFN-1) is being actively trialled in COVID-19 patients. It has been studied in the past for treating both Severe acute respiratory syndrome (SARS), Middle east respiratory syndrome (MERS). Type 1 interferon (IFN-1, IFN-a and IFN-B) functions in both paracrine and autocrine manners to induce the expression of various interferon-stimulated genes (ISGs) that provides antiviral activities to host cell [21]. In vitro and in some animal derived models, it was found to be relatively effective, however human studies were inconclusive.
Targeting interleukins: Since Interleukin-6 (IL-6) is crucial in cytokine storm pathology; another potential therapeutic technique is to block IL-6 [22]. Tocilizumab (monoclonal antibodies) can inhibit the IL-6 receptors (IL-6-R) that sticks to both membranes-bound IL-6R and soluble IL-6R, blocking IL-6 signaling downstream of gp130 binding [23].
Severe clinical symptoms such as difficulty in breathing or shortness of breath improved after Tocilizumab treatment in 138 COVID-19 patients, according to a study [24]. Tocilizumab right now is in phase IV clinical studies (ChiCTTR2000029765) and is also being approved in China. Tocilizumab is being tested in COVID-19 patients (TO-CIVID-19) by the Italian Regulator Drugs Agencies in phase II trial [24]. The trans-signaling pathway involving sIL-6R is involved in IL-6's pro-inflammatory actions. The cis signaling pathway involving the mIL- 6R, which is found on macrophage, neutrophil, few T lymphocyte, and hepatocyte, is involved in IL-6's antiinflammatory and regenerative actions. Tocilizumab is non-selective for the soluble IL-6R and may also block the membrane-bound IL-6R, resulting in undesirable side effects like, cytopenia, particularly neutropenia and thrombocytopenia. COVID-19 hypercytokinaemia may be treated with IL-1 inhibitors as an option. Anakinra showed a survival benefit in few COVID-19 patients during its phase III clinical trial with no additional side effects. Because they decrease the pro inflammatory actions of certain interleukins (1/37/38) could be considered as treatment possibilities for COVID-19.
JK/STAT signaling pathway Inhibitors: SARS CoV-2 invades into host cell through receptors mediating endocytosis, which is controlled by Numb-associated kinases (NKA) like adaptor complex protein 2 (AP2)- associated protein kinase (AAK1) and G-associated kinase (GAK). Ruxolitinib, a high affinity AAK1 blocker, is going to be studied for a treatment of COVID-19 (ChiCTTR2000029580). To inhibit NAK, lethal dosages of AAK1 inhibitors are necessary. Baricetinib can act by inhibiting both GAK and AAK1 (at a dose of 2-6 mg per day), as well as JAK 1 and 2, minimizes the IL-6 inflammatory effects via the JK-STAT signaling pathway. Due to its ability of low plasma protein binding, baricetinib can be used in mixture antivirals and antiinflammatory therapy [25]. Early results in COVID-19 patients reveal that baricetinib coupled with antiviral therapy has promise. The combined immunopathology in COVID-19 infection is clubbed and presented in the following Figure 3.
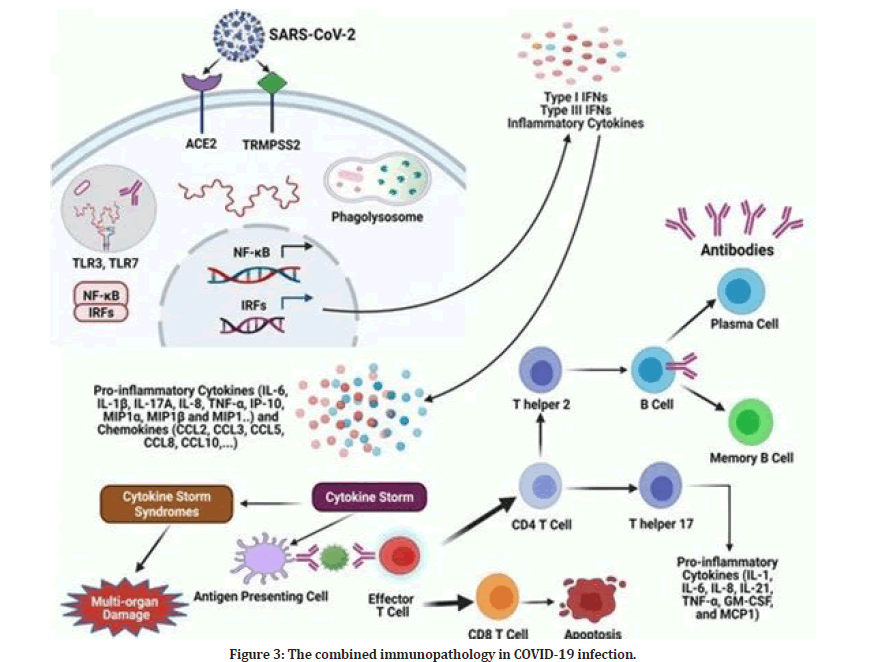
Figure 3: The combined immunopathology in COVID-19 infection.
Role of High Dose Corticosteroid pulse therapy and Low Dose Corticosteroid therapy in Cytokine Storm: Anti-inflammatory agents, such as corticosteroids, can be utilized to minimize the lung damage caused by the cytokine storm in COVID-19 patients. Dexamethasone, a recombinant corticosteroid, is a broad-spectrum immunosuppressant with higher activity and a longer half-life than cortisone. It has a variety of mechanisms of action, and as a result, it can influence a variety of body systems. Because of their capacity to reduce gene transcription of various pro-inflammatory cytokines, chemokine’s, and integrin’s, corticosteroids like dexamethasone have anti-inflammatory potential [26]. Because of its capacity to decrease the production of cytokines and minimize their harmful effects, dexamethasone may be useful in patients with COVID-19. As a result, it may be effective in combating the COVID- 19-related cytokine storm. In individuals with COVID-19 who develop pneumonia, short-term dexamethasone administration has shown to lower the intensity of inflammation by suppressing the severe cytokine storm or hyper inflammatory phase [27].
Dexamethasone however, is a broad-spectrum immunosuppressant that can also inhibit B cell-mediated antibody formation, diminish T cell protective function, and limit macrophage-mediated apoptotic cell clearance. This can lead to increased viral load with in plasma and a higher risk of subsequent infections. The effectiveness of corticosteroid therapy in the treatment of viral respiratory infections is dependent on the dose, the time of administration, and the patient type. Corticosteroids in high doses may be detrimental. As a result, we might presume that glucocorticoids' immunomodulatory effects are only advantageous in the later, hyper inflammatory stages of the disease. A pulse dose of intravenous dexamethasone, followed by nebulized triamcinolone (another corticosteroid) to concentrate the effects in the lungs alone, is a safer technique [28]. Simultaneous administration of intravenous immunoglobulins and interferon-beta is another technique for reducing the side effects of corticosteroid treatment. The therapeutic potential of dexamethasone provided in association with intravenous immunoglobulin and interferon-beta was examined in a multicenter randomized control trial (Identifier: IRCT20120225009124N4) conducted from April 18, 2020 to June 19, 2020 [29]. The trial's findings are likely to be released soon.
Alternative therapy techniques with cytokine induced storm
Stem Cells Therapy: Mesenchymal stem cells (MSCs) are stromal cells that have the ability to self-renew and also exhibit multiline age differentiation. MSCs also have antiinflammatory and immunological regulator functions in addition to self-renewing and differentiation, since they decrease the release of pro inflammatory cytokines. MSC can also secrete IL -10, keratinocytes and hepatocyte growth factors , Vascular Endothelial Growth Factor (VEGF), which work together to prevent fibrosis and heal injured lung tissues [30]. Therefore, MSC appears to be a viable therapy option for cytokine storm.
The fabricated liver technology
One more interesting therapy available is purification of blood products via procedures such as large volume plasma exchanging and plasma filtrations, which can significantly decrease the inflammation by removing inflammatory components and thereby limiting the production of cytokines causing cytokine storms in COVID-19 sufferers [31].
Chloroquine: The cytokine storm in COVID-19 patients is considered to be suppressed by Chloroquine, which inhibits the synthesis of inflammatory mediator including TNFs and IL-6. Chloroquine phosphate is being utilized successfully in the therapy of various covid-19 patients with undeniably varying success rates in China [32], based on early favorable results. “Hydroxycholoroquine is used in autoimmune diseases like systemic lupus erythematosus and rheumatoid arthritis, and shown to have antiviral effect in laboratory conditions. But the COVID-19 treatment guidelines panel recommends against the use of Chloroquine and Hydroxycholoroquine and azithromycin for treatment of COVID-19 in hospitalized patients (AI) and in nonhospitalized patients (AIIa).
Continuous renal replacement therapy
Continous renal replacement therapy (CRRT) can help critically sick patients with renal/circulatory problem due to COVID-19 by extracting various potentially toxic components and together maintain their hemodynamic and metabolically profile.
Conclusion
COVID-19 is giving rise to tremendous challenges in entire world and efforts are made to better understand the pathogenesis of COVID-19 especially with cytokine storm which is a lethal condition and ultimately lends a patient into ARDS, MODS, multiple coagulopathy across various organs. Serum plasma ferritin and IL-6 are most useful and fatal biomarker of cytokine storm for the patients with COVID-19. Since IL-6 played a determining role in disease severity, Tocilizumab becomes a good therapeutic option. Nowadays future researches are directing towards the special molecules that can regulate IL-6 amplification in fatal covid-19 disease. So, we know by now that cytokine storm is causing ARDS and MODS, which ultimately leads to physical deterioration and mortality. Timely management of cytokine storm in early stages by various immunomodulators and interleukin antagonists and cytokine inhibitors, anti-inflammatory drugs for reducing lung inflammatory cell infiltration, is the only key to reduce mortality and widening the treatment success rates in patients with COVID-19.
Seeing the undying hard work and concerned efforts of our scientific teams across whole world in field of an umbrella term called “Cytokine Storm”, we are soon expecting to see good results out of this fatal condition and with very less or negligible mortalities of our loved ones.
References
- Chein JY, Hsueh PR, Cheng WC, et al. Temporal changes in cytokine/chemokine profiles and pulmonary involve syndrome. Respirology 2006; 11715â??722.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020; 395:1054â??1062.
- Lee DW, Santomasso BD, Locke FL, et al. ASTCT consensus grading for cytokine release syndrome and neurologic toxicity associated with immune effector cells. Biol Blood Marrow Transplant 2019; 25:625-638.
- Asakura H, Ogawa H. COVID-19-associated coagulopathy and disseminated intravascular coagulation. Int J Hematol 2021; 113:45-57.
- Lee DW, Santomasso BD, Locke FL, et al. ASTCT consensus grading for cytokine release syndrome and neurologic toxicity associated with immune effector cells. Biol Blood Marrow Transplant 2019; 25:625-638.
- Sieni E, Cetica V, Hackmann Y, et al. Familial hemophagocytic lymphohistiocytosis: When rare diseases shed light on immune system functioning. Front Immunol 2014; 5:167.
- Schulert GS, Grom AA. Pathogenesis of macrophage activation syndrome and potential for cytokine- directed therapies. Annu Rev Med 2015; 66:145â??159.
- Behrens EM, Koretzky GA. Cytokine storm syndrome: Looking toward the precision medicine era. Arthritis Rheumatol 2017; 69:1135-1143.
- Teijaro JR, Walsh KB, Rice S, et al. Mapping the innate signaling cascade essential for cytokine storm during influenza virus infection. Natl Acad Sci  2014; 111:3799â??3804.
- Zhang JJ, Dong X, Cao YY, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 2020; 75:1730-1741.
- Nielsen SC, Yang F, Jackson KJ, et al. Human B cell clonal expansion and convergent antibody responses to SARS-CoV-2. Cell Host Microbe 2020; 28:516-525.
- Taylor A, Foo SS, Bruzzone R, et al. Fc receptors in antibody-dependent enhancement of viral infections. Immunol Rev 2015; 268:340â??364.
- Thierry AR, Roch B. SARS-CoV2 may evade innate immune response, causing uncontrolled neutrophil extracellular traps formation and multi-organ failure. Clin Sci 2020; 134:1295â??1300.
- Crayne CB, Albeituni S, Nichols KE, et al. The immunology of macrophage activation syndrome. Front Immunol 2019; 10:119.
- Chomarat P, Banchereau J, Davoust J, et al. IL-6 switches the differ-entiation of monocytes from dendritic cells to macrophages. Nat Immunol 2000; 1:510â??514.
- Herold T, Jurinovic V, Arnreich C, et al. Level of IL-6 predicts respiratory failure in hospitalized symptomatic COVID-19 patients. Medrxiv 2020;
- Faulkner L, Cooper A, Fantino C, et al. The mechanism of superantigen-mediated toxic shock: not a simple Th1 cytokine storm. J Immunol 2005; 175:6870-6877.
- Rhen T, Cidlowski JA. Antiinflammatory action of glucocorticoids--new mechanisms for old drugs. New Engl J Med 2005; 353:1711â??1723.
- Iqbal Yatoo M, Hamid Z, Rather I, et al. Immunotherapies and immunomodulatory approaches in clinical trials: A mini review. Human Vaccines Immunotherap 2021; 17:1897-1909.
- Selvaraj V, Dapaah-Afriyie K, Finn A. Short-term dexamethasone in sars-CoV-2 patients. R. I. Med. J. 2020;103(6):39â??43.
- Theoharides TC, Conti P. Dexamethasone for COVID-19? Not so fast. J Biol Regul Homeost Agents 2020; 34:1â??5.
- Abdolahi N, Kaheh E, Golsha R. Letter to the editor: Efficacy of different methods of combination regimen administrations including dexamethasone, intravenous immunoglobulin, and interferon-beta to treat critically ill COVID-19 patients: A structured summary of a study protocol for a randomized controlled trial. Trials 2020; 21:549.
- Frank D, Vince JE. Pyroptosis versus necroptosis: Similarities, differences and crosstalk. Cell Death Differ 2019; 26:99-114.
- Wang D, B Hu, C. Hu, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020; 323:1061-1069.
- Blanco-Melo, D. et al. Imbalanced host response to SARS-CoV-2 drives development of COVID-19. Cell. 2020;181:1036â??1045.
- Gabay C. Interleukin-6 and chronic inflammation. Arthritis Res Ther 2006; 8:S3.
- Zhang C, Wu Z, Li JW, et al. The cytokine release syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the key to reduce the mortality. Int J Antimicrob Agents 2020; 55:105954.
- Xu X, Han M, Li T, et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci USA 2020; 117:10970.
- Stebbing J, Phelan A, Griffin I, et al. COVID-19: Combining antiviral and anti-inflammatory treatments. Lancet Infect Dis 2020; 20:400â??402.
- Lee J, Fang X, Krasnodembskaya A, et al. Concise review: Mesenchymal stem cells for acute lung injury: Role of paracrine soluble factors. Stem Cells 2011; 29:913â??919.
- Zuccari S, Damiani E, Domizi R, et al. Changes in cytokines, haemodynamics and microcirculation in patients with sepsis/septic shock undergoing continuous renal replacement therapy and blood purification with CytoSorb. Blood Purification 2020; 49:107â??113.
- Gao J, Tian Z, X Yang. Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies. Bioscience Trends 2020; 14:72-73.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Rohan Somani and Sonali Choudhary*
Department of Community Medicine, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi (Meghe), Wardha, Maharashtra, IndiaReceived: 29-Aug-2022, Manuscript No. jrmds-22-70752; , Pre QC No. jrmds-22-70752(PQ); Editor assigned: 30-Aug-2022, Pre QC No. jrmds-22-70752(PQ); Reviewed: 13-Sep-2022, QC No. jrmds-22-70752(Q); Revised: 16-Sep-2022, Manuscript No. jrmds-22-70752(R); Published: 23-Sep-2022
